Sickle cell anemia is a common hereditary hematologic disease. It affects many systems and tissues in the body, including the mouth. Delayed tooth eruption, an uncommon degree of periodontitis, alterations in the cells of the tongue surface, hypomaturation and hypomineralization in enamel and dentin, pulp calcifications, hypercementosis, and bone alterations resulting in maxillary protrusion and formation of a thick trabecular pattern are some oral manifestations of the disease. The aim of this study was to report the orthodontic treatment of a patient with sickle cell anemia. Treatment consisted of correcting a Class II dental and skeletal pattern with an extraoral appliance combined with a fixed orthodontic appliance. From the orthodontic point of view, the results were satisfactory: the occlusion was normalized, and the patient’s health was maintained throughout the entire treatment period.
Sickle cell anemia is one of the most common hereditary hematologic diseases worldwide, and it is usually considered a matter of public health. It is a hereditary type of chronic hemolytic anemia, caused by a genetic mutation of the hemoglobin A molecule, which is called hemoglobin S.
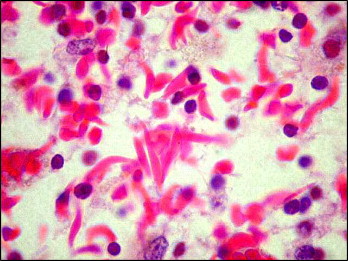
Hemoglobin is a respiratory protein in the erythrocytes with the primary function of transporting oxygen throughout the body. Molecular biology explains sickle cell anemia as a mutation of the hemoglobin that leads to cells that look like sickles. In situations of low oxygen tension, the affected hemoglobin molecules change from their normal disk shape to sickle shape. Initially, when the oxygen level increases, this sickling is reversible; however, the constant changes of shape of the red blood cells harm their cell membranes, which become rigid and no longer return to their normal state. This results in decreased capacity to transport oxygen to the tissues, vaso-occlusion conditions, and diminished lifespan of the red blood cells.
These physiopathologic events are the determinant in the origin of most signs and symptoms in the clinical condition of patients with sickle cell anemia: algic crises, high susceptibility to infections, hemolytic crises, ulcers in the lower limbs, splenic sequestration, priapism, strokes, and chronic compromise of multiple organs, systems, or processes.
The clinical spectrum of involvement can vary greatly from patient to patient. The pathologic effects of sickle cell anemia, demonstrated in mineralized and connective tissues in other areas of the body, also occur in oral tissues. The most common findings described in the literature involving the oral region are paleness of the oral mucosa, delayed tooth eruption, uncommon degree of periodontitis, alterations in the cells of the tongue surface, hypomaturation and hypomineralization in enamel and dentin, pulp calcifications, hypercementosis, and bone alterations, resulting in maxillary protrusion and formation of a thick trabecular pattern.
There is no specific treatment for sickle cell anemia, and it is necessary to include preventive measures to ameliorate its consequences. These measures include good nutrition, prophylaxis, early diagnosis of and treatment for infections, maintenance of good hydration, and avoidance of adverse climate conditions. Allied with the preventive measures, folic acid is indispensable, because of its fundamental importance in the maturation and speed of red blood cell production, and should be prescribed for patients with sickle cell disease. In some cases, it is associated with vitamin B12.
Orthodontists should have knowledge of the oral manifestations and possible interferences of sickle cell anemia in orthodontic treatment. Nevertheless, no article describing orthodontic treatment in these patients was found, only cephalometric evaluations in population groups with this pathology and descriptions of the effects of this pathology on craniofacial growth. With the intention of filling this gap, the objective of this article was to describe the clinical orthopedic and orthodontic treatment of a patient with sickle cell anemia, its particularities, and the care to be taken.
Diagnosis and etiology
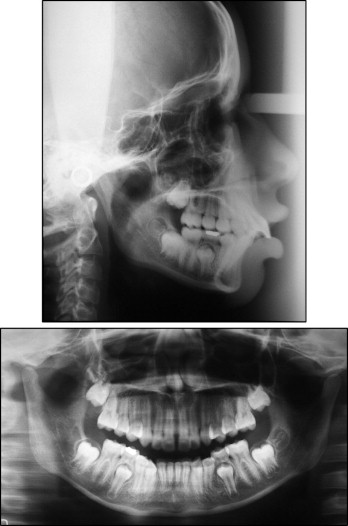
The patient, a 12-year-old girl, came for orthodontic consultation with the chief complaint of misaligned and protruding teeth ( Fig 1 ). Her mother said that she had sickle cell anemia and was under the care of a hematologist ( Fig 2 ). According to the mother, the girl took supplements of folic acid associated with vitamin B12, prescribed by the hematologist. Clinically, she patient had a good state of general health, without any complications because of this pathology.

For adequate orthodontic treatment, it is indispensable to know the medical history of a patient with sickle cell disease, as well as his or her family history, to gain knowledge of the degree of systemic compromise of the disease.
The patient had an Angle Class II dental relationship, 12 mm of overjet, and an exaggerated anterior overbite ( Fig 3 ). The gingivae showed discrete paleness, particularly in the posterior region. Enamel hypoplasia was noted on the maxillary incisors on the right side ( Fig 1 ).

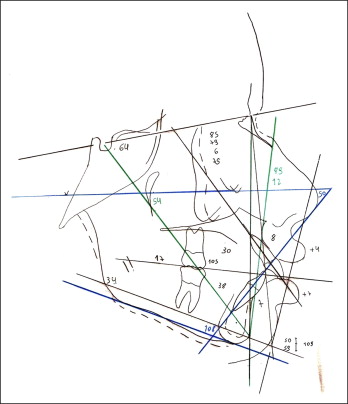
Cephalometrically, the patient had a Class II skeletal relationship (ANB, 6°) with maxillary protrusion (SNA, 85°) and a slightly retruded mandible (SNB, 79°), a trend toward a vertical facial growth pattern (SnGoGn, 34°), vestibularization and protrusion of the maxillary and mandibular incisors (1.NA, 30°; 1-NA, 8 mm; 1.NB, 38°; 1-NB, 7 mm), and a convex facial profile (LS-S, 4 mm; LI-S, 7 mm) ( Figs 4 and 5 ).
Treatment objectives
The goals were to correct the skeletal Class II relationship, improve the Class II dental relationship, harmonize the facial profile, improve the esthetics of the smile, and maintain the patient’s general health.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


