The complex and specialized anatomical regions of the face merit consideration because they have significant influence on facial appearance. The need for many secondary soft tissue procedures in these areas can be obviated by skillful primary surgery. In this chapter, special attention is given to injuries of the scalp, forehead, brow, eyelid, nose, lips, ear, and important deeper structures such as the facial nerve, the lacrimal gland, and the parotid duct.
Initial care of soft tissue injuries should be undertaken as described in Chapter 6 , and the following discussion assumes that these principles have been followed:
- •
Primary Advanced Trauma Life Support (ATLS) care
- •
Control of hemorrhage
- •
Early intervention for soft tissue injuries
- •
Careful evaluation of damage to nerves, ducts, and blood vessels
- •
Careful evaluation of any ocular injuries
- •
Identification of foreign bodies
- •
Clinical and radiological examinations to exclude bone fractures
Scalp and Forehead
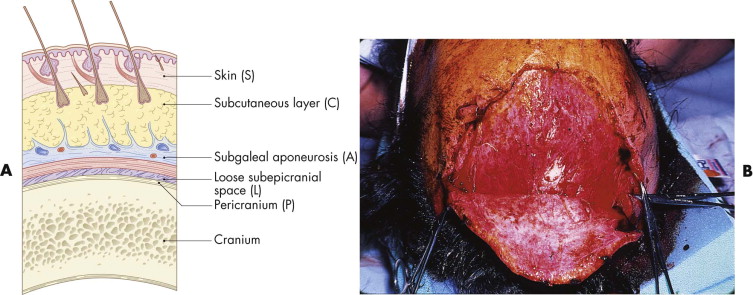
The scalp, with its well-defined five layers, represents a single anatomical unit that, including the forehead, extends from the supraorbital margins anteriorly to the superior nuchal line posteriorly. The musculoaponeurotic galea provides a source of vascular perforators to the skin, and its fibrous composition makes it a good anchor for deep sutures. The galea is readily mobilized, facilitating wound closure and the development of local flaps. The subgaleal fascia is the plane in which scalp avulsions almost exclusively occur ( Fig. 19-1 ).
Scalp injuries, particularly avulsions, often bleed profusely, and patients presenting with hemorrhagic shock require aggressive fluid resuscitation and blood replacement. Blood loss can be minimized with the application of pressure dressings or ligation of the galeal vessels and temporary suturing or stapling of the wounds. The vigorous blood supply of the scalp enhances the viability of tissue fragments that would not survive elsewhere. Near-complete avulsions of scalp segments may survive on small bridges of tissue or even as isolated islands. Only obviously devitalized tissue should be débrided. Scalp tissue that appears to have even a tenuous blood supply should be given the benefit of the doubt and retained, because the hair that it contains is a valuable resource. Any nonviable tissue can be readily removed and usually is not a source of infection. The robust blood supply serves as an adjunct in the prevention of infection. Scalp infections are uncommon even in contaminated wounds, and the resistance to infection makes it unnecessary to clip or shave hair from wound edges, unless doing so aids the alignment of the tissues.
Primary closure is the method of choice when there is no significant tissue loss (<3 cm). The wound edges tend to contract, and what initially appears to be a large defect may be relatively easily closed with subgaleal undermining ( Fig. 19-2 ). Wounds on the vertex of the scalp are usually more difficult to close because of the decreased tissue mobility in that region. Scoring of the galea on its deep surface is a well-described procedure to facilitate closure. It consists of transverse incisions made perpendicular to the axis of advancement. Care should be taken not to damage the more superficial subcutaneous vessels.
A layered primary closure is carried out if the galea has been lacerated. The galea adheres tightly to the overlying skin, and its approximation facilitates skin closure. Failure to repair this layer may result in cosmetic deformity, ranging from a depressed scar to asymmetrical brow contraction. Closure of the galea also prevents the spread of wound contaminants to the intracranial cavity through the emissary veins, which connect the skin to the venous sinuses. Satisfactory galeal closure prevents the development of most potential problems, including osteomyelitis and meningitis. The galea is approximated with interrupted, 2-0 or 3-0, slowly resorbable sutures.
Because a noticeable scalp scar is determined primarily by the presence of alopecia, great care should be paid to follicular viability. Dermal sutures are used sparingly, or not at all, to reduce the possibility of hair follicular damage. Restoring the continuity of the galea obviates the need in most cases for dermal sutures, relieving tension on the skin sutures so they may be removed early. Closure of the skin is carried out using non-interlocking, continuous sutures of 3-0 nylon or Prolene in adults and 4-0 sutures in children ( Fig. 19-3 ). Metallic staples may also be used, but their removal is painful.

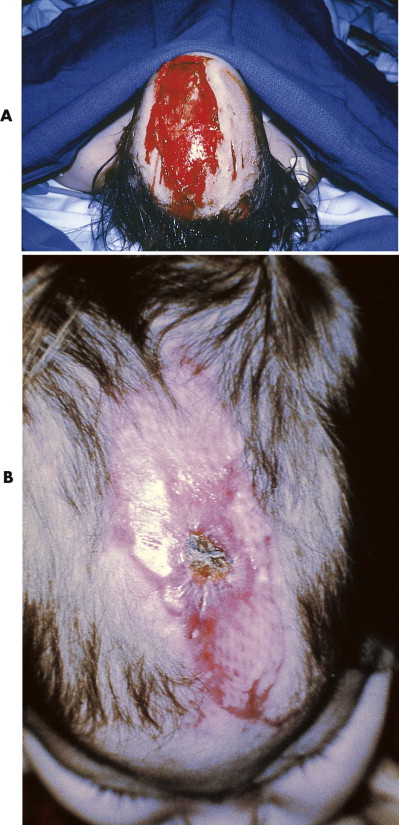
Split-Thickness Skin Grafting
Placement of a split-thickness skin graft is the treatment of choice for most larger scalp defects that are not amenable to primary closure. The pericranium must be intact, because grafts cannot succeed on denuded bone. Split-thickness skin grafts provide a rapid and reliable method for wound coverage in the acute setting ( Fig. 19-4 ). The 0.14- to 0.20-inch-thick grafts are harvested with a dermatome, usually from the lateral thigh. They can be placed as sheet grafts if encroaching on the forehead, but they typically are meshed in a 1.5 : 1 ratio and placed with minimal expansion. Meshing the graft has two purposes: It engrafts better without bolstering by allowing fluid egress, and it results in greater wound contracture, which is subsequently beneficial. Because scalp skin grafts are ultimately esthetically undesirable due to contour depression and alopecia, they are usually serially excised about 6 months after placement. Because split-thickness skin grafts contract by 20% to 40%, the reduction in size of the defect aids secondary excision and closure. In grossly contaminated wounds and those in which the viability of the pericranium is questionable, a homograft (cadaveric) or xenograft (porcine) may be used as a temporary biological dressing until the placement of an autograft is considered appropriate.
The lack of a pericranium obviates the success of a skin graft. In the absence of a pericranium, the outer table of the cranium typically is removed, exposing the well-vascularized diploë, which is an excellent bed for grafting. This can be done by burring away the outer table or drilling multiple holes through the outer table; either method allows granulation tissue to cover the exposed bone. After about 3 weeks, there should be a satisfactory covering of healthy granulation tissue on which the graft can be placed. Although this is an effective method to achieve epithelial coverage, it does require a considerable delay between bone removal and placement of the graft, and it is likely to leave a poorly contoured defect.
Flaps
Unless there are contraindications, a flap procedure provides a more expedient solution than grafting or removal of the outer bone plate. A locally based pericranial flap is used if the defect is small, or a free tissue transfer is employed for larger defects. Pericranial flaps enable the transfer of a thin, vascularized cover onto which a skin graft can be placed. Although originally thought to be random in nature, much of the blood supply of flaps is derived from the overlying subgaleal fascia, which usually is elevated with the flap. To be effective and reliable, the pericranial flap should be centered on a major vascular territory with minimal dissection close to the pedicle ( Fig. 19-5 ). The blood supply is extremely sensitive, and postoperative graft dressings should be very lightly applied.

Use of Local Flaps
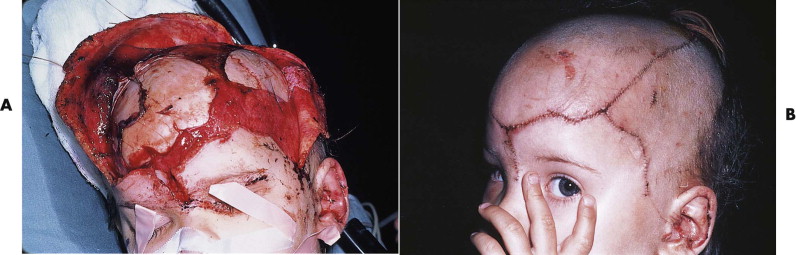
Flaps using local scalp tissue are appropriate for relatively small, partial- or full-thickness defects (3-5 cm wide). Local flaps permit closure of the defect with hair-bearing skin of similar thickness. Their use is appropriate for the cover of clean, sharply defined lacerations when surrounding tissue viability is not compromised. Many traumatic scalp wounds are the result of crush or avulsion injuries in which adjacent tissue damage is inevitable. Flap elevation may further compromise an already tenuous blood supply, and local flaps that must be raised and rotated have only limited use in these circumstances ( Fig. 19-6 ).

Use of Free Tissue Transfer
The transfer of free, vascularized flaps is a long and potentially demanding procedure, and the timing must be considered with care. It is not a procedure to start late at night with tired or inexperienced surgeons and anesthetists; it should be a planned, semi-elective procedure. Wet-dry dressings may be applied to large, denuded defects until free, vascularized tissue transfer can be arranged. Flaps should be muscular for bulk and should have maximal vascularity. The flap of choice usually is the latissimus dorsi because of its large surface area, relatively long pedicle, and ease of harvest ( Fig. 19-7 ). Other options include the rectus abdominis muscle, scapular or parascapular flaps, and the omental fat flap. Most of these options require a simultaneously placed split-thickness skin graft for outer coverage of the flap.

Replantation
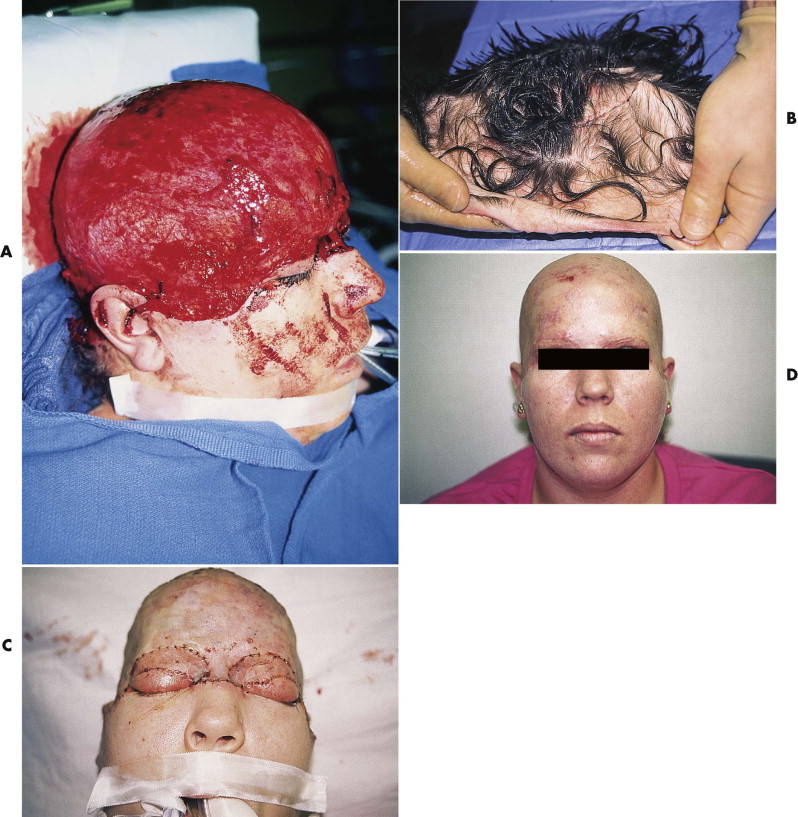
Microsurgical scalp replantation is the treatment of choice for total or near-total scalp avulsion. These uncommon injuries have a classic presentation and are usually caused by entanglement of long hair in rotating machinery. Separation occurs in the subgaleal, loose areolar plane at the peripheral margins of the scalp, where the galea is less resistant to applied force. Partial-avulsion injuries are rare, and the scalp and forehead typically are removed as a single anatomical unit ( Fig. 19-8 ). The upper eyelids and portions of the ears may be included in the avulsed segment because of the intimate relationship between the muscular segments of the galea and these structures.

Microsurgical replantation, if successful, is esthetically and functionally superior to any other method of wound closure or coverage. It restores normal hair growth in unscarred areas, and a large amount of the avulsed segment, such as eyelids and ears, can be expected to survive (see Fig. 19-8C ). Provided that the avulsed segment is not severely crushed and mutilated and the period of warm ischemia was not greater than 12 hours, every effort should be made for replantation.
Successful replantation depends on emergency access to the operating room, finding suitable recipient vessels in the surrounding temporal scalp or neck (which is always possible), and finding suitable vessels in the avulsed segment (which is not always possible). Vein grafts may be needed to move the microvascular repair out of the zone of injury and reduce tension along the vessels and across the anastomoses. Although the scalp can survive with only one arterial anastomosis, it is preferable to identify at least two vessels suitable for repair. It is possible (although rare) to identify and repair bilateral superficial temporal and occipital arteries. Because venous congestion is the predominant cause of most postoperative flap failures, it is essential to ensure adequate venous outflow. If no suitable veins are available, venous outflow can be achieved by anastomosis of a scalp artery directly to a recipient vein. The use of medicinal leeches is an option, but a large scalp replant requires four to six leeches concurrently, and the patient needs extensive transfusions until venous outflow is reestablished. Most established scalp replants require secondary revision of the scars, eyelids, ears, and any large remaining areas of alopecia. If it is not possible to replant the scalp, coverage may be obtained using one of the methods previously described ( Fig. 19-9 ).
If avulsion occurs in the forehead region, primary closure can be a problem because of the difficulty in recruiting local tissue to cover the defect. Extensive mobilization and release of the galea can help, but only for closure of defects of several centimeters. Reduction of the width of the forehead causes problems with medial or superior eyebrow transposition and frontal hairline disturbances, neither of which is easy to restore secondarily without recreating the original defect. Initial repair is usually best managed by coverage with a split- or full-thickness skin graft. If the avulsion is only of partial thickness, with preservation of some or all of the frontalis muscle, a full-thickness graft or unmeshed, thick, split-thickness graft may produce a reasonable result without significant contour deformity ( Fig. 19-10A and B ). If only pericranium is left, a split-thickness skin graft produces a healed but depressed wound that will require secondary reconstruction through tissue expansion or local flaps, or both (see Fig. 19-10C and D ).

The eyebrow is the most valuable esthetic structure of the forehead. Preservation of hair-bearing skin and accurate realignment of the eyebrow unit is essential ( Fig. 19-11 ). Eyebrow hair should not be shaved because it may not fully regrow, and the likelihood of secondary eyebrow deformities is increased even if it does regrow. After a portion of the eyebrow is lost, the remaining portion should be put back together along its preinjury arc, even if this creates a larger forehead defect. Closure of the wound with the eyebrow canted up or down can make secondary reconstruction more difficult, although a Z -plasty often can provide an effective solution. Significant eyebrow loss ultimately requires free scalp grafts or micrograft hair transplants for reconstruction (see Figs. 19-10D and 19-11D ).

Eyelids
In the management of eyelid injury, associated trauma to the underlying globe must be excluded. If the cornea has been exposed, care should be taken that the cornea remains moist by regular saline irrigation or placement of a saline-soaked dressing. At the time of repair, it is good practice to protect the cornea with a soft lens or shield. If injury is not seen or suspected, an ophthalmologist’s opinion is not immediately necessary, and visual acuity can be assessed by simple tests. If an injury is suspected, an expert evaluation is mandatory. A common error is to miss a foreign body. Lifting the lids away and carefully inspecting the depths of the fornices is a simple but important procedure. Corneal abrasions are common in facial trauma, and pain and irritation of the injured eye are typical findings. Definitive diagnosis requires ophthalmological assessment with fluorescein dye and slit-lamp examination.
With appropriate treatment, healing is usually rapid and uncomplicated. In rare cases, devastating infection can occur with Pseudomonas, which warrants an immediate ophthalmological intervention.
For practical purposes, the eyelid has two layers: an inner layer comprising the tarsal plate and conjunctiva and an outer layer of skin and orbicularis muscle ( Fig. 19-12A ). Apposition of skin, muscle, and tarsal plate is important, because conjunctival lacerations frequently heal adequately on their own. Lacerations in the upper eyelid may disrupt the levator aponeurosis and, if not properly repaired, result in postoperative downward positioning of the upper eyelid (i.e., ptosis). Downward positioning of the lower eyelid (i.e., ectropion) is usually the result of lacerations that run perpendicular to the lid margin; it is caused by poor anatomical realignment, tissue loss, or canthal disruption.
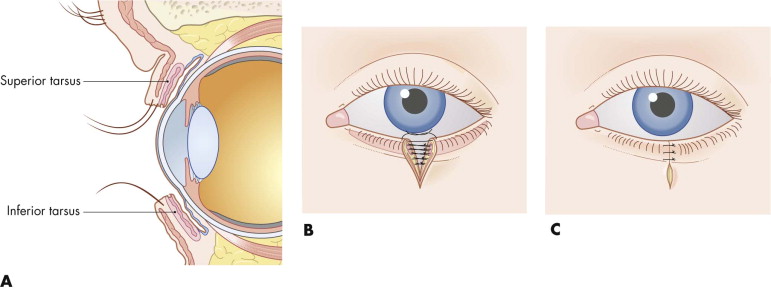
Full-thickness eyelid lacerations should have the lid margin approximated first by lining up the gray line (i.e., squamous-mucosal junction) or the meibomian gland orifices with 7-0 Vicryl suture, with the tail of the suture left long so it can be sewn down by the adjacent sutures. The remainder of the laceration is repaired in layers with 6-0 Vicryl for the tarsus and muscle; 6-0 plain or chromic gut, with the knots inverted to prevent corneal irritation, for the conjunctiva; and 6-0 or 7-0 nylon or Prolene for the skin (see Fig. 19-12B and C ). Approximating the tarsus and the ciliary margin are the crucial steps provided there is no significant tissue loss. For partial-thickness injuries with skin loss, full-thickness skin grafts from the avulsed segment (if available) or from the opposite upper eyelid or postauricular area can be used. For small, full-thickness defects involving less than one third of the lid, primary closure can be carried out. Many defects involving up to one half of the lid can be primarily closed with release of the lateral canthus ( Fig. 19-13 ). Defects larger than one half of the lid require a cheek advancement (i.e., Mustarde rotation flap) or an upper lid switch procedure. Use of these more extensive flap procedures, which are often only one-time use techniques, is not advised in the acute trauma setting. In some cases with more superficial loss, a full-thickness graft from the other upper eyelid is desirable.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


