Introduction
Cone-beam computed tomography (CBCT) imaging has broadened opportunities for examining morphologic aspects of the craniofacial complex, including alveolar bone, but limitations of the technology have yet to be defined. Through the use of comparisons with direct measurements, the purpose of this study was to investigate the accuracy and reliability of buccal alveolar bone height and thickness measurements derived from CBCT images.
Methods
Twelve embalmed cadaver heads (5 female, 7 male; mean age: 77 years) were scanned with an i-CAT 17-19 unit (Imaging Sciences International, Hatfield, Pa) at 0.3 mm voxel size. Buccal alveolar bone height and thickness measurements of 65 teeth were made in standardized radiographic slices and compared with direct measurements made by dissection. All measurements were repeated 3 times by 2 independent raters and examined for intrarater and interrater reliability. Measurement means were compared with 2-tailed t tests. Agreement between direct and CBCT measurements was assessed by concordance correlation coefficients, Pearson correlation coefficients, and Bland-Altman plots.
Results
Intrarater reliability was high as were interrater correlations for all measurements (≥0.97) except CBCT buccal bone thickness (0.90). CBCT measurements did not differ significantly from direct measurements, and there was no pattern of underestimation or overestimation. The mean absolute differences were 0.30 mm in buccal bone height and 0.13 mm in buccal bone thickness with 95% limits of agreement of −0.77 to 0.81 mm, and −0.32 to 0.38 mm, respectively. Agreement between the 2 methods was higher for the measurements of buccal bone height than buccal bone thickness, as demonstrated by concordance correlation coefficients of 0.98 and 0.86, respectively.
Conclusions
For the protocol used in this study, CBCT can be used to quantitatively assess buccal bone height and buccal bone thickness with high precision and accuracy. Comparing the 2 sets of CBCT measurements, buccal bone height had greater reliability and agreement with direct measurements than did the buccal bone thickness measurements.
Orthodontists have historically relied on 2-dimensional imaging to aid diagnosis and treatment planning as well as to monitor treatment progress and growth. This traditional imaging approach limits analysis to linear and angular measurements between landmarks superimposed onto a single plane of space, often leading to distortion errors. Conventionally, the most accurate measures have relied on direct evaluation of patients or objects, and this remains the standard from which to judge other measurement techniques. With the advent of 3-dimensional imaging modalities such as conventional computed tomography (CT) and cone-beam CT (CBCT), practitioners can now visualize and measure the true 3-dimensional anatomy of patients. In addition to avoiding the intrinsic weaknesses of 2-dimensional imaging (distortion, superimposition), CBCT also allows measurements to be made in planes of space not available or accurately depicted in traditional radiographs. However, limits to the accuracy of CBCT measurements have not been well defined.
For several decades, conventional CT has been used selectively for imaging of the craniofacial region—eg, to evaluate the temporomandibular joint, osseous pathology, deformities, and asymmetries. However, drawbacks including cost, equipment size, and risks associated with relatively high radiation doses have made conventional CT impractical for many dental applications.
Increasingly over the past decade, CBCT imaging has been advocated for head and neck applications due in part to advantages of reduced cost and radiation exposure relative to conventional CT technology. Multiple orthodontic applications have been described including locating impacted teeth, quantification of bone modeling, displacement in response to orthognathic surgery or growth modification, 3-dimensional analysis of facial asymmetries, soft tissues, and airways, visualization of root resorption and inclination, and improved cephalometric landmark identification. By offering isotropic voxels (volumetric pixels that are identical length in all 3 dimensions) ranging from as small as 0.07 to 0.25 mm, CBCT potentially provides a means to accurately measure the craniofacial complex in detail. For example, investigators have used CBCT to document changes in buccal bone dimensions after rapid palatal expansion and archwire expansion of the dental arches.
A potential side effect of buccal orthodontic tooth movement on the alveolus has previously been demonstrated in animal studies and histologic examinations. In monkey and dog models, bony dehiscences of tooth roots have been produced by such tooth movements with little correlation to connective tissue attachment loss. Because such deterioration of underlying periodontal structures might not be reflected in the clinical appearance of the dentition and the soft tissues, orthodontists might be blinded to the creation of irreversible hard-tissue changes that could accompany such tooth movements. Because histologic cross-sections are not a realistic option in patients and routine soft-tissue reflection is impractical and potentially damaging, the unique combination of submillimeter resolution with multiple display modes (eg, oblique or nonorthogonal orientation) and real-time analysis and enhancement options (eg, reformatting images or realigning slices) potentially makes CBCT imaging ideal for evaluating alveolar bone changes associated with orthodontic treatment.
Whereas CBCT imaging is generally regarded as inherently accurate, to date there are limited published reports confirming this. Studies that have examined accuracy favor CBCT over more traditional imaging modalities such as cephalograms and periapical radiographs, as well as conventional CT. However, compared with direct anthropometric measurements, the results of several CBCT investigations suggest that further inquiries are warranted to better define the limitations of measurements derived from CBCT imaging. As examples, Lascala et al found that CBCT-derived measurements consistently underestimated direct measurements over large distances (30-100 mm), with differences ranging from 3.43 to 6.59 mm. Baumgaertel et al showed a similar trend for underestimating dental measurements such as mesiodistal tooth widths and overjets on dry skulls, with these differences becoming significant for values such as available arch length when calculated from multiple measurements. Lastly, Berco et al found that distances between traditional cephalometric landmarks made on images of dry skulls had statistically significant mean measurement errors compared with direct measurements.
The findings of statistically significant measurement errors in the studies above that were made under ideal laboratory conditions justify caution in accepting the premise that clinically related CBCT images are fundamentally accurate. Additionally, variations in imaging parameters, subjects, and structures of interest make it difficult to confidently apply the results more broadly to structures and clinical conditions that have not yet been investigated. With clinical studies relying on CBCT imaging currently reaching the literature in an attempt resolve an orthodontic controversy regarding the effects on alveolar bone when teeth are moved facially, it is essential to investigate the accuracy of the technique under conditions that replicate clinical imaging.
The purpose of this study was to investigate the reliability and accuracy of measurements of alveolar buccal bone height and thickness from CBCT scans of cadaver heads relative to direct measurements acquired after dissection by using multiple measures of reliability and agreement.
Material and methods
Human cadaver specimens were made available through the Department of Integrative Biosciences, School of Dentistry, Oregon Health and Science University, Portland, Ore, after review and approval of the study’s protocol by the institutional review board. A preliminary screening of 17 subjects was performed, with 12 dentate cadavers fulfilling the initial selection criteria of no full-mouth restorations, no clinically observable oral pathology or mechanical damage in the oral region, and no prior dissection of the craniofacial complex. The sample consisted of 5 female and 7 male subjects, all white, with ages ranging from 55 to 89 years (mean, 77 years). A final sample of 65 teeth was selected by direct observation based on the following inclusion criteria: (1) no alloy restoration in the tooth itself or adjacent teeth, (2) intact crown, and (3) a periodontium without embalming-related artefacts such as pins or wires. To help distribute the sampling among all specimens, maximums of 4 anterior and 4 posterior teeth were selected from each cadaver. Table I shows the distribution of the teeth examined by tooth type. To facilitate the logistics of CBCT imaging, before transport, all specimens were disarticulated below the shoulder.
| Tooth type | Maxilla | Mandible | Total |
|---|---|---|---|
| Anterior | |||
| Central incisor | 14 | 21 | 35 |
| Lateral incisor | 0 | 2 | 2 |
| Canine | 2 | 9 | 11 |
| Anterior total | 16 | 32 | 48 |
| Posterior | |||
| First premolar | 1 | 8 | 9 |
| Second premolar | 1 | 5 | 6 |
| First molar | 1 | 0 | 1 |
| Second molar | 1 | 0 | 1 |
| Posterior total | 4 | 13 | 17 |
| Total | 20 | 45 | 65 |
The CBCT scans were acquired using an i-CAT 17-19 CBCT unit (Imaging Sciences International, Hatfield, Pa) by using the technical parameters and settings listed in Table II . The cadaver specimens were wrapped in a plastic barrier and placed on top of a base in the i-CAT motorized chair. Each specimen was oriented to replicate normal patient positioning and secured with a chin support, a head support, and a forehead strap. A preview image was then exposed to validate the appropriate head positioning before acquiring the CBCT scan. The CBCT scans were saved as digital imaging and communications in medicine (DICOM) files.
| Technical parameter | Value |
|---|---|
| Manufacturer | Imaging Sciences International, Hatfield, Pa |
| X-ray source voltage | 120 kVp |
| X-ray source current | 3-8 mA (pulse mode) |
| Focal spot size | 0.5 mm |
| X-ray beam size | 0.5 × 0.5−8 × 10 in |
| Scanning time | 8.9 s |
| Total number of pulses | 309 |
| Image acquisition rotation | 360° |
| Image detector | Amorphous silicon flat panel detector |
| Gray scale | 12 bit |
| Field of view | Landscape 13 mm |
| Voxel size | 0.3 mm |
After the CBCT scans, the specimens were dissected by using a full-thickness buccal flap reflected around each tooth of interest. Buccal bone height was measured by using a digital vernier caliper (General Tools, New York, NY) with a reading to the nearest 0.01 mm. Buccal bone height was defined as the linear distance from the incisal edge or the buccal cusp tip to the buccal alveolar crest along the long axis of the tooth ( Fig 1 , A and B ). The coronal reference point was defined as the mesiodistal center of the incisofacial (or occlusofacial) line angle of the tooth of interest. The apical reference point was defined as the mesiodistal center of the root surface at the height of the buccal bone plate. For rotated teeth, the mesiodistal width was measured from contact to contact of adjacent teeth, and measurements were made in the plane of space perpendicular to the dental arch form ( Fig 1 , C ). In cases of maxillary molar measurements, the mesiobuccal cusp and root were measured.
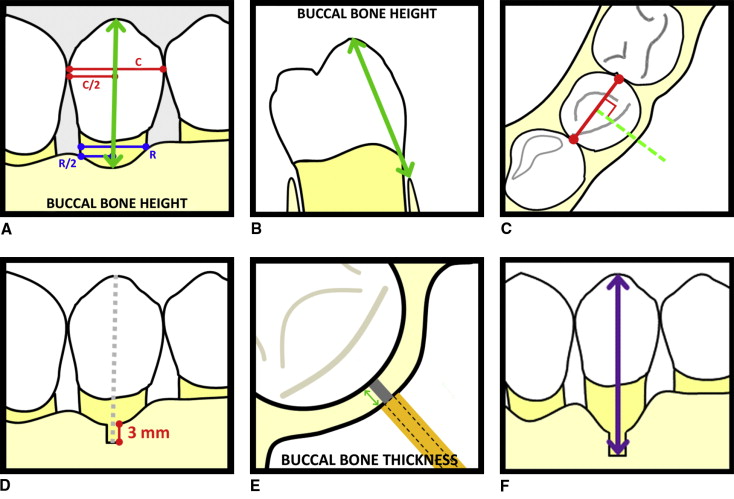
In preparation for the buccal bone thickness measurements, a section of buccal alveolar bone approximately 3 mm in height was removed from the most coronal aspect of the alveolar bone along the long axis of the tooth ( Fig 1 , D ). Buccal bone thickness was measured in the mesiodistal center of the newly exposed root surface from the most buccal cortical bone to the cementum by using a modified depth gauge accurate to 0.01 mm held parallel to the occlusal plane ( Fig 1 , E ). To account for the effect of rotations on the measured bone thickness, the measurements were made in the plane of space perpendicular to the dental arch form.
For both buccal bone height and buccal bone thickness values, 2 investigators (A.T., V.C.) each made 3 independent measurements, with a minimum interval of 1 day between measurements. Additionally, to measure buccal bone thickness at the same bone level in the CBCT images, each investigator measured the height at which the buccal bone thickness values were measured relative to the coronal reference point ( Fig 1 , F ), and the average was cross-referenced during the CBCT measurements.
The DICOM files were imported into Dolphin 3D Imaging (Dolphin Imaging Systems, Chatsworth, Calif) for analysis. As with the direct measurements, 3 separate CBCT measurements of buccal bone height and buccal bone thickness were made independently by the same 2 investigators, with a minimum interval of 1 day between recordings. The measurements were made in the appropriate sectional slice of 0.5 mm thickness in a darkened room. A standardized orientation was established, and a step-by-step protocol was followed.
- 1.
The image was oriented so that the occlusal plane was parallel to the axial plane in the frontal and lateral views, and the head’s midline was bisected by the midsagittal plane ( Fig 2 , A ).
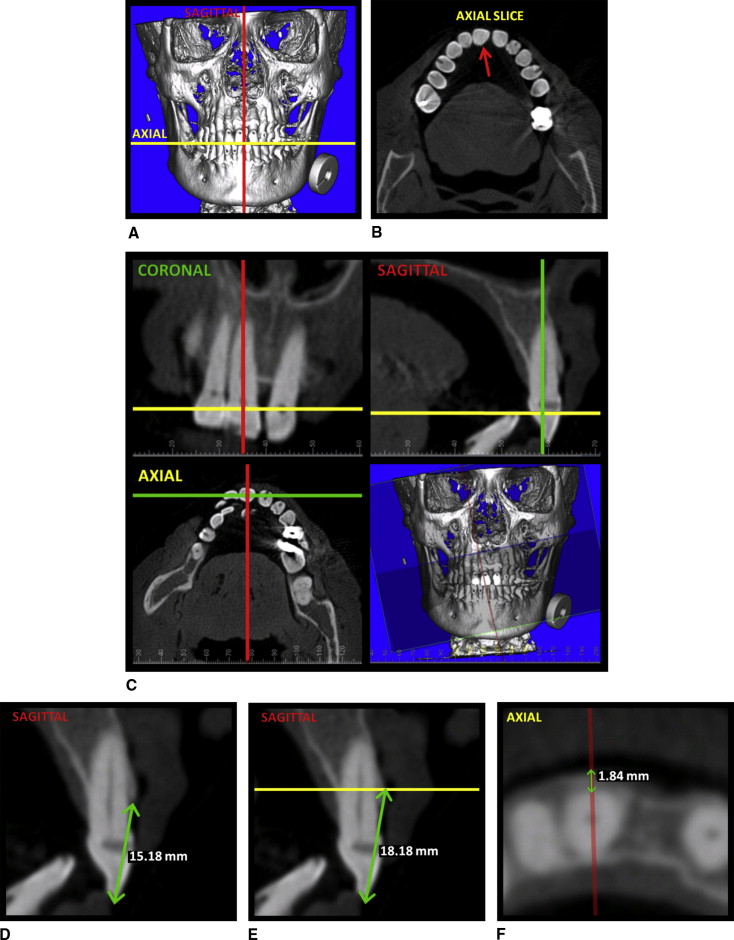
Fig 2 CBCT measurement protocol: A, initial orientation of the image in the 3-dimensional volumetric view; B, the axial plane was adjusted to pass through the crown of the tooth of interest ( red arrow ); C, the coronal and sagittal planes were oriented to pass through the long axis of the tooth of interest with the sagittal plane oriented perpendicular to the arch form as viewed in the axial plane; D, measurement of buccal bone height ( green arrow ) was made in the sagittal plane from the incisal edge (or the buccal cusp tip) to the alveolar bone crest; E, to measure buccal bone thickness, the axial plane ( yellow line ) was repositioned to the height recorded for the direct buccal bone thickness measurement ( Fig 1 , F ); F, buccal bone thickness was measured ( green arrow ) in the axial plane from the root surface to the buccal aspect of the alveolar bone along the orientation of the sagittal plane ( red line ). - 2.
The axial plane was selected to intersect with the crown of the tooth of interest ( Fig 2 , B ).
- 3.
The coronal and sagittal planes were adjusted to pass through the center of the crown and root of the tooth of interest (dilacerated apices were ignored), with the sagittal plane perpendicular to the subject’s arch form in the axial view ( Fig 2 , C ).
- 4.
By using the sagittal view, buccal bone height was measured from the most incisal (or occlusal) and buccal aspects of the tooth to the most coronal aspect of the buccal alveolar bone crest ( Fig 2 , D ).
- 5.
The apical reference point identifying the alveolar crest was dragged apically along the buccal aspect of the alveolar bone to the height at which the direct buccal bone thickness measurements were made as described above ( Fig 2 , E ).
- 6.
The axial plane was adjusted to the height established in step 5 ( Fig 2 , E ), and buccal bone thickness was measured from the most buccal aspect of the root to the most buccal aspect of the alveolar bone along the orientation of the sagittal plane ( Fig 2 , F ).
Statistical analysis
A generalizability analysis was performed by using EduG (version 6.0; Swiss Society for Research in Education Working Group, Neuchatel, Switzerland) to assess the sources of error variation for both buccal bone height and buccal bone thickness measurements. Data from repeated measurements were pooled to examine interrater reliability within the method.
Interrater reliability was described by mean differences and mean absolute differences (positive or negative signs ignored), and further analyzed by calculating concordance correlation coefficients and Pearson correlation coefficients by using Stata statistical software (release 11.0; StataCorp, College Station, Tex) for 4 sets of data: direct measurements of buccal bone height, direct measurements of buccal bone thickness, CBCT measurements of buccal bone height, and CBCT measurements of buccal bone thickness. The concordance correlation coefficient, although similar to the Pearson correlation coefficient in measuring the linear relationship, or association, between 2 sets of data, also takes into account any departure from a line of perfect agreement such as a scale or a location shift.
Overall measurement accuracy was evaluated by using pooled data from both raters. Comparisons of means, mean differences, and mean absolute differences between the direct and CBCT methods were made in addition to concordance and Pearson correlation coefficients. Two-tailed paired t tests were performed to examine differences between means derived from the 2 measurement methods, with the level of significance set to P ≤0.05. Agreement between direct and CBCT measurements was analyzed with Bland-Altman plots by using 95% limits of agreement (average differences ±1.96 of the standard deviation of the differences).
Results
The generalizability analysis showed that the percentages of variance due exclusively to the timing of the measurements were small: 0.0% and 0.3% for buccal bone height and buccal bone thickness, respectively. Including all interactions of time with the other variables (rater, method, and subject), additional values of 1.4% and 11.3% of variance, respectively, were associated in part to time. Because the amount of variance from the repeated measures was minimal, and to facilitate the analysis of the reliability between raters, the data were pooled across time points.
Table III displays the descriptive statistics for the agreement between raters for buccal bone height and buccal bone thickness measured directly and from CBCT images. The concordance and the Pearson correlation coefficients between raters for the direct measurements of buccal bone height and buccal bone thickness were extremely high (≥0.98). The concordance and the Pearson correlation coefficients for CBCT buccal bone height measurements also demonstrated excellent agreement and reliability (0.98 for both), whereas buccal bone thickness measurements showed more modest agreement (0.90 and 0.91, respectively).



