http://evolve.elsevier.com/Haveles/pharmacology
The dental hygienist is the first professional patients visit when they notice a lesion in the oral cavity. Patients often ask the dental hygienist and dentist, “What is this? How do I get rid of it? How long will it take to go away? Why do I have it? Is it cancer?” Patients who have even visited several physicians may appear at the office with commonly seen oral lesions. The first step is the diagnosis. Obtaining an in-depth history of the problem (by listening and asking open-ended questions) and examining the lesion can often result in a diagnosis or potential diagnoses. Depending on the diagnosis, the lesion may require only reassurance, palliative treatment, specific treatment, or even surgical intervention.
This chapter discusses a few of the more common oral lesions and the medications used for their treatment. Before individual oral lesions are discussed, commonly used treatments for several types of lesions are described.
Infectious lesions
Acute Necrotizing Ulcerative Gingivitis
Acute necrotizing ulcerative gingivitis (ANUG), which is also called Vincent’s infection and trench mouth, has both bacteriologic (spirochetes) and environmental (stress, debilitation) factors (Figure 12-1). ANUG is a spreading ulcer associated with a distinctive odor; the ulcerated area begins at the interdental papillae. The main symptoms are painful bleeding gums and ulceration of the interdental papillae. It is classified as a necrotizing periodontal disease along with necrotizing ulcerative periodontitis. The severe gingival pain that occurs with ANUG distinguishes it from the more common chronic periodontitis, which is not painful. ANUG is the acute form of necrotizing ulcerative gingivitis (NUG), which is the usual course of the disease. If not properly treated or neglected it can become chronic and/or recurrent.

Good oral hygiene is the cornerstone of treatment, but other modalities have been recommended. Mouthwashes, such as hydrogen peroxide, or saline rinses assist through their flushing action. If pain or an elevated temperature accompanies ANUG, aspirin, nonsteroidal antiinflammatory drugs, or acetaminophen can be recommended. If eating is difficult, food supplements, such as Meritene, Sustacal, or Sustagen, may be used instead of meals. Vitamin supplementation is useful only if the patient has a vitamin deficiency. The food supplements mentioned contain the required vitamins and minerals. Antibiotics should be considered only if the patient is immunosuppressed or there is evidence of systemic involvement (see Table 7-1). Antibiotics useful for the immunosuppressed patient with ANUG include penicillin VK and metronidazole. Topical chlorhexidine gluconate, which is active against gram-positive and gram-negative organisms and Candida organisms, is used as a rinse for ANUG. The majority of ANUG cases respond dramatically to local treatment (oral prophylaxis with scaling).
Herpes Infections
Primary herpetic gingivostomatitis (Figure 12-2), or primary herpes, is the manifestation of the initial herpes infection. Occurring principally in infants and children, it is caused by the herpes simplex virus (HSV). Because it is often associated with or follows other infections, it is also known as a fever blister or cold sore. The painful lesions may appear throughout the oral mucosa. Beginning as an erythematous area, numerous ulcers with a circumscribed area of erythema appear. The ulcers can coalesce to form larger irregular ulcers with gray centers. Other signs of herpes include the formation of vesicles that become scabbed. Systemic symptoms that are more severe in infants can develop and, in some cases, can be life threatening.



Without treatment, herpes is self-limiting in the patient with normal immunity. Approximately 80-90% of the adult population has been exposed to HSV. HSV-1 is involved in most oral lesions, and transmission is usually not sexual. HSV-2 is usually responsible for genital herpes and is transmitted sexually. Both HSV-1 and HSV-2 can spread to other parts of the body, for example, the eyes, genitals, and fingers (herpetic whitlow). When the lesions are in the vesicle stage, they are contagious, and the virus can survive for several hours on surfaces (one should think about possibilities in the dental office).
After the primary episode, the patient may experience recurrent outbreaks (cold sores or fever blisters) that occur at irregular and variable intervals. Events that may precipitate a herpetic outbreak include sunlight (ultraviolet light), hormonal changes such as menstruation, lip pulling, a rubber dam, biting an anesthetized lip, emotional stress, and other infections (e.g., a viral respiratory infection). According to the Centers for Disease Control, patients with active herpetic lesions receive dental treatment provided that either emergency dental care is required or the treatment is for the lesions only. All other care should be delayed until the lesions have healed. If the patient requires care, one should repeatedly apply a nonpetroleum lubricant to the lips and should be careful when manipulating the lips to minimize the trauma from a dental appointment. The effectiveness of the antiviral drugs varies depending on whether the outbreak is a primary episode or recurrence and whether the patient is immunocompromised or not.
Treatment
The treatment of herpes may include an antiviral agent, depending on the patient and the episode. Most instances of herpes simplex can be treated with symptomatic measures.
Symptomatic treatment of lesions includes swishing the mouth with topical diphenhydramine (DPH) (Benadryl) elixir or viscous lidocaine and spitting it out. Antiviral agents, such as acyclovir, valacyclovir, and penciclovir, are useful in certain herpes simplex infections (Table 12-1). Docosanol is another antiviral that is available without a prescription.
Table 12-1
Dosing of FDA-Approved Antiviral Agents in the Management of Herpes Labialis
| Drug | Indication | Dosing |
| Acyclovir topical cream (Zovirax) | Treatment of recurrent herpes labialis in adults and adolescents 12 years and older | Apply 5 times a day for 4 days |
| Acyclovir systemic ointment (Zovirax) | Treatment of herpes labialis in immunocompromised patients | Apply q3h,for a total of 6 times a day while awake, for 7 days |
| Valacyclovir systemic (Valtrex) | Treatment of herpes labialis | 2 g orally every 12 hours for 1 day |
| Famciclovir (Famvir) | Treatment of herpes labialis in adults | 1500 mg oral in a single dose |
| Penciclovir topical (Denavir) | Recurrent herpes labialis in immunocompetent patients | Apply every 2 hours while awake for 4 days |
| Docosanol 10% topical cream (Abreva) | Nonprescription treatment for herpes labialis | Apply 5 times daily |
FDA, U.S. Food and Drug Administration.
Acyclovir
Acyclovir is available in tablet, capsule, oral suspension, ointment, cream, and parenteral forms. This discussion is limited to the oral and topical products; parenteral products are not discussed in depth.
The approved indications for oral acyclovir include the treatment of primary and recurrent HSV in the immunocompromised patient. In the nonimmunocompromised patient, oral acyclovir is indicated for both treatment of the primary (first episode) outbreak and prophylaxis. Used prophylactically, it reduces the number and severity of recurrent outbreaks. Acyclovir should not be used prophylactically to prevent minor outbreaks because excessive use may lead to resistant strains of herpes.
Administration of oral acyclovir can be used before situations known to precipitate herpes lesions, such as a ski trip or wedding (stress), or a dental appointment that will produce trauma. The usual prophylactic dose of acyclovir is 400 mg twice a day (bid). It has yet to be shown that oral acyclovir has a significant clinical effect in the treatment of recurrent lesions in the immunocompetent patient. It may shorten the time to healing or the pain by a small amount.
Topical acyclovir ointment does not affect the course of recurrent herpes in the immunocompetent patient. This may be a result of poor penetration or delay in applying the ointment. Cell damage may be irreversible by the time symptoms are noticed. Topical acyclovir cream was recently approved to treat herpes labialis in immunocompetent patients.
The incidence of resistance of the herpes organisms to acyclovir is increasing. If herpes lesions fail to respond to therapy, the virus should be tested for susceptibility to acyclovir. Resistant strains have been identified, especially in patients who test positive for human immunodeficiency virus (HIV) are on long-term acyclovir therapy. This is the same principle that produces antibiotic resistance in the general population.
Penciclovir
Penciclovir (Denavir), which is available only topically, has been shown to reduce by one-half day the duration and pain of lesions on the lips and face associated with both primary and recurrent herpes simplex. The advantages of penciclovir over acyclovir are that penciclovir can achieve a higher concentration within the cell and that it remains in the cells longer. Table 12-1 summarizes the indications for the antiviral agents.
Docosanol (Abreva)
Docosanol is the only antiviral drug available without a prescription to treat recurrent herpes simplex virus. It is available as a topical 10% cream and should be applied at the first sign of symptoms. It has been shown to reduce the duration by about one half day in patients with recurrent herpes simplex virus.
Famciclovir and valacyclovir
Both famciclovir and valacyclovir are prodrugs that are converted to active antiviral agents. They are indicated in the treatment of acute localized varicella-zoster infections and recurrent genital herpes in immunocompetent adults. Valacyclovir is also indicated for the treatment of herpes labialis. Ganciclovir is indicated for serious cytomegalovirus retinitis in immunocompromised patients. It may be effective in some acyclovir-resistant organisms.
Treatment of symptoms
Palliative treatment involves treating the patient’s symptoms. In a primary episode of herpes, fever may be managed by the administration of acetaminophen or by sponging the affected area with tepid water. The discomfort associated with herpes may be relieved by swishing diphenhydramine. This product is available under many trade names, for example, Diphen Cough, Diphenhist, Genahist, and Siladryl. All of these products are alcohol-free liquids. Perhaps the most commonly available proprietary product is Benadryl. The strength of all the products is 12.5 mg of the active ingredient per 5 ml (1 teaspoonful). Other agents, such as viscous lidocaine (Xylocaine) and combinations of diphenhydramine with kaolin (Kaopectate), calcium carbonate (Maalox Quick Dissolve), and simethicone (Mylanta Gas), are recommended for use in the oral cavity. Because antihistamines, such as diphenhydramine, are similar in structure to local anesthetics, they have some local anesthetic action and can therefore reduce the pain.
Sodium carboxymethylcellulose paste (Orabase plain or with benzocaine) may reduce discomfort. Food supplements may be used if intake of food is impossible (because of oral discomfort). These remedies are the same as those used for patients receiving cancer chemotherapy agents. Corticosteroids are contraindicated because they suppress the cellular immunity that inhibits viral infections.
Candidiasis (Moniliasis)
Candidiasis, a fungal infection caused by Candida albicans, often affects the oral and vaginal mucosa. Candidiasis occurs when the organisms multiply and predominate. Because Candida is part of the normal oral flora, it is always present in small numbers. When other flora are suppressed, Candida can predominate.
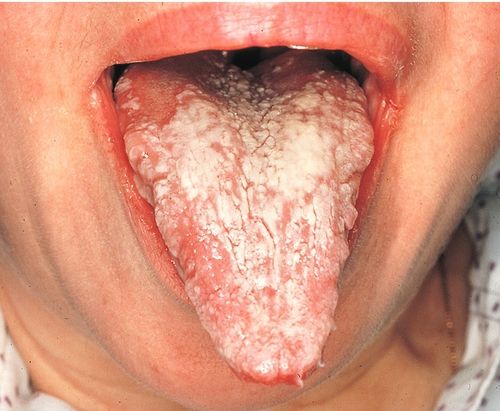
When a patient presents with oral candidiasis, it is important that the dental health care worker search exhaustively for potential predisposing factors. Systemic antibiotic treatment, especially with broad-spectrum antibiotics such as tetracycline, can predispose a patient to candidiasis. A dental health care worker may be the first professional to diagnose HIV-positive patients or those with acquired immunodeficiency syndrome (AIDS) (Figure 12-3).

Although candidiasis can appear in several different forms, the lesions are typical and can usually be diagnosed from their clinical appearance. They may be confirmed by culture. Topical products available to treat oral candidiasis include nystatin products (aqueous suspension, vaginal tablets [used as lozenges], and lozenges [pastilles]), and clotrimazole troches (see Chapter 8).
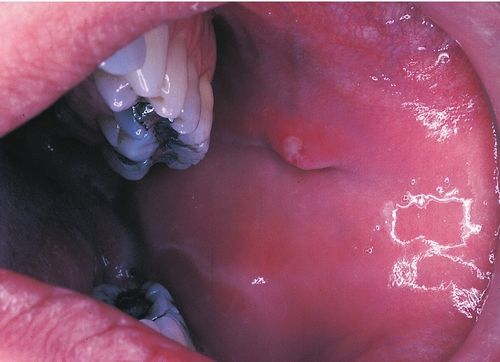
With chronic candidiasis (Figure 12-4), ketoconazole tablets taken orally once daily can be used. Systemic alternatives include either fluconazole or itraconazole. All are effective, but they should be continued for at least 2 weeks and/or at least 2 or 3 days past the time when the symptoms have disappeared.
Angular Cheilitis/Cheilosis
Angular cheilitis appears as simple redness, fissures, erosion, ulcers, and crusting located at the angles of the mouth, which may or may not be painful (Figure 12-5). Most cases of cheilitis are associated with a mixed infection. Often C. albicans infection is present, and not uncommonly both Candida and gram-positive bacteria, such as streptococci and/or staphylococci, also invade the lesion.

Predisposing factors include moisture from drooling (moist areas are more likely to be infected with fungus). In the past, a decrease in vertical dimension of occlusion was thought to contribute to angular cheilitis, but later evidence has not shown this to be true.
Depending on the presentation of the patient’s lesion, therapy is addressed toward treating the secondary infection(s). If Candida organisms are present, treatment with an antifungal agent (see Chapter 8) is indicated. Examples of topical antifungal agents are nystatin, clotrimazole, and miconazole. If inflammation is present, some practitioners prescribe a combination of an antifungal agent mixed with a topical steroid (e.g., Mycolog [nystatin (Mycostatin) plus triamcinolone acetonide (Kenalog)]). One concern, which may or may not be clinically significant, about using steroids with a fungal infection is that steroids inhibit the inflammatory reaction associated with cellular immunity (this is the reaction that normally fights fungal infections).
If a bacterial overgrowth is suspected, the organisms responsible are usually similar to staphylococci and streptococci. To treat this bacterial infection, systemic penicillinase-resistant penicillins, such as dicloxacillin, are indicated (see Chapter 7). Mupirocin (Bactroban), is a topical antibacterial useful in the treatment of staphylococcal and streptococcal infections. Using mupirocin decreases the likelihood of adverse reactions, and mupirocin is as effective as systemic penicillinase-resistant penicillins (see Chapter 7). A topical antifungal agent and mupirocin can be used concomitantly if both are indicated.
Although rarely produced by a deficiency of vitamin B6 (pyridoxine) or B2 (riboflavin), cheilosis can result from deficiencies of these vitamins. Vitamin B supplements would be useful, but only if a vitamin deficiency exists.
Alveolar Osteitis
Alveolar osteitis, or “dry socket,” occurs in 2-3% of all tooth extractions, most commonly in the lower molar region, where the incidence is considerably higher than in other areas. Alveolar osteitis is thought to be caused by loss or necrosis of the blood clot that has formed in the extraction site, exposing the underlying bone. The exposed bone is severely painful. Predisposing factors include oral contraceptive use and menstrual cycle phase. Smoking, especially after extraction, can increase the likelihood of dry socket. Inhaling on a cigarette produces a negative pressure in the oral cavity that may dislodge the clot.
Infection, swelling, elevated temperature, lymphadenopathy, and a foul odor may be present. Treatment consists of rinsing with saline water and debridement, placement of a pack, analgesics, and supportive therapy. There is some indication that local placement of antibiotics may reduce the incidence of dry socket, but aseptic techniques, proper suturing techniques, and minimal trauma should be used as prophylactic measures. Most literature does not recommend the use of prophylactic antibiotics. If infection is present, antibiotics are indicated (as treatment not prophylaxis). Antibiotics may be indicated in patients at high risk for infection.
Immune reactions
Recurrent Aphthous Stomatitis
Recurrent aphthous stomatitis (RAS), which is sometimes referred to as a canker sore, is a common oral lesion occurring in about 20% of the population. It is seen in patients older than 20 years and has an unknown etiology, although an involvement of the immune system is suspected.
RAS manifests clinically as a few small to many large ulcers. The ulcers can even coalesce into giant ulcers. Although three distinct types have been clinically identified—minor, major, and herpetiforme—the most common form of aphthous ulcers is the minor type (Figure 12-6).

The etiology of aphthous stomatitis involves an immunologic component and may be associated with a focal immune dysfunction in which T lymphocytes play a significant role. The ratio of T-helper (CD4+) cells to T-suppressor/cytotoxic (CD8+) cells is decreased. An increase in the CD8+ cells is seen. The oral mucosa is destroyed by lymphocytes.
Many hypotheses have been advanced concerning the etiology of RAS, including the following: an allergenic/hypersensitivity reaction (endogenous [autoimmune], exogenous [hyperimmune]), genetic, hematologic, hormones, infection, nutrition, and nonspecific events such as trauma and stress. Another hypothesis is that it is a hypersensitivity reaction to the sodium lauryl sulfate present in many over-the-counter (OTC) products, including most toothpastes (Table 12-2).
Table 12-2
Toothpastes (Dentifrices) That Do Not Contain Sodium Lauryl Sulfatea
| Dentifrice | American Dental Association Approved? |
| Arm & Hammer Dental Care Baking Soda Tooth Powder | No |
| Platinum Whitening Toothpaste with Fluoride | No |
| Pycopay Tooth Powder | No |
| Sensodyne Gel, Cool Mint | No |
| Sensodyne-SC Toothpaste | Yes |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


