This article describes a patient whose permanent canines and premolars had not erupted at age 14 years, although their root formation was complete, with closed apices. Surgical and orthodontic treatment was planned to correct the multiple impactions. The orthodontic traction used 5 strategic teeth and allowed for the eruption of all 12 impacted teeth. The surgical-orthodontic treatment of many impacted teeth yielded good esthetic and periodontal results, as shown by the patient’s satisfaction and the periodontal probing 2 years after the treatment. Multiple impacted teeth are a rare eruption disturbance that requires early detection: no signs of a genetic syndrome or an endocrine disorder had been found, or failure to move along the eruption path, which is a characteristic of another syndrome, primary failure of eruption.
Impacted teeth other than third molars can be a challenge for the orthodontist. A single impacted tooth can increase the complexity of the orthodontic treatment significantly, and multiple impactions certainly complicate the treatment and lengthen the overall treatment time considerably.
Maxillary canine impaction has an estimated incidence of 1 patient in 100 in the general population, but much higher incidences have been reported in some orthodontic practices. The estimated incidence of mandibular canine impaction is nearly 3.5 in 1000. Canine impaction is rarely associated with multiple impacted teeth; few reports have been published about such cases, with several teeth involved.
A relatively high incidence of impacted teeth and delayed eruption of deciduous and permanent teeth has been observed in patients with cleidocranial dysplasia. Patients with multiple impactions need careful orthodontic and surgical treatment planning: the cooperation with the surgeon is crucial to guide the eruption of as many useful teeth as possible.
This patient had no permanent canines or premolars erupted at age 14 years. The teeth were markedly inclined and had complete root formation with closed apices. The periodontal status was reevaluated 2 years after treatment.
Diagnosis and etiology
The patient, a 14-year-old girl, was in good physical and emotional health. Her chief complaint was having several deciduous teeth ( Figs 1–3 ). The panoramic radiograph shows the displaced permanent teeth. She had already been sent to a physician and an endocrinologist to investigate possible systemic factors, but no signs of any genetic syndrome or endocrine disorder had been found. The mandibular deciduous canines had been extracted by a general practitioner 1 year before, but the mandibular permanent canines failed to erupt. There had been no eruption problems in the family, according to her parents.

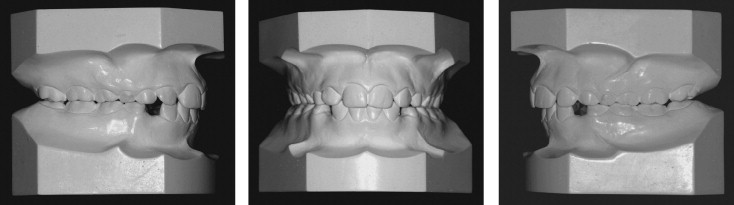

The clinical examination showed Class I molar relationships on both sides, associated with persistence of all deciduous molars and maxillary canines. Part of the space of the deciduous canines in the mandibular arch was lost a year after their extraction, whereas the mandibular permanent canines remained deeply impacted and partly covered by the first premolars.
The diagnosis of multiple impactions (12 teeth excluding the third molars) was based on the complete development of the roots (closed apices) of the unerupted and malpositioned permanent teeth and the persistence of many deciduous teeth without significant root resorption. The mandibular permanent canines had not erupted a year after the extraction of the deciduous ones, and eruption of the other retained permanent teeth was not expected to occur in a reasonable time. The cephalometric analysis showed that the maxilla was well positioned, but the mandibular plane angle was high (SNaGo-Gn, 39°); therefore, extrusion of the molars had to be prevented ( Fig 4 ).
Treatment objectives
The objectives of the orthodontic treatment were to guide the eruption of the 12 impacted teeth to a functional and stable occlusion, level and align the arches, obtain normal overjet and overbite, and achieve a bilateral Class I canine and molar occlusion.
Full fixed orthodontic therapy was proposed with oral surgery to expose and ligate the impacted teeth. We planned to extract a few teeth at a time to limit the damage in case of failure and maintain the second deciduous molars as intra-arch anchorage during the traction phase. They would be extracted only when the premolars and canines had erupted.
Sufficient oral hygiene and periodontal health, and willingness to cooperate and wear fixed appliances were obvious prerequisites: the patient was motivated and requested the treatment to proceed as quickly as possible. The parents were informed about the expected length of the treatment and the risk of lateral incisor root resorption. A consent form for alignment of impacted or ectopic teeth was signed at the first stage of treatment. The combined orthodontic-surgical treatment was first planned for the mandible.
Treatment objectives
The objectives of the orthodontic treatment were to guide the eruption of the 12 impacted teeth to a functional and stable occlusion, level and align the arches, obtain normal overjet and overbite, and achieve a bilateral Class I canine and molar occlusion.
Full fixed orthodontic therapy was proposed with oral surgery to expose and ligate the impacted teeth. We planned to extract a few teeth at a time to limit the damage in case of failure and maintain the second deciduous molars as intra-arch anchorage during the traction phase. They would be extracted only when the premolars and canines had erupted.
Sufficient oral hygiene and periodontal health, and willingness to cooperate and wear fixed appliances were obvious prerequisites: the patient was motivated and requested the treatment to proceed as quickly as possible. The parents were informed about the expected length of the treatment and the risk of lateral incisor root resorption. A consent form for alignment of impacted or ectopic teeth was signed at the first stage of treatment. The combined orthodontic-surgical treatment was first planned for the mandible.
Treatment alternatives
A simple treatment alternative of extracting just the deciduous teeth was not considered an effective option because of the expected loss of space and the poor estimated probability of spontaneous eruption. The mandibular permanent canines had not erupted 1 year after extraction of the deciduous canines, and eruption of the other retained permanent teeth was not expected in a reasonable time.
Uncovering the maxillary first premolars or the palatal canines before the start of the orthodontic treatment could be another alternative. Once the bone and tissue have been removed, these palatally displaced canines usually erupt in 6 to 8 months, resulting in facilitated orthodontic treatment. However, the impacted teeth were considered too deeply positioned, and a combined surgical and orthodontic approach was preferred.
The choice of surgical technique—closed eruption or open eruption—was based on the canine and pre-molar locations: the impactions were considered too deep for open eruption, so closed eruption was considered the correct approach.
All aspects of the case were considered in detail during the treatment-planning interview. A combined surgical-orthodontic approach was chosen because it allowed for extracting a few teeth at a time and hastening the eruption of the permanent teeth. Alternative treatment plans would be considered in case of failure of the planned treatment because of the potential ankylosis of some permanent impacted teeth.
Treatment progress
Maxillary and mandibular fixed appliances on the deciduous molars and the permanent erupted teeth were used with the straight-wire technique. Inter-maxillary Class II elastic mechanics were used, with0.016-in nickel-titanium archwires and sequential 0.017×0.022-in stainless steel archwires. The patient was referred to the oral surgeon for exposure of the impacted teeth after rigid archwires were placed in both arches. Surgery was first carried out in the mandible, and the mandibular first premolars were exposed. A button was bonded intraoperatively to each exposed crown as coronally as possible. Custom wire chains were prepared with 0.012-in ligature wire and fixed to the bonded button. The flaps were then sutured back to their original positions. The chains passed under the flaps and emerged at the center of the crest in the mandibular arch ( Figs 5–7 ).




