Root resorption is a common problem associated with orthodontic treatment. Minor and clinically insignificant amounts of root resorption occur frequently. In some rare cases, however, the extent of orthodontically related root resorption can be severe enough to jeopardize the prognosis for the teeth involved ( Fig. 27-1 ). This chapter discusses the following topics related to orthodontic root resorption: (1) clinical and biological background; (2) epidemiology; (3) risk factors; and (4) prediction, early detection, and treatment.

CLINICAL AND BIOLOGICAL BACKGROUND OF ROOT RESORPTION
Whether occurring in the pulp chamber or on the root surface, root resorption is almost always associated with a healing response to some type of insult. Injured tissue is removed in preparation for the reparative phase of wound healing. The mechanism controlling this reparative process currently is not well understood, but newer evidence suggests that the mechanism may be similar to that controlling bone remodeling.
In bone remodeling the receptor activator of nuclear factor kappa B (NF-κB) ligand (RANKL), found on the osteoblast stromal cells, binds to RANK, located on the osteoclast precursor cells, to stimulate osteoclast numbers and activities. Osteoprotegerin (OPG) is a circulating molecule that acts as a decoy receptor that binds to RANKL, thereby preventing the genesis of osteoclasts. The relative concentration of the stimulator and inhibitor is a common signaling mechanism that controls osteoclasts and bone remodeling in response to most stimulators. As with other stromal cells, periodontal ligament (PDL) cells and cementoblasts possess RANKL, suggesting that they also may be able to control odontoclastogenesis and root resorption in response to stimulation by parathyroid hormone–related protein (PTHrp). Some investigators have suggested that antiresorption factors may reside in both the PDL and the pulp, and if these are impaired by injury, root resorption can occur. Current evidence suggests that such a mechanism may exist in the form of OPG, but that the ultimate control of root resorption may reside in a combination of both inhibition and stimulation of odontoclasts. The clinical observation that endodontically treated teeth are more resistant to orthodontic root resorption suggests that pulpal cells also may play a role in this control.
The most common classification of external root resorption categorizes the sites in ascending order of the severity of associated trauma. The mildest form, surface root resorption, is characterized by cemental cratering that can extend into the dentin. These sites are usually adjacent to focal injuries in the PDL, the most common being the hyalinization lesions that occur at compression sites during orthodontic tooth movement. Inflammatory root resorption is the next order of severity. Involved sites are adjacent to inflammatory lesions and may be related to orthodontic tooth movement, but usually these are related to more extensive injuries of traumatic or endodontic origin. The response to the most severe types of injuries, including tooth displacement, avulsion, and reimplantation, manifests as replacement resorption. The radiographic picture of replacement resorption is characterized by root resorption, with the crater being repaired by bone. This type of resorption is often progressive and, because the PDL space is lost, results in ankylosis of the tooth.
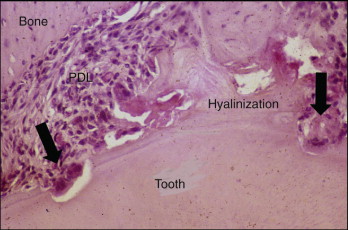
The pathogenesis of orthodontic root resorption has been well described through animal models and initiates at sites of compression. Orthodontic appliances produce sustained pressure that exceeds the pressure in the PDL arterioles. This results in their occlusion and the necrosis of the PDL served by them. These necrotic lesions, known as “hyalinizations” because of their histological resemblance to hyaline cartilage, have been well described and consist of cells with pyknotic nuclei, as well as fragmented PDL fibers. Adjacent arterioles compensate by becoming engorged, and the lesions are removed at the periphery by various resorptive cells, including macrophages, osteoclasts, and cementoclasts. Surface root resorption results from this peripheral removal at the tooth surface ( Figs. 27-2 and 27-3 ).
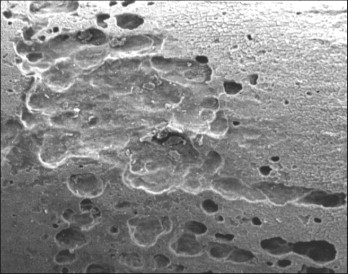
This process is progressive until the necrotic lesions are removed, finally permitting the tooth to move. Presumably, if new PDL necrotic lesions were generated at the same site after movement or reactivation of the appliance, progression of the root resorption would continue. This is consistent with the clinical impression that, in the absence of other inflammatory lesions, the progression of orthodontic root resorption ceases when orthodontic treatment ceases. It also may explain why patients with long durations of treatment or those requiring significant root movements are at risk for more extensive root resorption lesions; most likely these types of treatments require more appliance activations with greater risk of focal necroses in the PDL.
Only limited healing potential exists once a root resorption lesion has been created. Most cemental craters can repair completely with secondary cementum, but loss of root length or gross changes in root morphology do not entirely repair. Instead, restoration of these larger lesions does not proceed beyond their becoming lined with secondary cementum.
The most common radiographic image of orthodontic root resorption is loss of root length from the apex. Because of the prevalence of this clinical picture, the descriptive term external apical root resorption (EARR) has begun to appear in the root resorption literature. If the histological evidence links orthodontic root resorption to sites of compression, one must ask, “Why is apical root resorption so common?” Several possible explanations exist. First, root apices are common sites of compression in modern orthodontic mechanical approaches, including tipping, torque, and intrusion. Second, tooth structure is minimal at the root apex, which means these sites are more prone to morphological change with less loss of tissue. Third, standard radiographs easily visualize the root apex but not root loss from the lateral root surface because much (on buccal and lingual aspects) is not visible. However, autopsy sections from orthodontic patients and sections prepared from extracted premolars with orthodontic treatment clearly demonstrate that resorption sites are not found exclusively at the apex.
The sequelae of orthodontic root resorption range from being clinically insignificant or minor to severe enough to jeopardize the longevity of the dentition. Cases of minor root loss (<2 mm) are common and have no clinical consequences. However, persistent tooth mobility is a risk in teeth that lose significant root length. Therefore close follow-up of those teeth is indicated to prevent loss of crestal alveolar bone height. There are no good data on the prevalence of actual tooth loss as a result of severe orthodontic root resorption, but anecdotal clinical reports suggest this outcome is extremely rare.
EPIDEMIOLOGY
The prevalence of EARR varies among the different tooth types. Maxillary central incisors are most commonly affected. The reasons for this finding are not well understood. It is possible that the morphological or biological composition of these teeth make them highly prone to root loss or that they more often require orthodontic mechanics that put them at risk. Certainly the latter is likely considering that Class II and III malocclusions represent significant problems requiring orthodontic treatment, often with greater root movements and higher torquing forces to correct overjets. Maxillary incisors also may be more prone to lateral traumatic forces from mastication, putting them at risk for root loss before and during orthodontic treatment.
The prevalence of EARR in nonorthodontic patients is low (1%-2%) and is probably related to minor traumatic lesions or occlusal interferences. By contrast, the prevalence in orthodontic patients has been reported as high as 70%, strongly suggesting that the minor periodontal ligament (PDL) trauma associated with orthodontic treatment is a significant contributing factor. Most orthodontic patients experience clinically insignificant EARR (<2 mm). However, 2% to 5% experience greater than 5 mm of loss in root length.
Therefore most orthodontic patients who experience root shortening do not have clinically significant sequelae. The important subpopulation of orthodontic patients is the 2% to 5% who do experience enough root loss to constitute a clinical problem. Because modern orthodontic appliances and approaches are similar, it is difficult to see how these patients are experiencing unusual orthodontic treatments that alone are causing greater root loss. Assuming this is the case, it follows that the patients who experience severe EARR are more susceptible to the minor PDL traumas associated with orthodontic treatment caused by host, not environmental, factors.
EPIDEMIOLOGY
The prevalence of EARR varies among the different tooth types. Maxillary central incisors are most commonly affected. The reasons for this finding are not well understood. It is possible that the morphological or biological composition of these teeth make them highly prone to root loss or that they more often require orthodontic mechanics that put them at risk. Certainly the latter is likely considering that Class II and III malocclusions represent significant problems requiring orthodontic treatment, often with greater root movements and higher torquing forces to correct overjets. Maxillary incisors also may be more prone to lateral traumatic forces from mastication, putting them at risk for root loss before and during orthodontic treatment.
The prevalence of EARR in nonorthodontic patients is low (1%-2%) and is probably related to minor traumatic lesions or occlusal interferences. By contrast, the prevalence in orthodontic patients has been reported as high as 70%, strongly suggesting that the minor periodontal ligament (PDL) trauma associated with orthodontic treatment is a significant contributing factor. Most orthodontic patients experience clinically insignificant EARR (<2 mm). However, 2% to 5% experience greater than 5 mm of loss in root length.
Therefore most orthodontic patients who experience root shortening do not have clinically significant sequelae. The important subpopulation of orthodontic patients is the 2% to 5% who do experience enough root loss to constitute a clinical problem. Because modern orthodontic appliances and approaches are similar, it is difficult to see how these patients are experiencing unusual orthodontic treatments that alone are causing greater root loss. Assuming this is the case, it follows that the patients who experience severe EARR are more susceptible to the minor PDL traumas associated with orthodontic treatment caused by host, not environmental, factors.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


