Introduction
The aim of this longitudinal study was to investigate mandibular rotation and angular remodeling in mouth-breathing children compared with nasal-breathing children.
Methods
The sample included 55 severely obstructed mouth-breathing children (mean age, 6.1 years) and 55 nasal-breathing children (mean age, 7.3 years). The cephalograms at baseline and after 1 year were traced and measured, and superimpositions were made to determine true mandibular rotation, apparent rotation, and angular remodeling. The significance level was set at 5%.
Results
The mouth-breathing children had a longer face cephalometric pattern compared with nasal-breathing children. No cranial deflection differences were observed. No changes in the vertical growth pattern were observed during the 1-year period in either group. There were no statistically significant differences between the groups regarding apparent rotation (mouth breathing, −0.54°, vs nasal breathing, −0.41°). In comparison with the nasal breathers, the mouth breathers showed statistically significant lower yearly rates of counterclockwise true rotation (mouth breathing, −0.60°, vs nasal breathing, −1.31°) and angular remodeling (mouth breathing, 0.06°, vs nasal breathing, 0.87°).
Conclusions
Mouth-breathing children had a hyperdivergent cephalometric pattern, but against all expectations, counterclockwise true mandibular and apparent rotations were the average observations. Mouth-breathing children showed less true rotation and angular remodeling than did nasal breathers; however, apparent rotations were similar.
Previous studies reported that the mandible typically rotates in a forward direction during childhood and adolescence. However, on occasion, the mandible exhibits a simple pattern of rotation. In most cases, the rotational phenomenon appears to be complex with variations in the direction and intensity.
Persons with a backward rotation of the mandible and an increased lower anterior facial height are of concern to orthodontists because of esthetic, functional, and biomechanical reasons. Excessive vertical dentofacial growth is associated with hereditary factors, but environmental factors, such as mouth breathing, can play an important role in the growth direction. The association between mouth breathing and a long facial form can be attributed to the backward rotation of the mandible in nasally impaired children. This backward rotation most likely occurs because of greater vertical growth in the molar region than at the condyles; this happens when the mouth is maintained in an open position. Moreover, the effect of airway is gaining in importance, particularly with the increasing role of orthodontics in obstructive sleep apnea.
Mandibular rotation includes 3 components: true rotation, apparent rotation, and angular remodeling. However, in daily practice and scientific investigations, orthodontists analyze mandibular rotation primarily by considering apparent rotation. Previous reports have nonetheless shown that the mandible undergoes only limited amounts of apparent rotation because larger amounts of true rotation are typically camouflaged by angular remodeling. Therefore, understanding true mandibular rotation and angular remodeling could add important information to better understand facial growth changes. Because mouth-breathing subjects have a peculiar pattern of growth adaptation, a study designed to determine the 3 components of mandibular rotation of these patients is needed.
The aim of this investigation was to determine the 3 components of mandibular rotation in mouth-breathing children to determine whether the expectation that the mandible rotates in a clockwise direction is accurate. It was also our purpose to evaluate the cephalometric vertical patterns of mouth and nasal breathers at baseline and 1 year later.
Material and methods
The study protocol was approved by the ethics committee of Federal University of Minas Gerais, Belo Horizonte, Minas Gerais, Brazil (ETIC 488/06). Informed written consent was obtained from the parents before the subjects entered the study.
The sample size of each group was calculated based on an alpha significance level of 0.05 and a beta of 0.2 to achieve power of 80% to detect a mean difference of 0.5° between the groups, with an estimated standard deviation of 1.05°, according to the study of Wang et al. The sample size calculation showed that 55 patients in each group were needed. Therefore, the sample included 110 prepubertal children (55 nasal breathers, 55 mouth breathers) from 3 to 10 years of age. No subject had previous orthodontic or orthopedic treatment, cleft of the lip or palate, or a persistent sucking habit at the beginning of the study.
The nasal breathers were selected from a growth study sample at the Pontifical Catholic University of Minas Gerais (ethics committee CAAE 2001/02) and had a normo-occlusion Class I dental pattern. Their parents were questioned about the children’s medical history to exclude any subject with chronic mouth breathing, permanent snoring, and tonsillectomy or adenoidectomy. Nasal breathers with obvious hyperplasia of the tonsils and adenoids on the cephalometric film were excluded from further analysis.
The mouth breathers were consecutively referred by pediatricians or primary care physicians to the Outpatient Clinic for Mouth-Breathers at the Federal University of Minas Gerais, Belo Horizonte, Minas Gerais, Brazil, with the chief complaint of mouth breathing. They were systematically evaluated in 1 visit by a multidisciplinary team comprising otorhinolaryngologists, allergists, and orthodontists. Based on the clinical and endoscopic otorhinolaryngology examinations performed by 2 authors (L.P.F., H.M.G.B.) in the first consultation, mouth breathing was confirmed, and the nasopharyngeal obstruction by adenoidal tissues was classified into 3 categories: mild (<50%), moderate (50%-75%), and severe (>75%). Palatine tonsil hypertrophy was classified according to the criteria of Brodsky and Koch. Only children with severe obstructions (nasopharynx obstruction >75%, or Brodsky and Koch’s grades 3 or 4) with an indication for adenoidectomy or tonsillectomy were included in this investigation. All children were on the waiting list for authorization from the municipal health service, which at the time of the sample collection (2006-2010) generally took more than 1 year for the otorhinolaryngology surgical approval because of high demand and low absorptive capacity. During this waiting period, no children had any medical management (surgical or nonsurgical) that might have altered the soft-tissue inflammation of the airways.
The patients in each group were matched by the stage of skeletal maturation, which was evaluated basing on the lateral cephalometric radiograph morphologic aspect of cervical vertebrae C2, C3, and C4. All subjects were in cervical vertebrae stage 1 (prepubertal) at baseline. All children in both groups had the same ethnicity and lived in the same metropolitan area at the time of the sampling process.
Lateral cephalometric radiographs of all children were obtained at baseline (T0) and 1 year later (T1), at a mean of 12 months apart (±2 months). For every child, both radiographs were taken with the same equipment. The cephalograms had to be of sufficient quality to ensure that all structures necessary for landmark identification and regional superimposition could be identified. The cephalometric landmarks ( Fig 1 ) were identified on all radiographs and hand-traced on acetate paper with a 0.5-mm lead pencil on a standard light box by 1 investigator (B.Q.S.). The radiographs were scanned and imported into commercially available software systems (Dolphin Imaging & Management Solutions, Chatsworth, Calif; and AutoCAD, version 10.0; Autodesk, San Rafael, Calif).
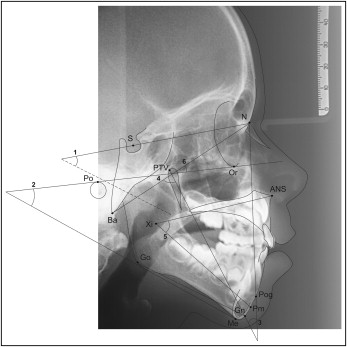
The vertical cephalometric analysis, comprising 6 angular measurements ( Fig 1 ), was digitally performed with the Dolphin software. Superimposing the tracings of the baseline and 1-year later cephalograms allowed classification of the mandibular rotation as true rotation, apparent rotation, and angular remodeling ( Fig 2 ). The measurements of the 2 rotational angles were made with the AutoCAD software.
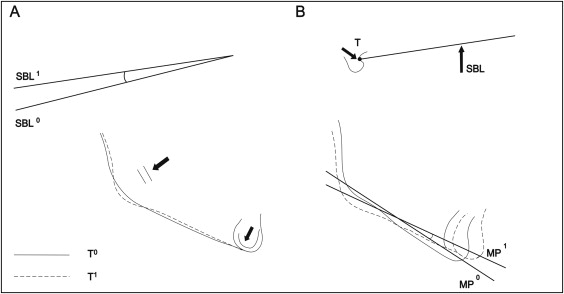
The assessment of mandibular rotation was based on a previously described reference system traced on stable craniofacial structures. For the cranial base, the tracings were superimposed on the stable basicranial line. It was traced through the most superior point of the anterior wall of the sella turcica at the junction with tuberculum sellae (point T) drawn tangent to the lamina cribrosa of the ethmoid bone. The mandible was superimposed on the internal cortical outline of the symphysis with the best fit on the alveolar canals.
True rotation was defined as the angular change between the stable basicranial lines at the first and second observations on the superimposed tracings using fiduciary mandible landmarks. Apparent rotation was measured after these superimpositions of the stable basicranial line at point T. The difference in the inclination of the mandibular plane (gonion-gnathion) measurements represented the apparent rotation ( Fig 2 ). Angular remodeling was defined as the difference between apparent rotation and true rotation.
Statistical analysis
To determine errors in landmark identifications and measurements, 25 subjects were randomly selected, and their cephalograms were retraced and remeasured by the same orthodontist (B.Q.S.) 1 month later. Fifty subjects were traced by another orthodontist (T.B.J.P.) to evaluate interexaminer reliability. Both intraclass correlation coefficients and Dahlberg’s equation were used to assess any landmark errors, and the means of the errors were calculated. Systematic error (bias) was assessed using the paired t test.
To assess the differences between mouth and nasal breathers in the age distribution at baseline, and the cephalometric vertical measurements at both times, an independent samples t test was used. To evaluate the cephalometric changes between baseline and 1 year later in each group, paired t tests were used. The chi-square test was used to compare the proportions of the sexes between mouth and nasal breathers.
To assess the 3 components of mandibular rotation, the breathing pattern was considered to be the independent variable, and true rotation, apparent rotation, and angular remodeling were the dependent variables. Multivariate analysis of variance (MANOVA) with the Hotelling T was used to compare the independent variables between the 2 groups. The Hotelling T is used when the independent variable forms 2 groups and represents the most significant linear combination of the dependent variables. The assumptions of normality in each group (Kolmogorov-Smirnov test), equality of covariance-variance matrices among groups (Box test), and multiple correlations between dependent variables (Bartlett test) were accomplished. The significance level was set at P <0.05.
Results
The systematic errors in the cephalometric measurements did not exceed 0.24° and were thus considered to be within an acceptable limit. Dahlberg’s error of the method yielded results between 0.02° and 0.16° for the angular cephalometric measurements at baseline and between 0.15° and 0.22° for the mandibular rotation measurements. Intraclass correlation coefficient values showed high agreement between the sets of measurements, varying between 0.98 (SNGoGn and FMA) and 0.82 (true rotation).
The mean ages at baseline were 6.1 years (SD, 1.90) in the mouth-breathing group and 7.3 years (SD, 1.82) in the nasal-breathing group. Although the age distribution of the subjects in the groups showed a significant difference at baseline, all children were in the same prepubertal stage of mandibular growth maturation during the observation period (CS 1). The nasal-breathing group had 19 boys and 36 girls, and the mouth-breathing group had 35 boys and 20 girls, a significant difference between the 2 groups for sex distribution.
Statistically significant differences in the cephalometric patterns of the mouth and nasal breathers at baseline and 1 year later are shown in Table I . Most cephalometric measurements of the mouth breathers represented a hyperdivergent growth pattern. The measurements of the nasal breathers were within normal limits. Table I also shows that in the 1-year observation period, the cephalometric patterns of both groups were maintained. No statistically significant differences were found in the intragroup paired comparison ( P >0.05). Cranial deflection (FH.N-Ba) was within normal limits for both groups, without significant statistical differences between them.
| Measurement | Normative value | MB (n = 55) | MB paired t test (T1 − T0) | NB (n = 55) | NB paired t test (T1 − T0) | Independent t test at T0 (MB vs NB) | Independent t test at T1 (MB vs NB) | ||
|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | P value | T0 | T1 | P value | P value | P value | ||
| SNGoGn (°) | 32.0 ± 3.0 | 38.1 ± 4.5 | 37.9 ± 4.8 | 0.555 | 33.9 ± 4.2 | 34.0 ± 4.6 | 0.780 | <0.001 | <0.001 |
| FMA (°) | 25.0 ± 5.0 | 30.3 ± 5.3 | 29.6 ± 5.0 | 0.168 | 26.2 ± 4.6 | 26.1 ± 5.0 | 0.895 | <0.001 | 0.001 |
| Facial taper (°) | 67.0 ± 4.0 | 62.7 ± 2.9 | 63.1 ± 3.1 | 0.111 | 66.1 ± 3.5 | 66.2 ± 3.4 | 0.699 | <0.001 | <0.001 |
| Facial axis (°) | 90.0 ± 4.0 | 84.6 ± 7.2 | 86.5 ± 3.9 | 0.076 | 89.9 ± 3.4 | 89.7 ± 3.5 | 0.580 | <0.001 | <0.001 |
| Lower face height (°) | 47.0 ± 4.0 | 47.5 ± 3.7 | 47.6 ± 3.8 | 0.836 | 43.7 ± 3.9 | 44.1 ± 3.9 | 0.168 | <0.001 | <0.001 |
| Cranial deflection (°) | 27.0 ± 3.0 | 31.1 ± 3.0 | 30.9 ± 2.6 | 0.498 | 29.8 ± 2.6 | 29.8 ± 2.5 | 0.784 | <0.05 | <0.05 |
The MANOVA test showed a significant difference between the children’s modes of breathing on the components of mandibular rotation: F 3,106 = 3.002, P <0.05; Hotelling T = 0.085; partial ɛ 2 = 0.078. Mean value vectors were significantly different between the 2 group in regard to mandibular angular remodeling (mouth breathers, 0.06°, vs nasal breathers, 0.87°) and true mandibular rotation (mouth breathers, −0.60°, vs nasal breathers, −1.31°) ( Table II ). However, the apparent mandibular rotation of the mouth breathers was similar to that of the nasal breathers (mouth breathers, −0.54°, vs nasal breathers, −0.41°). Forward (counterclockwise) mandibular displacement was the predominant growth behavior in the apparent and true rotations in both groups ( Table II ).



