Patients with multiple craniofacial fractures often suffer from stomatognathic problems after their primary treatment, because administering emergency care is the clinician’s highest priority. Therefore, optimal bone repositioning is sometimes difficult because bone fixation is delayed. Moreover, neither an adequate radiographic examination nor an evaluation of primary occlusion is available during the repair of fractured bones. The lack of these assessments can also lead to occlusal dysfunction after bone fixation. As a result, patients with craniofacial fractures often require occlusal reconstruction. This report describes the successful occlusal reconstruction with orthodontic-surgical treatment of a patient with multiple maxillofacial bone fractures. Combined surgery, including an intraoral vertical ramus osteotomy and a mandibular body osteotomy, was performed to reposition the deviated mandible after 3 months of preoperative orthodontic treatment. The total active treatment period was 25 months. After treatment, both the facial asymmetry and the anterior open bite caused by the skeletal disharmony were significantly improved. Additionally, the range of condylar motion, maximum occlusal force, and occlusal contact area during maximum clenching were also increased. These stomatognathic functions were further enhanced by 2 years of retention. Orthodontic-surgical reconstruction appears to improve both facial esthetics and occlusal function in patients with facial asymmetry caused by severe traumatic maxillofacial fractures.
The treatment of multiple craniomaxillofacial fractures caused by a traumatic injury is sometimes challenging, since the results of bone fixation affect both facial esthetics and occlusal function, which directly affect the patient’s quality of life. On the other hand, patients who have suffered craniomaxillofacial trauma frequently have both neurologic and orthopedic injuries, which can be life-threatening conditions.
For these patients, providing emergency care is the most immediate priority, so optimal bone repositioning is often difficult because bone fixation is delayed. Additionally, neither an adequate radiographic examination nor an evaluation of the primary occlusion is available when the fractured bones are being repaired. These situations can lead to poor preoperative imaging of and inadequate preoperative treatment planning for maxillofacial injuries. As a result, patients with craniofacial fractures often have a malocclusion after their primary treatment.
Consequently, most patients with craniofacial fractures require occlusal reconstruction including secondary surgery and orthodontic or prosthetic treatment. These patients frequently suffer both morphologic and stomatognathic problems. To treat these dysfunctions, occlusal rehabilitation is occasionally necessary. However, there have been few reports regarding the clinical assessment of the changes in occlusal function produced by the secondary treatment of maxillofacial fractures.
We report here the successful orthodontic-surgical treatment of a patient with multiple maxillofacial bone fractures who subsequently required occlusal reconstruction. Combined surgery, involving an intraoral vertical ramus osteotomy and a mandibular body osteotomy, was performed to reposition the mandibular body. In addition, the patient’s stomatognathic function, condylar motion, and jaw movement were assessed to evaluate the gnathologic improvement after treatment.
Diagnosis and etiology
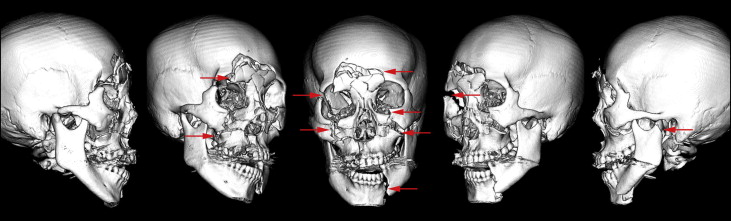
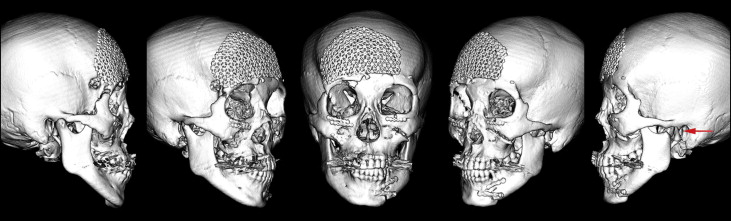
A Japanese woman, aged 29 years 10 months, came to the outpatient clinic of Okayama University Hospital in Japan. She had been involved in a traffic accident 2 months before and had suffered multiple maxillofacial bone fractures in her basal skull, nasal bone, zygoma, maxilla, mandibular body, and condyle ( Fig 1 ). After the cerebral surgery, duraplasty for cerebrospinal fluid rhinorrhea was performed, and the fractured bones were repositioned and fixed in place with titanium plates by a plastic surgeon ( Fig 2 ). However, the fractured condyle on the left side could not be surgically repaired and displayed abnormal adhesion ( Fig 2 ).
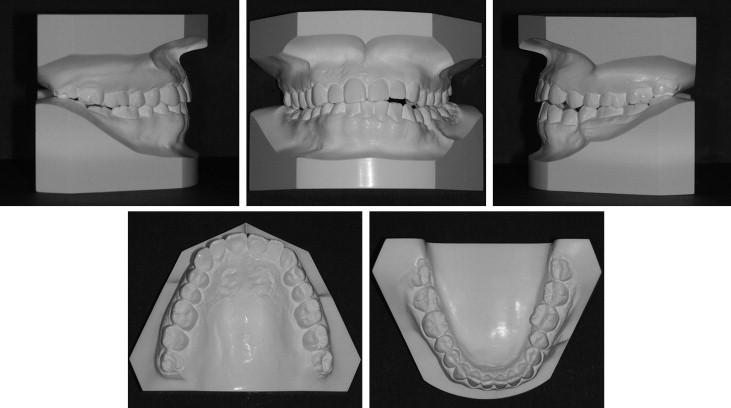
Her chief complaints were masticatory dysfunction, a unilateral open bite, and facial asymmetry ( Figs 3-5 ). She had a straight profile, but her mandible deviated to the left ( Fig 3 ). A lateral open bite was observed in the left anterior segment, and the mandibular border was discontinuously fixed at the fracture line ( Figs 3 and 4 ). The anteroposterior molar relationships were Class III on the right side and Class I on the left side. The maxillary dental midline almost coincided with the facial midline, but the mandibular dental midline was shifted 2.0 mm to the left ( Figs 3, 4, and 5 , B ). Minor crowding was observed in both arches ( Figs 3 and 4 ). No fractured teeth were observed on the panoramic radiography ( Fig 5 , C ).

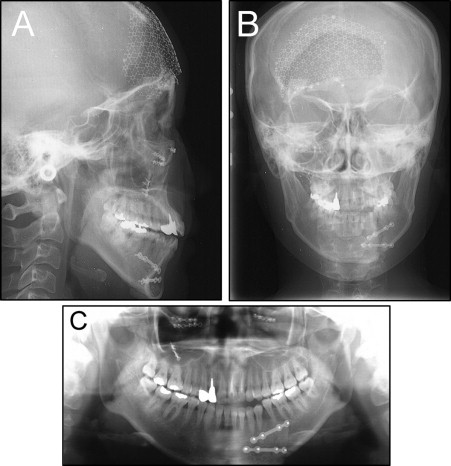
The cephalometric analyses, when compared with Japanese norms, showed a skeletal Class I jaw relationship (ANB, 2.8°), a steep mandibular plane angle (Mp-SN, 42.0°), and excessive anterior facial height (N-Me, 134.0 mm) ( Table I ). The mandibular incisors were lingually inclined relative to the mandibular plane (L1-Mp, 81.0°).
| Variable | Japanese norm (adult female) | SD | Pretreatment | Posttreatment | 2-year retention |
|---|---|---|---|---|---|
| Angular (°) | |||||
| ANB | 2.8 | 2.44 | 2.5 | 3.0 | 3.0 |
| SNA | 80.8 | 3.61 | 86.0 | 86.0 | 86.0 |
| SNB | 77.9 | 4.54 | 83.5 | 83.0 | 83.0 |
| Mp-SN | 37.1 | 4.64 | 42.0 | 44.5 | 44.5 |
| U1-FH | 112.3 | 8.26 | 112.0 | 114.0 | 113.5 |
| U1-SN | 105.9 | 8.79 | 110.5 | 111.5 | 110.5 |
| L1-Mp | 93.4 | 6.77 | 81.0 | 80.5 | 80.0 |
| Interincisal angle | 123.6 | 10.64 | 126.0 | 126.0 | 126.5 |
| Occlusal plane | 16.9 | 4.40 | 19.0 | 17.5 | 17.5 |
| Linear (mm) | |||||
| S-N | 67.9 | 3.65 | 67.0 | 67.0 | 67.0 |
| N-Me | 125.8 | 5.04 | 134.0 | 131.0 | 131.0 |
| Me/NF | 68.6 | 3.71 | 75.0 | 72.0 | 72.0 |
| Go-Me | 71.4 | 4.14 | 71.5 | 63.0 | 63.0 |
| Ar-Me | 106.6 | 5.74 | 111.0 | 108.5 | 108.5 |
| Ar-Go | 47.3 | 3.33 | 46.0 | 49.5 | 49.5 |
| Overjet | 3.1 | 1.07 | 4.5 | 2.5 | 2.3 |
| Overbite | 3.3 | 1.89 | −1.5 | 2.7 | 2.9 |
| U1/PP | 31.0 | 2.34 | 30.0 | 30.0 | 30.5 |
| U6/PP | 24.6 | 2.00 | 22.5 | 22.5 | 22.5 |
| L1/Mp | 44.2 | 2.68 | 48.0 | 50.0 | 50.0 |
| L6/Mp | 32.9 | 2.50 | 32.0 | 32.0 | 32.0 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


