The focus in dentistry has gradually changed over the past 25 years. Dentists previously were in the “repair business.” Routine dental treatment involved excavating dental caries and filling the enamel and dentinal defects with amalgam. Larger holes may have required more durable restorations, but the focus was the same: repair the effects of dental decay.
With the advent of fluorides and sealants, however, in addition to a better understanding of the role of bacteria in causing both caries and periodontal disease, patient needs have changed. Many young adults, who are products of the sealant generation, have little or no decay and few existing restorations. At the same time, the image of the value of teeth in Western society has also changed. The public still regards teeth as an important part of chewing, but the focus of many adults has shifted toward esthetics. They ask, “How can my teeth be made to look better?” Therefore the formerly independent disciplines of orthodontics, periodontics, restorative dentistry, and maxillofacial surgery must often join together to satisfy this desire to “look better.”
This heightened awareness of esthetics has challenged dentistry to examine dental esthetics in a more systematic manner, to ensure that the health of patients and their teeth is still the most important underlying objective. Some existing dentitions simply cannot be restored to a more esthetic appearance without the assistance of several different dental disciplines. Every dental practitioner must now have a thorough understanding of the roles of these various disciplines in producing an “esthetic makeover,” using the most conservative and biologically sound interdisciplinary treatment plan possible.
As an orthodontist, the author has worked with an interdisciplinary study group of nine dental specialists and one general dentist since 1984. The group has met monthly to educate the members about the advances in their respective areas of dentistry and to plan interdisciplinary treatment for the most challenging and complex dental situations. One of these interdisciplinary areas is esthetics. The purpose of this chapter is to provide a systematic method of evaluating dentofacial esthetics in a logical, interdisciplinary manner.
SEQUENCING THE PLANNING PROCESS
Historically, the treatment-planning process in dentistry usually has begun with an assessment of the biology or biological aspects of a patient’s dental problem. This might include the patient’s caries susceptibility, periodontal health, endodontic needs, and general oral health. Once the biological health was reestablished through caries removal, modification of bone and gingiva, endodontic therapy, or tooth removal, the restoration of the resulting defects would be based on structural considerations. If teeth were to be restored or repositioned, the function of the teeth and condyles would be paramount in dictating occlusal form and occlusal relationships, respectively. Finally, esthetics would be addressed to provide a pleasing appearance of the teeth.
However, if the treatment-planning sequence proceeds from biology to structure to function and finally to esthetics, the eventual esthetic outcome could be compromised. The author proceeds in the opposite direction, starting with esthetics and proceeding to function, structure, and finally biology. None of the important parameters is left out; the planning process is merely sequenced from a different perspective. This sequence is chosen because the decisions made in each category, especially esthetics, will directly affect the subsequent categories.
BEGINNING WITH ESTHETICS
Maxillary Central Incisors Relative to Upper Lip
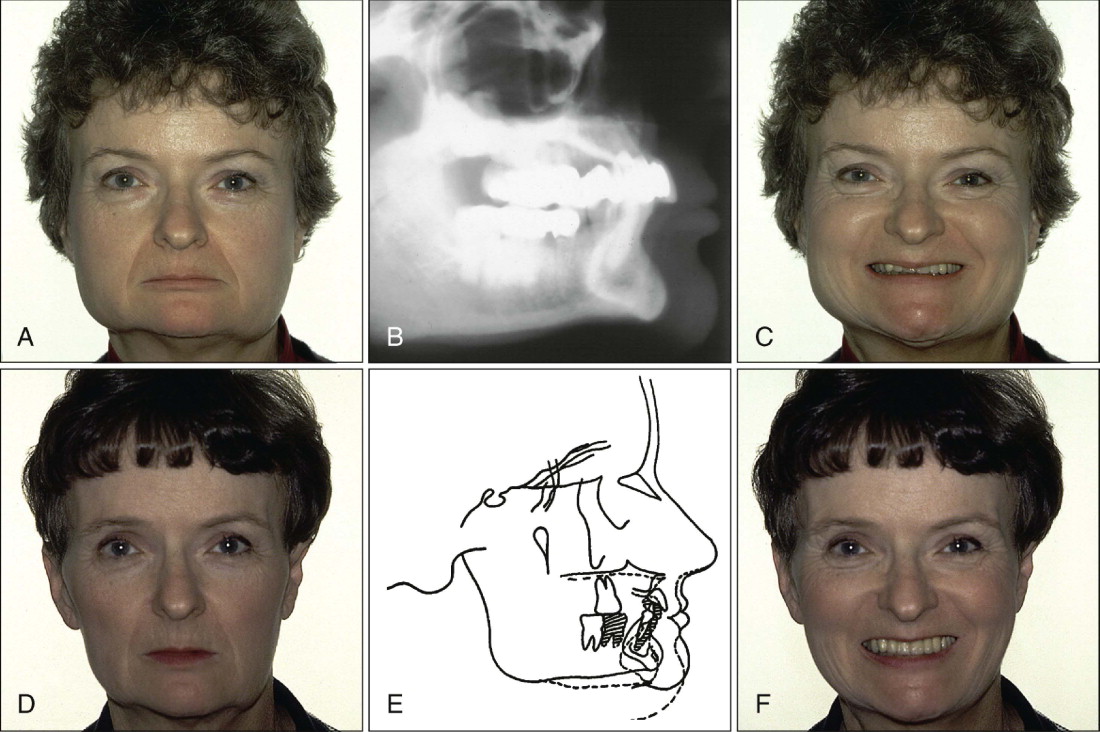
When beginning with esthetics, the first step is an appraisal of the position of the maxillary central incisors relative to the upper lip ( Fig. 21-1 ). This assessment is made with the patient’s upper lip at rest. Using a millimeter ruler or periodontal probe, the clinician determines the position of the incisal edge of the maxillary central incisor relative to the upper lip. The position of the maxillary central incisor can either be acceptable or unacceptable. An acceptable amount of incisal edge display at rest depends on the patient’s age. Previous studies have shown that with advancing age, the amount of incisal display decreases proportionately. For example, in a 30-year-old patient, 3 mm of incisal display at rest is appropriate, whereas in a 60-year-old patient, the incisal display could be 1 mm or less. The change in incisal display with time probably relates to the resiliency and tone of the upper lip, which tends to decrease with advancing age.
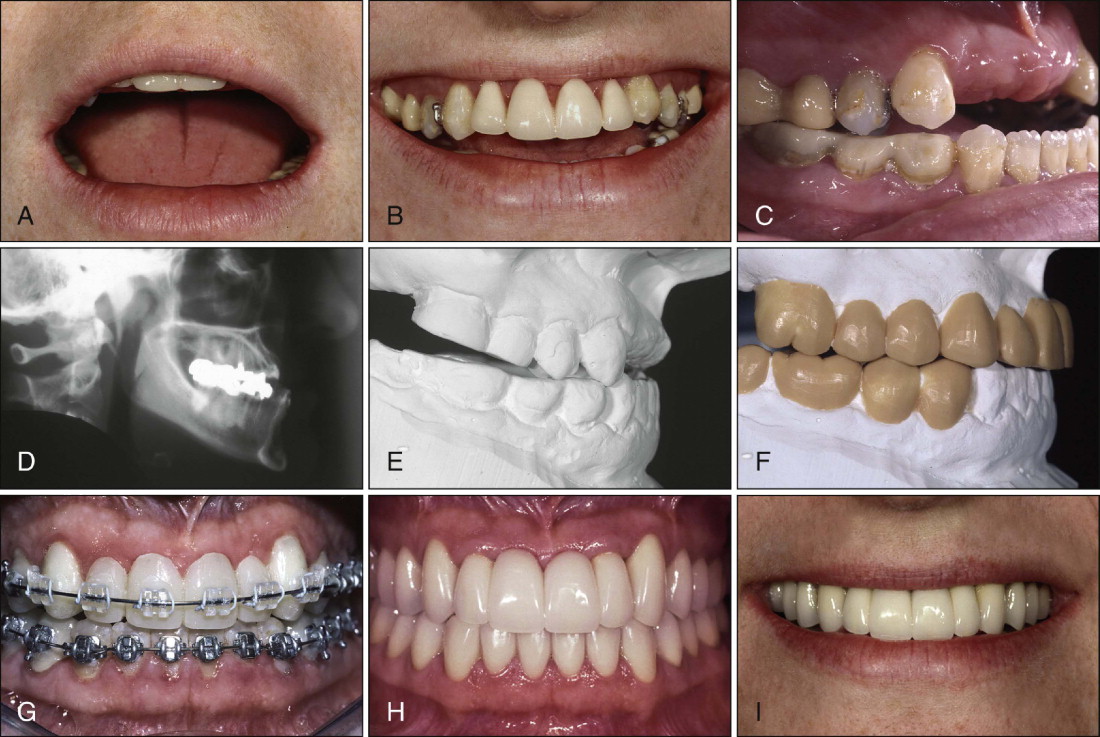
If the incisal edge display is inadequate ( Fig. 21-2 ), a primary objective of interdisciplinary treatment may be to lengthen the maxillary incisal edges. This objective can be accomplished with restorative dentistry, orthodontic extrusion, or orthognathic surgery ( Fig. 21-2 ). Choosing the correct procedure will depend on the patient’s facial proportions, existing crown length, and opposing occlusion. If the incisal edge display is excessive, an objective of treatment may be to move the maxillary incisors apically by equilibration, restoration, orthodontics, or orthognathic surgery. The treatment decision will depend on the patient’s existing anterior occlusion and the facial proportions.
Maxillary Dental Midline
The second aspect of esthetic tooth positioning to be evaluated is the maxillary dental midline. Recent studies have shown that laypeople do not notice midline deviations of up to 3 or 4 mm if the long axes of the teeth are parallel with the long axis of the face. Therefore the most important relationship to evaluate may be the mediolateral inclination of the maxillary central incisors. If the incisors are inclined by 2 mm to the right or left ( Fig. 21-3 ), laypeople regard this discrepancy as “unesthetic.” A canted midline can be corrected with orthodontics or restorative dentistry. Usually the decision depends on whether the maxillary incisors will require restoration.
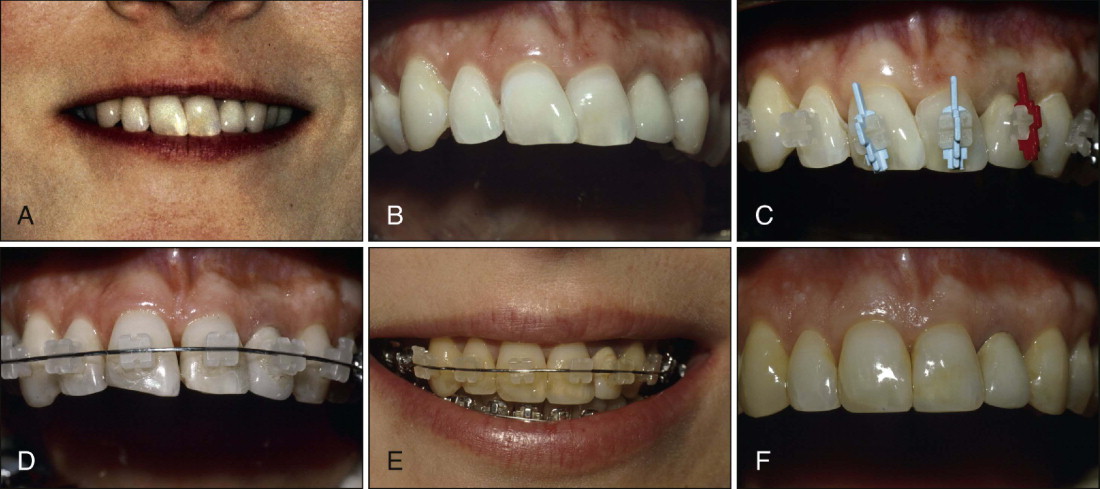
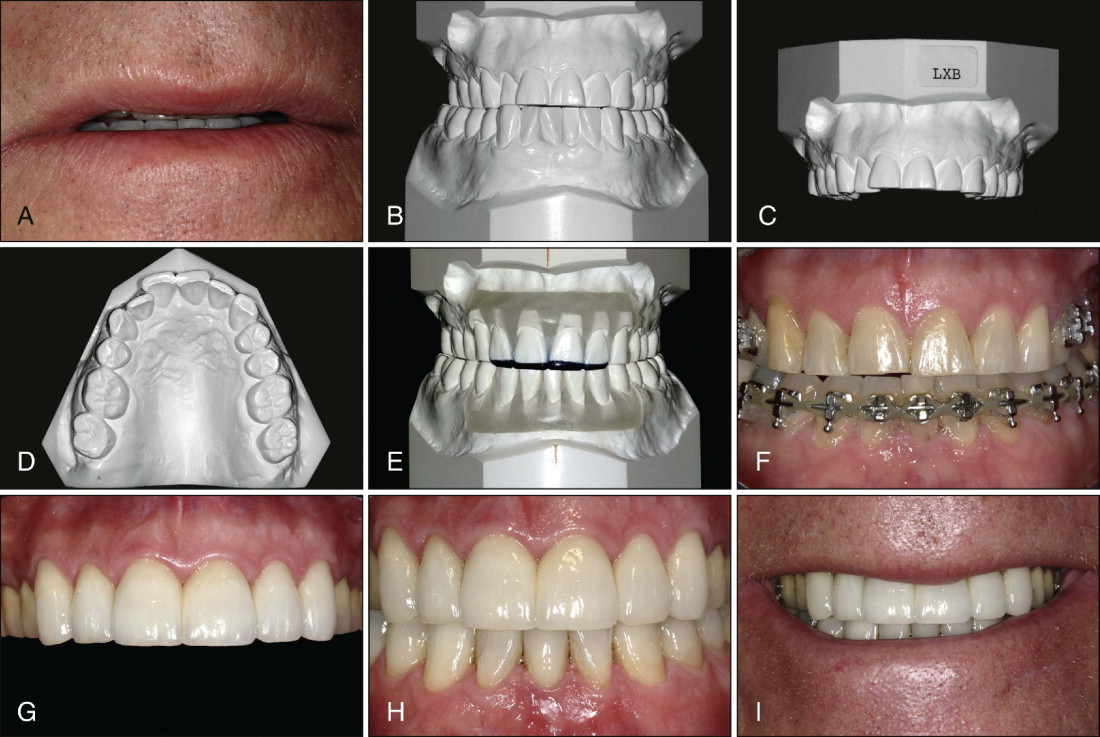
Maxillary Incisor Inclination and Posterior Occlusal Plane
Once the correct incisal edge position and midline relationship of the maxillary incisors has been established, the next step is to evaluate the labiolingual inclination of the maxillary anterior teeth. Are they acceptable, proclined, or retroclined? When orthodontists evaluate labiolingual inclination, they rely on cephalometric radiographs to determine tooth inclination. However, general dentists do not use cephalograms. Another method of assessing the inclination of the maxillary anterior teeth is to evaluate the labial surface of the existing maxillary central incisors relative to the patient’s maxillary posterior occlusal plane. Generally, the labial surface of the maxillary central incisors should be perpendicular to the occlusal plane ( Fig. 21-4 ). This relationship permits maximum direct light reflection from the labial surface of the maxillary central incisors, which enhances their esthetic appearance. If teeth are retroclined ( Fig. 21-5 ) or proclined ( Fig. 21-6 ), correction may require either orthodontics or extensive restorative dentistry and possibly endodontics to establish a more ideal labiolingual inclination.
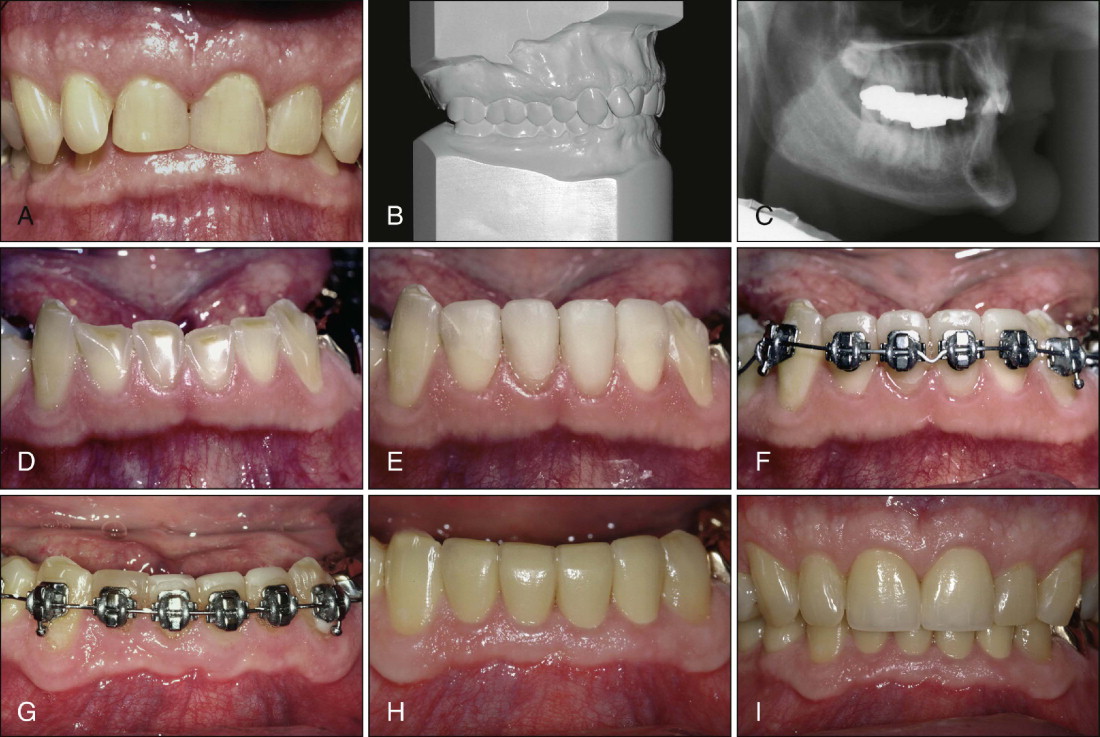
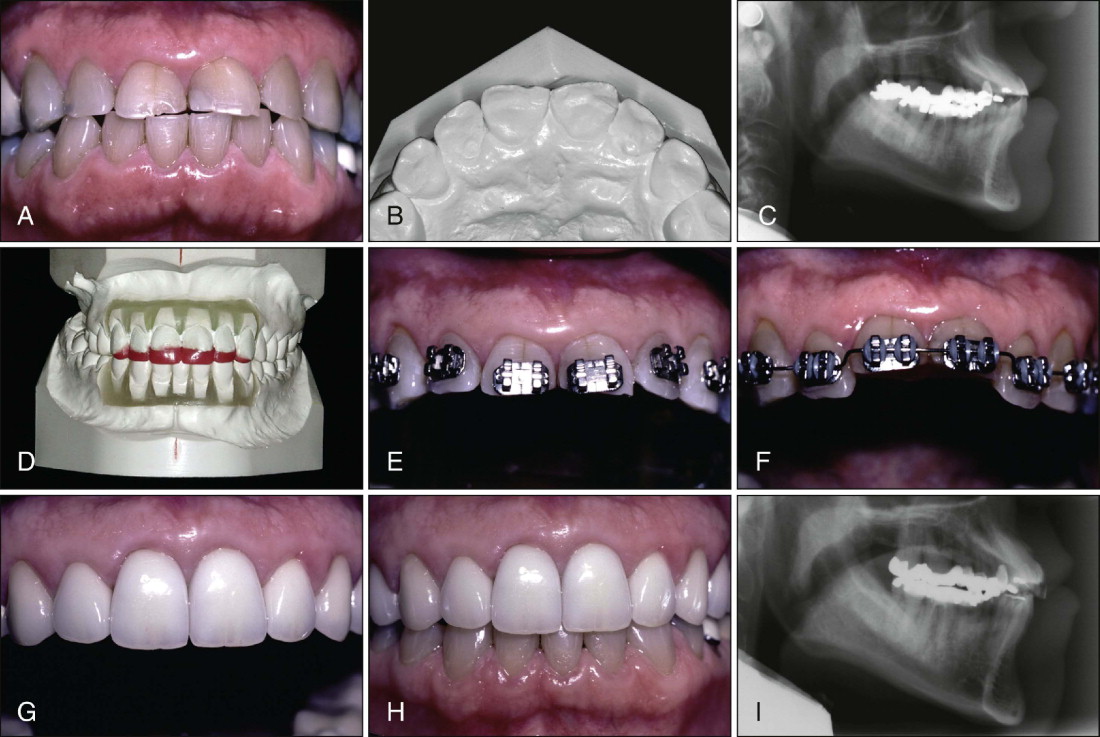
The next step is to evaluate the maxillary posterior occlusal plane relative to the ideal location of the maxillary incisal edge. The maxillary incisal edge will be level with the posterior occlusal plane (see Fig. 21-4 ), coronal to the posterior occlusal plane (see Fig. 21-1 ), or apical to the posterior occlusal plane (see Fig. 21-2 ). Correcting the posterior occlusal plane position will require orthognathic surgery (see Figs. 21-1 and 21-2 ) and/or restorative dentistry. The amount of tooth abrasion, the patient’s vertical facial proportions, and the position of the alveolar bone will help to determine the correct solution of posterior occlusal plane discrepancies.
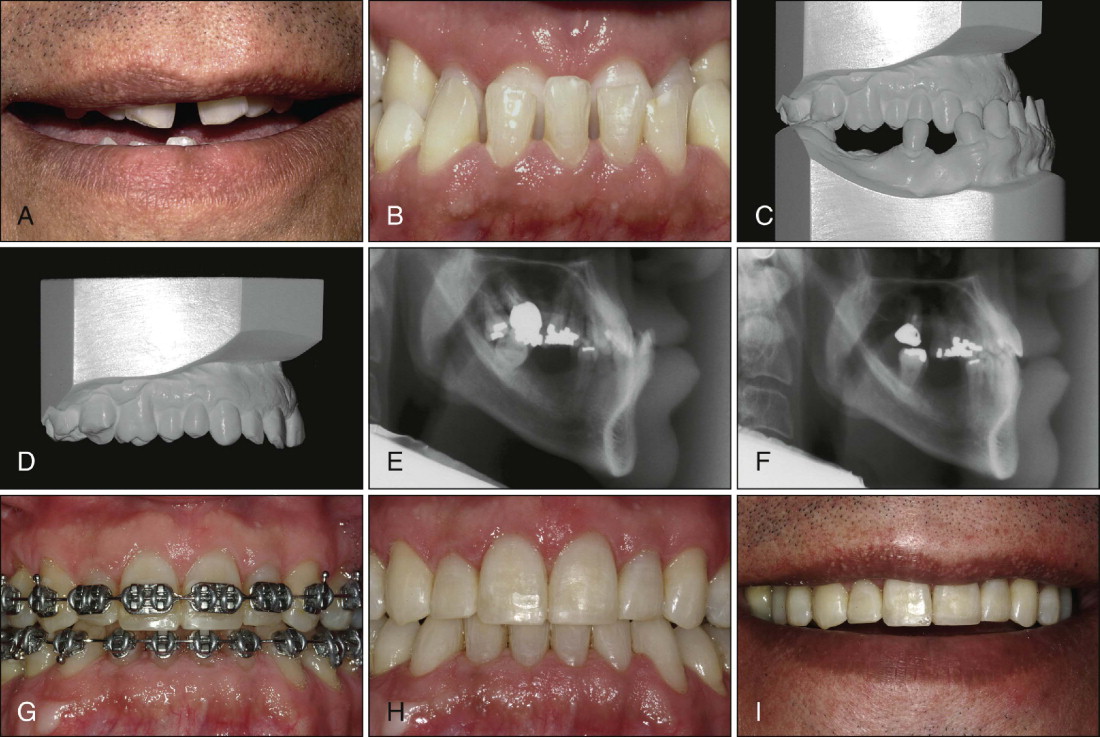
After the position of the maxillary central incisal edges have been determined, the incisal edges of the maxillary lateral incisors and canines, as well as the buccal cusps of the maxillary premolars and molars, can be established ( Fig. 21-7 ; see Fig. 21-4 ). The levels of these teeth generally are determined by their esthetic relationship to the lower lip when the patient smiles. If the patient has an asymmetric lower lip, it may be more prudent to use the interpupillary line as a guide in establishing the posterior occlusal plane.
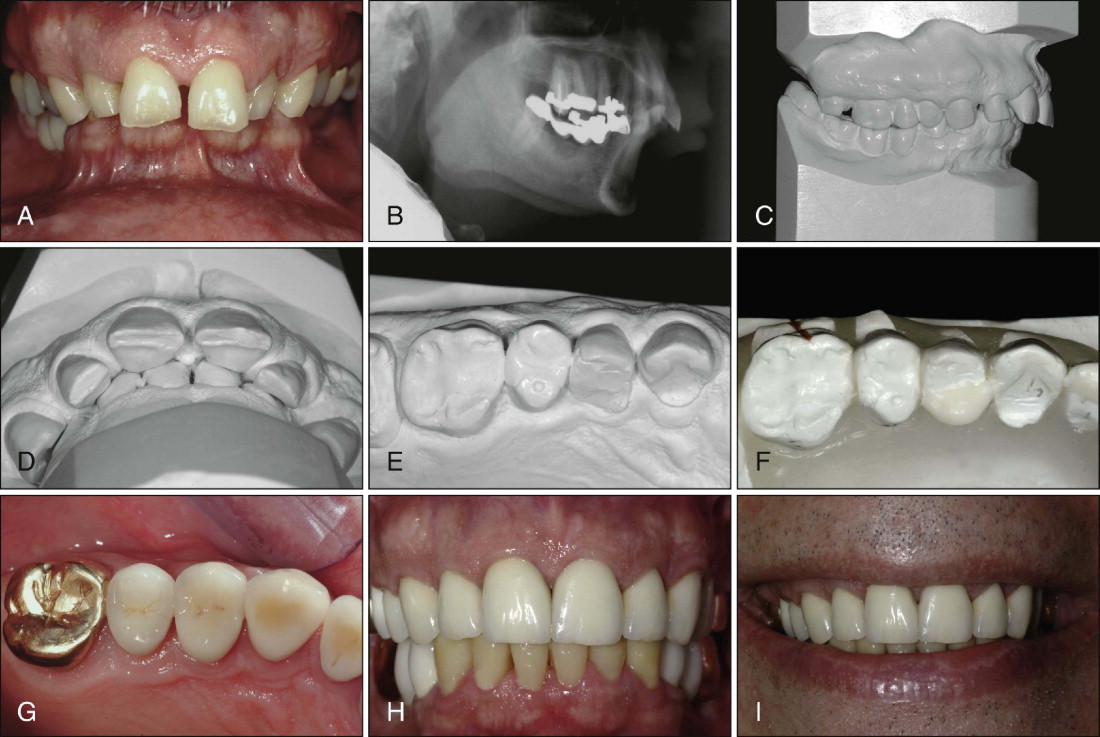
Gingival Levels
The next step in the process of determining the esthetic relationship of the maxillary anterior teeth is to establish the gingival levels. The current gingival levels should be assessed relative to the projected incisal edge position. The key to determining the correct gingival levels is to determine the desired tooth size relative to the projected incisal edge position ( Fig. 21-8 ). Remember, the incisal edge is not positioned to create the correct tooth size relative to the gingival margin levels. Using the gingiva as a reference to position the incisal edges is risky, because gingiva can move with eruption or recession. Thus the ideal gingival levels are determined by establishing the correct width/length ratio of the maxillary anterior teeth, the desired amount of gingival display, and symmetry between right and left sides of the maxillary dental arch.
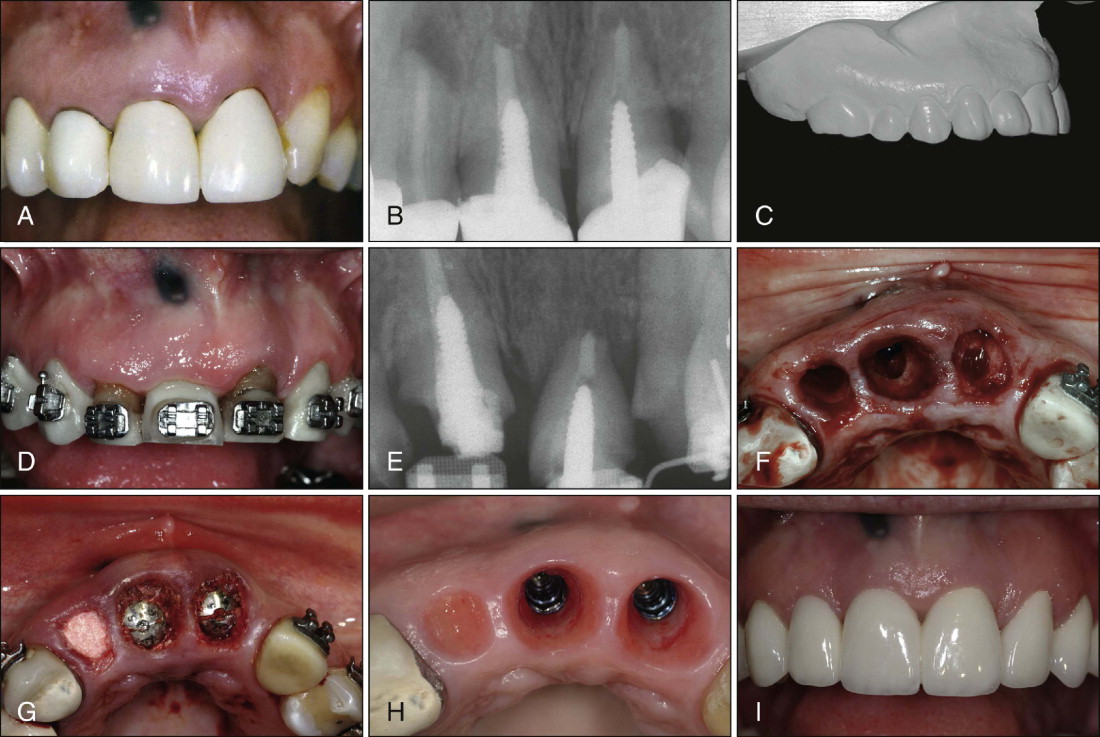
If the existing gingival levels will produce a tooth that is too short relative to the projected incisal edge position, the gingival margins must be moved apically ( Fig. 21-9 ). This adjustment can be accomplished with gingival or osseous surgery ( Fig. 21-9 ), orthodontic intrusion, or orthodontic intrusion and restoration (see Figs. 21-6 and 21-9 ). The key factors that determine the most appropriate method of correction are the sulcus depth, location of the cementoenamel junction relative to the bone level, amount of existing tooth structure, root/crown ratio, and shape of the root. In some situations, surgical crown lengthening of the maxillary incisors (see Fig. 21-9 ) is more appropriate to establish the correct gingival levels. In other situations, orthodontic intrusion (see Fig. 21-6 ) and restoration of the incisal edge are more appropriate.
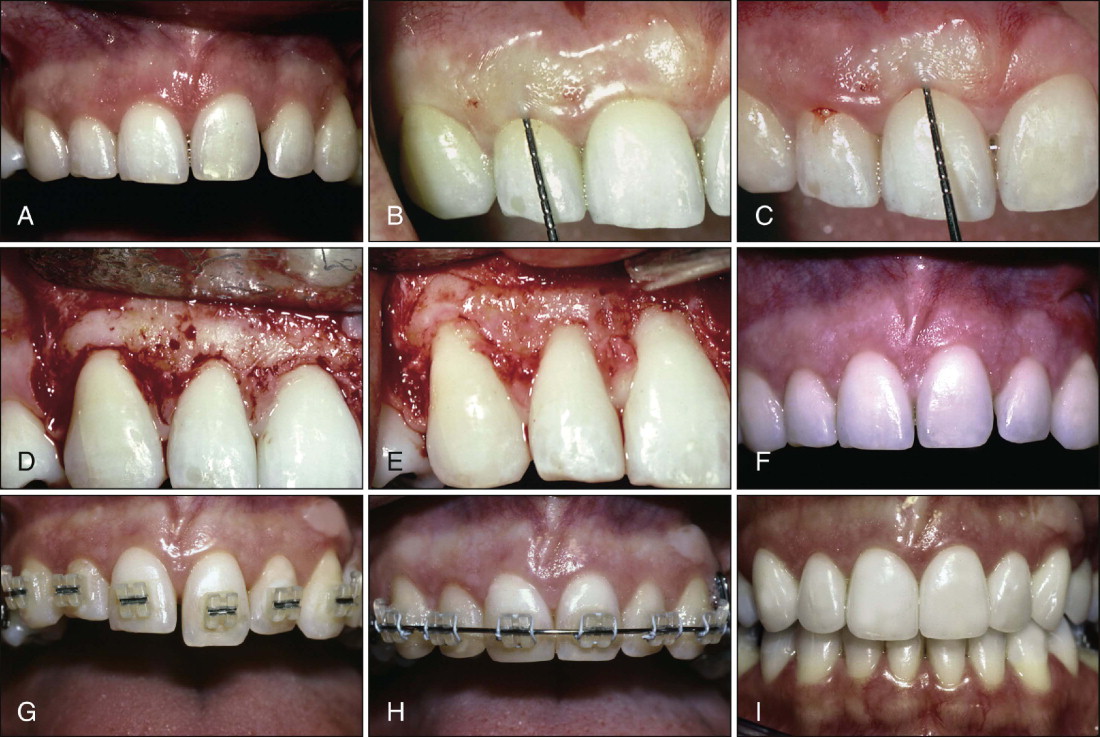
The next step in the process of establishing the correct esthetic position of the maxillary anterior teeth is to assess the papillary levels relative to the overall crown length of the maxillary central incisors. Research has shown that the average ratio is about 50% contact and 50% papilla. If the contact is significantly shorter than the papilla, it usually indicates moderate to significant incisor abrasion, which tends to shorten the crowns and therefore shortens the contact between the central incisors. If the contact is significantly longer than the papilla, the gingival contour or scallop over the central incisors might be flat, which could be caused by altered passive or altered active eruption of the teeth. Gingival or osseous surgery or orthodontic intrusion or extrusion ( Fig. 21-10 ) may be necessary to correct the level of the papillae between the maxillary anterior teeth.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


