Class II malocclusion can be managed in three different ways: extraction, nonextraction with distal movement of the maxillary teeth into Class I, and orthognathic surgery, which can be combined with extraction or nonextraction of teeth. Factors that might influence the treatment options include the severity of the Class II malocclusion and age of the patient. For the growing patient, nonextraction with growth modification may be the treatment of choice. Modification of growth is usually done by functional appliances, either removable or fixed.
TRADITIONAL FUNCTIONAL APPLIANCES
A variety of removable functional appliances have historically been used in the management of Class II malocclusion in the growing patient.
Headgear
Of all the functional appliances, headgear is the most common. Its use dates back to the nineteenth century. The headgear restricts maxillary growth as well as distal movement of the maxillary first molars to which the headgear forces are applied. Forces from the headgear can be efficiently controlled, which makes it a versatile appliance. Success with the headgear largely depends on patient cooperation. Although the preadolescent patient is usually very compliant, teenage patients are the least likely to use the headgear effectively because of peer pressure. Also, the headgear should be used cautiously because of the risk of possible impaction of the unerupted maxillary second molars.
Other Nonfixed Functional Appliances
Whereas the headgear can be used universally, other nonfixed functional appliances may not have this advantage. Certain criteria must be fulfilled for a patient to be treated with removable functional appliances. These criteria include low mandibular plane to Frankfort horizontal angle (FMA no greater than 30 degrees), upright mandibular incisors, and growth potential. Low FMA is most preferred because of the bite-opening effect of functional appliances during correction of Class II malocclusion. Functional appliances are usually contraindicated in high-angle patients because these appliances tend to open the bite. In addition, because they rest against the mandibular incisors, these appliances can result in their proclination and thus are contraindicated in proclined and procumbent incisors as well.
Fixed Functional Appliances
The fixed functional appliances can be classified into three groups: fixed rigid, fixed flexible, and fixed hybrid. The most used and historically prominent of the fixed rigid functional appliances is the Herbst.
Herbst appliance
The Herbst appliance (Dentauram, Ispringen, Germany) was first introduced in the early twentieth century and gained popularity in the 1980s after work by Pancherz. Considerable debate surrounds how correction of Class II malocclusion is achieved during use of the Herbst. Users of the appliance have argued in favor of growth modification. Research has shown that the Herbst, as with other functional appliances, does not “grow” mandibles but produces a “headgear effect” by distalizing the maxillary molars and restricting maxillary growth. There is no evidence to support enhanced mandibular growth from use of the Herbst. The results obtained from the Herbst may be no different from Class II elastics.
Interpretation of these studies requires caution. The basic tool used to assess changes in most studies is the lateral cephalogram, which has limited application in detecting condylar changes and is more suited to interpretation of large, gross changes. Computed tomography (CT) scans would be better suited for such assessment but are more expensive.
The Herbst appliance was initially developed for the growing patient. However, its applications to correct Class II malocclusion have been extended to adult patients. Other appliances in the same category as the Herbst include the mandibular anterior repositioning appliance (MARA) (AOA Orthodontic Appliances, Sturtevant, Wis.) and fixed twin block. Of the flexible fixed functional appliances, the most studied is the Jasper Jumper (American Orthodontics, Sheboygan, Wis.).
HYBRID FUNCTIONAL APPLIANCES
Recently, a new group of hybrid functional appliances have appeared in the orthodontic armamentarium. Unlike the rigid fixed functional appliances that lack flexibility, hybrid functional appliances contain the features of both rigid and flexible appliances. They are spring loaded, which allows greater flexibility of the mandible. Two such appliances include the Sabbagh Universal Spring (Dentaurum) and the Forsus Spring (3M Unitek, Monrovia, Calif.).
Sabbagh Universal Spring
Developed by Dr. Sabbagh in Germany, the Sabbagh Universal Spring (SUS) is a telescopic device similar to the Herbst externally but with a different mode of activation. The SUS consists of a telescopic rod fitted into a guide tube ( Fig. 10-1, A ). Inside the guide tube is a spring that can be adjusted to deliver different force levels, depending on the severity of the Class II malocclusion ( Fig. 10-1, B ). Its U -loop is designed to fit into the maxillary first molars while the lower end is tied to the archwire between the first premolar and the canine, or even between the canine and the lateral incisor.
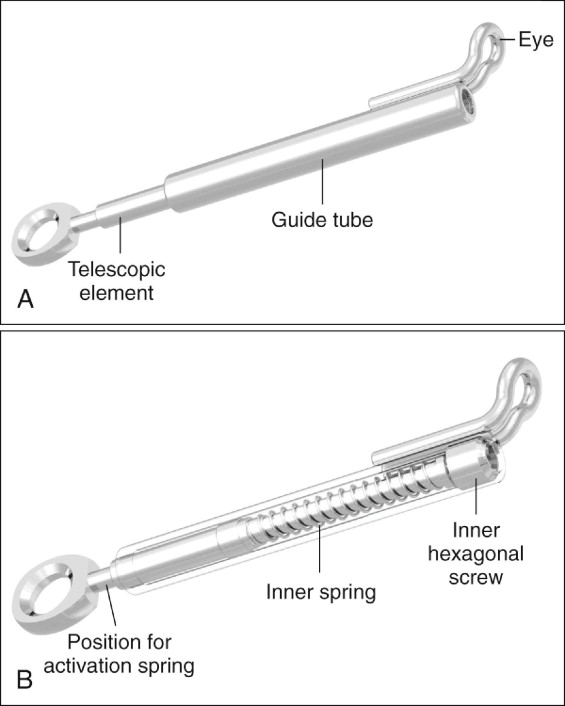
Unlike the Forsus, the SUS is a true universal spring in that it does not have a left or right side. External springs can be added on to the appliance to increase its springiness. Dentaurum supplies springs for such a purpose, but any spring that fits into the telescopic rod can be used.
Indications
The SUS can efficiently treat a variety of Class II malocclusions. Currently, limited information is available in the literature on the use of the SUS. Studies conducted at the University of Oklahoma have shown that the appliance can be used in both adult and young patients to correct Class II discrepancies. Treatment of the adult patient is based on the understanding that management of Class II malocclusion using the nonextraction protocol does not depend on restriction of maxillary growth or modification of mandibular growth; rather, it is mostly dentoalveolar.
The SUS can be used in patients with high or low FMA because the appliance intrudes the buccal segments in the maxillary arch. In patients whose second molars have erupted, it is recommended that the arch wire be extended to include the maxillary second molars. The SUS delivers an intrusive force to the maxillary first molars, and failure to incorporate the maxillary second molars into the archwire may result in severe second-order discrepancy between the first and second molars after the first molar is moved distally and intruded.
Figure 10-2 shows a patient with bilateral Class II malocclusion who was treated with an SUS. Initially, the second molars were not included in the archwires, as shown by the vertical discrepancy between the first and second molars. This could have been avoided if the second molars had been either bonded or banded and included in the initial archwires used for distal movement of the maxillary arch.
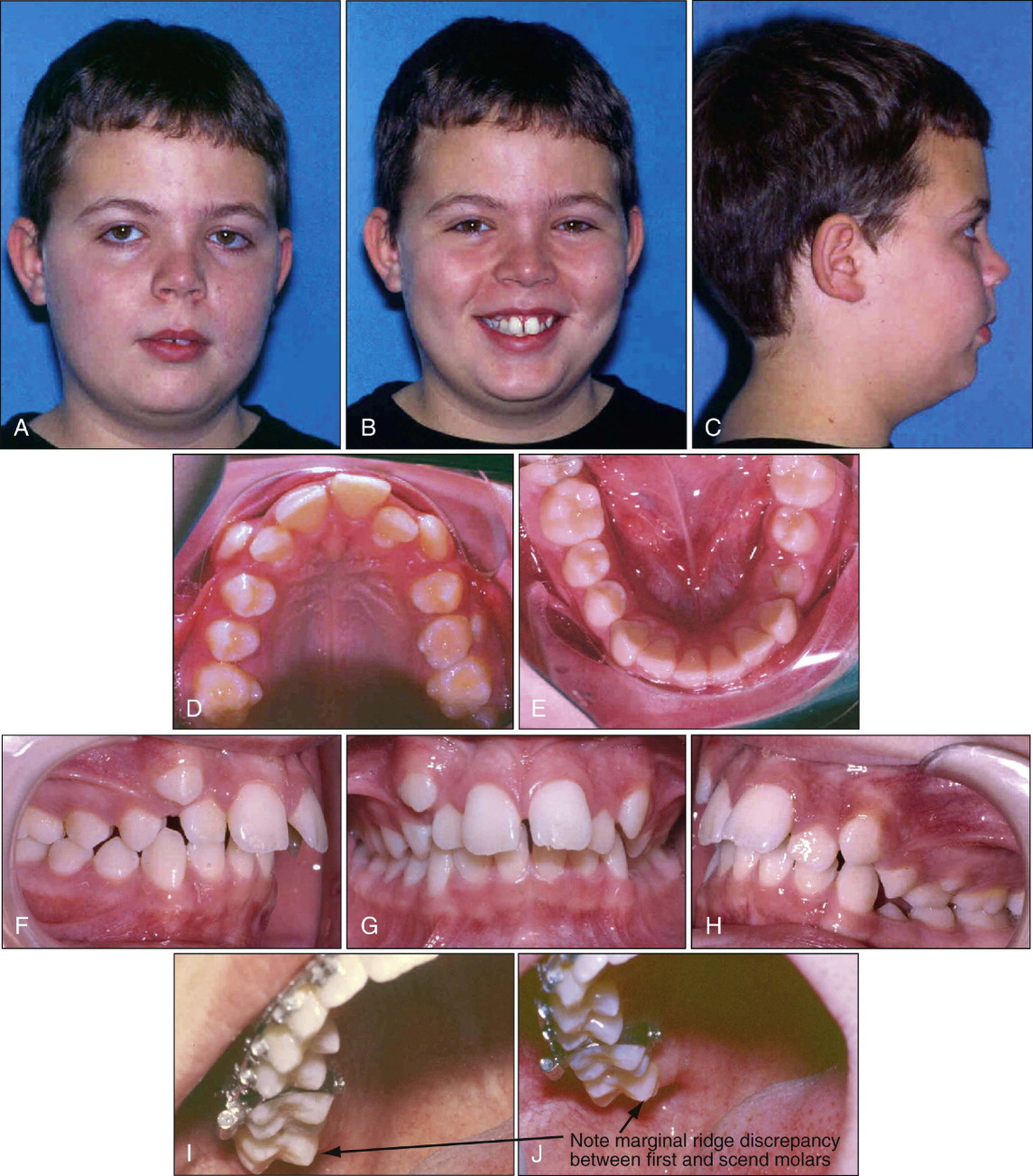

As in the maxillary arch, the mandibular second molars also need to be included in the mandibular archwires to increase the anchorage in that arch. Although it is not necessary to use a full-size wire in the maxillary arch, a rigid full-size wire is recommended in the mandibular arch to avoid proclination of the mandibular incisors. The author also recommends an omega loop mesial to the mandibular first or second molars to tie back the whole mandibular arch. If this is not done, the patient will likely develop spacing between the first premolars and the canines if the mesial part of the SUS is engaged between these two teeth.
A contraindication of functional appliances is proclination of the mandibular incisors, which may occur during use of the appliance. After the appliance is removed and during the recovery period, the mandibular incisors return to their previous position before delivery of the SUS. The same is true for the Forsus appliance.
Table 10-1 summarizes cephalometric measurements of patients treated with the SUS. The average time needed to correct the Class II malocclusion is 3 to 4 months. Depending on space available in the maxillary arch, no more than 6 months is required after Class II correction to detail and finish the treatment. Thus on average, a full-step Class II malocclusion is treated in 15 months.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


