Despite the different orthodontic treatment options for patients with Class II subdivision malocclusions, the involvement of the skeletal structures is significant. It is desirable to combine orthodontic and surgical treatment to achieve a stable and better esthetic result, as illustrated in this case report. The occlusal plane was canted to the right as a part of the patient’s facial asymmetry. Consequently, a 3-mm differential impaction of the maxilla on the left side allowed occlusal plane leveling. Mandibular rotation with advancement on the right side corrected the right Class II malocclusion. The successful attainment of the treatment goals was accomplished through teamwork and integration between the orthodontist and the maxillofacial surgeon.
Facial asymmetries can have dental, functional, or skeletal causes (resulting from discrepancies in shape or position of at least 1 bone of the craniofacial complex) or a combination of factors.
The main causes of mandibular lateral deviation are (1) genetic or congenital malformations (eg, hemifacial microsomia or unilateral cleft lip and palate); (2) environmental factors (eg, habits and trauma); (3) functional deviations (eg, mandibular shifts caused by tooth interferences); (4) posterior discrepancy with unilateral eruption space deficiency in the posterior area, which could lead to supereruption of the molars; (5) other causes (eg, poor dental reconstructions, such as asymmetric height of the restorative material on the left and right sides), temporomandibular joint arthrosis, and so on.
The degree of the subsequent jaw deformity depends not only on the type, intensity, extent, and chronology of the noxious agent, but also on the site and its particular involvement in growth activity. Class II subdivision malocclusions can be corrected through a variety of treatment protocols, depending on the etiologic factors that produce the asymmetric dentoalveolar characteristics of the malocclusion. However, when there are also severe skeletal components associated with that malocclusion, such as a vertical growth pattern and a retruded mandible, a combined surgical approach is often the best treatment option.
In this case, the patient had a right Class II subdivision malocclusion, an upwardly canted occlusal plane on the affected side, and a highly compensated occlusion. Orthodontic treatment and orthognathic surgery were used to level the occlusal plane and reposition the mandible.
Diagnosis and etiology
The patient was a 28-year-old woman. Her chief concerns were her asymmetric face, retrognathic mandible, malpositioned teeth, and asymmetric appearance of her anterior teeth. The intraoral photographs showed Class I molar and canine relationships on the left side and Class II molar and canine relationships on the right. There was a midline discrepancy of about 5 mm, with a 1.5-mm maxillary dental midline deviation to the left and a 3.5-mm mandibular dental deviation to the right. There was no crowding in either dental arch. There was labial tipping of the maxillary anterior teeth, with a deep overbite of 7 mm. The occlusal plane was canted upward on the affected side. The maxillary and mandibular arches were narrow because of the lingual tipping of the teeth ( Figs 1 and 2 ).

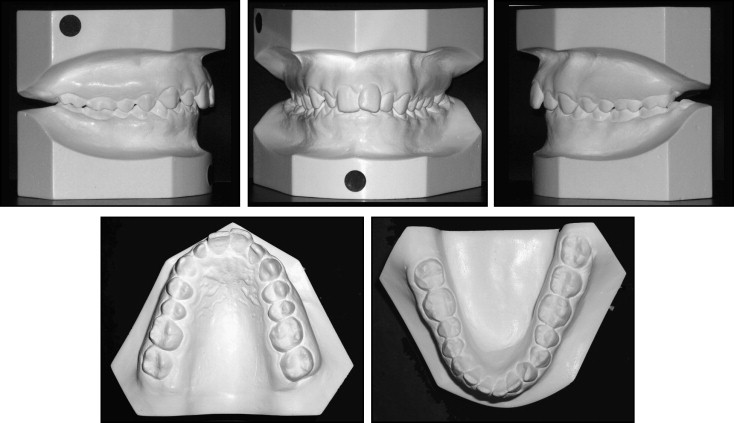
When the maxillary and mandibular dental midlines were aligned on the dental casts, a complete crossbite on the right side and a complete scissors-bite on the left side were created.
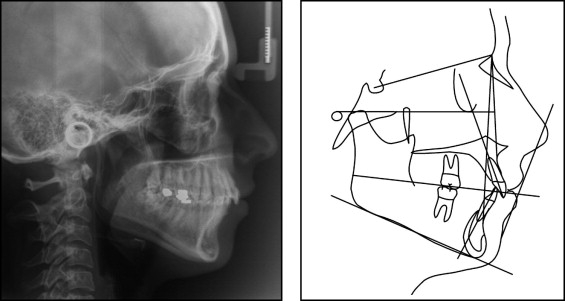
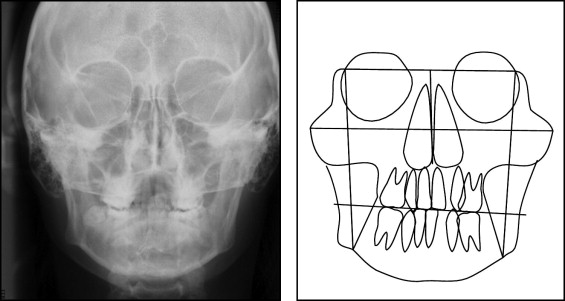
The panoramic radiograph showed that all third molars were present ( Fig 3 ). The lateral cephalometric analysis showed a normal mandibular plane angle, a skeletal Class II malocclusion with slight retrusion of the maxilla, and a retrusive mandible ( Table , Fig 4 ). A frontal cephalometric analysis confirmed the canted occlusal plane with compensatory tooth tipping and angulation of the posterior teeth ( Fig 5 ).

| Measurement | Norm | Pretreatment | Posttreatment |
|---|---|---|---|
| FMIA | 67° ± 3° | 62.1° | 64.0° |
| FMA | 25° ± 3° | 23.5° | 17.4° |
| IMPA | 88° ± 3° | 94.4° | 98.6° |
| SNA | 82° ± 2° | 77.2° | 78.6° |
| SNB | 80° ± 2° | 71.4° | 76.0° |
| ANB | 1°-5° | 5.9° | 2.7° |
| Ao Bo | 2 ± 2 mm | 4.5 mm | −1.4 mm |
| UI/NA | 22° ± 2° | 16.7° | 24.5° |
| Occlusal plane | 8°-12° | 6.4° | 3.5° |
| Z-angle | 75° ± 5° | 70.5° | 86.3° |
| Posterior facial height | 45 mm | 50.8 mm | 53.4 mm |
| Anterior facial height | 65 mm | 74.7 mm | 75.8 mm |
| Index post ant | 0.69 | 0.7 | 0.7 |
| Overjet | 2.5 ± 2.5 mm | 5.9 mm | 2.6 mm |
| Overbite | 2.5 ± 2.5 mm | 6.9 mm | 1.6 mm |
| Interincisal angle | 126° ± 10° | 132.4° | 125.3° |
Treatment objectives
The treatment objectives for this patient were reorientation of the occlusal plane, decompensation of dental arch tipping, improvement of facial and smile symmetry by surgical impaction of the left side of the maxilla, and correction of the mandibular retrognathia by forward and left repositioning of the mandible.
Treatment objectives
The treatment objectives for this patient were reorientation of the occlusal plane, decompensation of dental arch tipping, improvement of facial and smile symmetry by surgical impaction of the left side of the maxilla, and correction of the mandibular retrognathia by forward and left repositioning of the mandible.
Treatment alternatives
Based on the objectives, we could have chosen to reorient the occlusal plane using a multiloop edgewise archwire. However, this would not correct the position of the maxilla and would not improve the retrognathic mandible. Consequently, no improvement of the asymmetric gummy smile could be expected. An asymmetric maxillary impaction could significantly improve the gummy smile. Since the facial asymmetry, gummy smile, and retrognathic mandible were the patient’s major concerns, an orthodontic-orthognathic surgical treatment plan was chosen.
Preoperative orthodontic treatment
To assist in the correction of the posterior discrepancy and to facilitate the mandibular surgery, all third molars were extracted 12 months before the surgery. A multi-bracket straight-wire appliance (0.022-in slot) was bonded to all teeth. The orthodontic treatment during the first stage was for alignment and leveling to correct the tooth compensations in the maxillary and mandibular arches.
Despite the difference in height of the occlusal plane, the mandibular dental midline was centered with the mandible. Positioning the dental casts with the dental midlines coincidently produced a complete crossbite on the right side and a complete scissors-bite on the left side. To improve the transverse maxillary compensation, we applied a heavy archwire with torque and offsets or insets in the lateral and posterior areas (corono-vestibular with an offset for the maxillary right and mandibular left segments; corono-lingual with an inset for the maxillary left and mandibular right sides).
Photographs ( Fig 6 ) and radiographs ( Fig 7 ) were taken as soon as the patient was fully decompensated, and we had obtained our orthodontic treatment goals.


Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


