The face is essential for the expression of emotion and physical state. Scars on the face, in particular, are a stigma in human society and can isolate a person from social contacts. Facial wounds are commonly the result of road traffic accidents, windshield injuries, assaults, animal and human bites, and war injuries. Facial wounds should be aggressively treated to avoid the consequence of an unsightly scar. The presence of separate esthetic units and combined injuries to bone, skin, and vital structures require special attention in the assessment and treatment of facial wounds and subsequent scars.
Although facial scar management is an elective procedure, the appropriate management of acute facial wounds dramatically affects the quality and quantity of scar tissue formation, thus affecting the need for and results of secondary scar revision procedures. It is therefore essential to understand and make use of the principles of wound healing.
Principles of Wound Healing
Acute Inflammation
As soon as tissue is damaged, the wound is filled by a coagulum. Nerve impulses are generated at the injured site, and the substances released by the damaged cells cause local hyperemia and increased permeability of the vessel wall. This acute inflammatory reaction is the initial step and cornerstone of the healing process. Platelet degranulation and activation of the complement and clotting cascade form a fibrin clot for hemostasis. Chemotactic agents including epidermal growth factor (EGF), insulin-like growth factor 1 (IGF-1), platelet-derived growth factor (PDGF) and transforming growth factor-β (TGF-β) are released during platelet degranulation. Recruitment of neutrophils, macrophages, epithelial cells, mast cells, endothelial cells, and fibroblasts follows. Inflammatory cells proliferate and differentiate for phagocytosis, with further release of cytokines, and form granulating tissue.
The second phase, known as the proliferative phase, spans days 5 to 14 after injury. Capillaries and fibroblasts invade the coagulum in the wound. This new tissue is known as granulation tissue. Blood supply to the area remains high, but permeability of the vessel walls is restored to normal and edema resolves. However, prolongation of the inflammatory process as a result of infection, presence of foreign bodies, and delay in treatment increases the activity of fibrogenic cytokines such as TGF-β and IGF-1, thereby increasing the chance of hypertrophic scar development.
During the maturation phase of wound healing, the collagen scaffold is being remodeled, resulting in increased tensile strength. This process continues for about 1 year under normal conditions.
Scar Formation
In a scar, type I collagen is laid down by fibroblasts. Its appearance ranges from an inconspicuous line to keloid that overgrows the original wound. This process begins on day 4 of wound healing, when the fibroblasts start synthesizing extracellular collagen. The activity of the fibroblasts is increased by fibroblast activation factor, which is liberated by macrophages. Capillaries develop from the vascular endothelium and form a dense vascular network within the newly formed connective tissue. Myofibroblasts differentiate into fibroblasts and produce type I collagen, giving the scar stability. Capillaries are then obliterated, and the original multitude of cells is reduced to a few cell types.
Various factors cause persisting stimulation of the wound, resulting in enhanced cicatrization. Therefore, care is needed to remove all foreign bodies and prevent infection. Adequate débridement should remove all necrotic tissue, and further trauma should be avoided by use of an atraumatic suturing technique.
Factors Affecting Wound Healing
General Factors
The process of healing is more rapid in young patients. Patients with protein, vitamin, or trace element deficiency heal more slowly. Chronic illnesses such as anemia, uremia, uncontrolled diabetes, or immunosuppressive states decrease wound-healing capacity. The long-term use of steroids or immunosuppressive agents for treatment of other medical illnesses could change the inflammatory phase of the wound and lead to delayed formation of new tissue.
Local Factors
Blood Supply
A healing wound needs energy and building materials such as oxygen, glucose, amino acids, vitamins, and trace elements. The blood supply to the wound affects the availability of oxygen to the tissue. Blood supply is decreased in the state of shock and in patients with arteriosclerosis or diabetes. Hematoma underneath the wound raises the skin flap, resulting in an impaired blood supply to the tip of the flap via the reticular dermal plexus and causing necrosis of the wound edge and secondary infection. Although the face is rich in blood supply, necrosis of wound edges leads to undesirable scars.
Necrotic Tissue
The facial skin has a rich blood supply, and débridement should be minimal, because most of the tissue will survive and heal.
However, necrotic tissue at the wound edges, caused by direct trauma to the skin, can harbor bacteria. It should be trimmed off before suturing, because devitalized tissue provides an anaerobic medium for the multiplication of anaerobic microbes as well as other microorganisms.
Foreign Bodies
Depending on the mechanism of injury, foreign bodies are common in certain trauma scenarios. Organic foreign bodies (e.g., wooden splinters, soil) and inorganic foreign bodies (e.g., glass or metal shards) should be removed thoroughly during the acute treatment of wounds. These materials not only provide a nidus for bacteria but prolong the inflammatory response of the wound, causing scarring, recurrent infection, and traumatic tattooing.
Previous Irradiation
The patient’s head and neck area may have been irradiated for the treatment of cancer or other clinical conditions. The radiation effect to the skin is permanent if the radiation exceeded 15 to 20 Gy over a relatively short period. Radiation-induced atrophy is usually noticed weeks to months after the initial exposure, although further atrophic changes may evolve over 1 or 2 years. The skin is thinned, dry, and hyperkeratotic. Telangiectasia and hyperpigmentation or hypopigmentation are usually prominent features. In the upper dermis, capillaries are reduced in number, and the capillaries, venules, and lymphatics are often widely dilated. Wound healing of irradiated skin is usually slower than that of normal skin, and complications such as infection and dehiscence are more common. Irradiated skin wounds are usually inelastic, and the edges are difficult to approximate in the usual manner.
Infection
Infection of the wound causes an inflammatory reaction and edema. There is an increased number of inflammatory cells, as well as fibrinolysis and breaking down of collagen; hence, the tensile strength of the wound is affected.
Common bacteria causing skin infection are commensals such as Staphylococcus and Streptococcus species. Wounds that communicate with the nasal or oral cavities may be contaminated with anaerobes. Antibiotics usually are not necessary if there is adequate débridement and cleaning of the wound. Booster tetanus immunization is mandatory in appropriate cases.
Factors Affecting Wound Healing
General Factors
The process of healing is more rapid in young patients. Patients with protein, vitamin, or trace element deficiency heal more slowly. Chronic illnesses such as anemia, uremia, uncontrolled diabetes, or immunosuppressive states decrease wound-healing capacity. The long-term use of steroids or immunosuppressive agents for treatment of other medical illnesses could change the inflammatory phase of the wound and lead to delayed formation of new tissue.
Local Factors
Blood Supply
A healing wound needs energy and building materials such as oxygen, glucose, amino acids, vitamins, and trace elements. The blood supply to the wound affects the availability of oxygen to the tissue. Blood supply is decreased in the state of shock and in patients with arteriosclerosis or diabetes. Hematoma underneath the wound raises the skin flap, resulting in an impaired blood supply to the tip of the flap via the reticular dermal plexus and causing necrosis of the wound edge and secondary infection. Although the face is rich in blood supply, necrosis of wound edges leads to undesirable scars.
Necrotic Tissue
The facial skin has a rich blood supply, and débridement should be minimal, because most of the tissue will survive and heal.
However, necrotic tissue at the wound edges, caused by direct trauma to the skin, can harbor bacteria. It should be trimmed off before suturing, because devitalized tissue provides an anaerobic medium for the multiplication of anaerobic microbes as well as other microorganisms.
Foreign Bodies
Depending on the mechanism of injury, foreign bodies are common in certain trauma scenarios. Organic foreign bodies (e.g., wooden splinters, soil) and inorganic foreign bodies (e.g., glass or metal shards) should be removed thoroughly during the acute treatment of wounds. These materials not only provide a nidus for bacteria but prolong the inflammatory response of the wound, causing scarring, recurrent infection, and traumatic tattooing.
Previous Irradiation
The patient’s head and neck area may have been irradiated for the treatment of cancer or other clinical conditions. The radiation effect to the skin is permanent if the radiation exceeded 15 to 20 Gy over a relatively short period. Radiation-induced atrophy is usually noticed weeks to months after the initial exposure, although further atrophic changes may evolve over 1 or 2 years. The skin is thinned, dry, and hyperkeratotic. Telangiectasia and hyperpigmentation or hypopigmentation are usually prominent features. In the upper dermis, capillaries are reduced in number, and the capillaries, venules, and lymphatics are often widely dilated. Wound healing of irradiated skin is usually slower than that of normal skin, and complications such as infection and dehiscence are more common. Irradiated skin wounds are usually inelastic, and the edges are difficult to approximate in the usual manner.
Infection
Infection of the wound causes an inflammatory reaction and edema. There is an increased number of inflammatory cells, as well as fibrinolysis and breaking down of collagen; hence, the tensile strength of the wound is affected.
Common bacteria causing skin infection are commensals such as Staphylococcus and Streptococcus species. Wounds that communicate with the nasal or oral cavities may be contaminated with anaerobes. Antibiotics usually are not necessary if there is adequate débridement and cleaning of the wound. Booster tetanus immunization is mandatory in appropriate cases.
Types of Wound
The nature of the wound is the most important determining factor for the final result of wound healing. The orientation of the wound in relation to the resting skin tension lines (RSTLs), its location and pattern, the degree of tissue trauma, presence of foreign bodies, degree of contamination, and individual tissue response determine the final scar appearance.
Every wound that involves the dermal papilla produces a scar. The most important prognostic factor for the final appearance of the scar is how the wound was inflicted rather than how it was sutured. Surgical technique is important in alleviating the damage caused by the injury but cannot totally reverse it.
Lacerated Wound
Laceration causes minimal tissue loss. Contamination is usually limited. However, the deep structures such as nerves and underlying organs should be examined for any injury.
Crush Wound
Crush injury is caused by blunt trauma. The wound edges are often irregular, and tissue is lost ( Fig. 23-1 ). All obviously devitalized tissue should be débrided. Traumatized tissue may be left behind, because the blood supply of the facial skin is rich and the chance of recovery is high. Unjustified débridement of facial skin leads to disfigurement, deformity, loss of function, and creation of a bigger scar.

Contaminated Wound
Contaminated wounds must be cleansed thoroughly. Deep-seated debris encourages inflammation, allergic reactions, and infection, whereas debris embedded within the superficial dermis becomes an unsightly “traumatic tattoo” if left unattended. Thorough scrubbing with a brush while the patient is under general anesthesia is necessary in the acute stage of wound treatment. This can avoid further treatment after the wound has healed.
Potentially Contaminated Wound
Wounds that communicate with the nasal or oral mucosa are potentially contaminated by the presence of normal flora, secretions, and anaerobes. They should be closed as soon as possible (i.e., within 6 hours), and patients should be prescribed antibiotics for gram-positive cocci and anaerobic bacteria.
Penetrating Wound
Care should be taken in treating penetrating wounds and deep lacerations, because important structures can be damaged. A thorough examination should be carried out and a plan for wound exploration prepared if necessary.
Management of Acute Wounds
Timing
Treatment should be undertaken as early as possible and preferably with the patient under general anesthesia to reduce discomfort and speed up healing. Delay in wound closure increases the risk of infection. For wounds with a low risk of infection, the “golden period” is within 12 to 24 hours after injury. With contaminated wounds or immunocompromised patients, primary closure should be achieved within 6 hours. If the wound carries a high risk of infection, delayed primary closure should be used. However, poor cosmetic outcome, prolonged patient discomfort, and inconvenience are negative factors of this approach and should be thoroughly discussed with the patient.
Débridement with Scrubbing
Particles of dark color (e.g., dirt, sand, gunpowder) will result in a traumatic tattoo if they remain in the wound. Such discoloration tends to be permanent. This can be easily dealt with by débridement or scrubbing in the acute stage, and these preventive measures cannot be overemphasized ( Figs. 23-2 and 23-3 ).


Thorough Irrigation to Remove Foreign Bodies
It has been said, “The solution to pollution is dilution.” Normal saline irrigation remains the best, most economical, and most readily available solution to the problem of contamination. Other antiseptics such as povidone-iodine or hydrogen peroxide are sometimes used; however, these agents can induce tissue reaction, inflammation, and possibly toxicity and should be avoided.
Pressurized irrigation is used in contaminated wounds to remove soil or small foreign bodies. The optimal pressure for irrigation remains debatable, but too high a pressure increases tissue trauma. The recommended pressure of 5 to 8 lb per square inch can be achieved by use of a 16- or 19-gauge needle.
Trimming of Necrotic Tissue
The potential for skin recovery in blunt facial trauma is great because the blood supply of the face is abundant. Trimming should therefore be limited to obviously dead tissue. The trimming of other tissue such as muscle and nerve should be minimal because it leads to depressed scars and loss of function.
Functional and Anatomical Repair in Layers
Facial appearance and expression depend on the integrity and function of the underlying musculature. Failure of functional and anatomical repair leads to depressed scars, tethering of the overlying skin, or facial asymmetry.
Damage to Facial Structures
Deep laceration is likely to damage underlying or adjacent organs or structures. Early identification and surgical repair are necessary to avoid unnecessary complications.
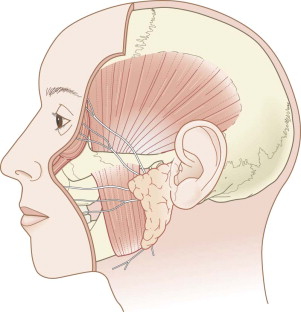
The facial nerve emerges from the skull base via the stylomastoid foramen. It emerges into the parotid gland from the posteromedial surface and divides into two main trunks, the temporozygomatic and cervicofacial branches. They are further divided into five branches: temporal, zygomatic, buccal, marginal mandibular, and cervical. They remain under the superficial musculo-aponeurotic system (SMAS) until the line shown in Figure 23-4 . The function of the facial nerve should be tested if the clinical situation allows. Wounds superficial to the SMAS behind the line are unlikely to have injured the facial nerve and need not be explored.
Parotid duct injury should be suspected if the wound is situated at the anterior border of the parotid gland or if there is salivary leak. The duct should be repaired with absorbable sutures. Untreated parotid injury leads to fistula formation.
The nasolacrimal duct connects the lacrimal sac at the medial canthus, slopes downward and laterally, and drains to an opening in the inferior meatus. Its injury should be suspected if there is a wound or previous suturing at or below the medial canthus. Cannulation of the duct with a fine probe is necessary before the wound is explored or sutured at that area.
Appropriate Use of Antibiotics and Suturing Materials
Routine systemic antibiotics are not necessary. The use of antibiotics should be tailored based on host defense status, degree of contamination, mechanism of injury, and likelihood of wound infection. Débridement is the most important step in cleaning up the wound, and antibiotics should not be a substitute.
Prophylactic antibiotics are necessary if the wound is expected to be contaminated, such as animal bites or wounds that communicate with the oral cavity. In medical conditions such as rheumatic heart disease or when host resistance is compromised, as in patients with uncontrolled diabetes and those taking steroids or immunosuppressive agents, antibiotics should also be commenced systemically and early. Commonly encountered organisms are streptococci, staphylococci, and gram-positive bacteria. Penicillin and cloxacillin are the drugs of choice. Patients who are sensitive to the penicillin group should be given erythromycin.
Topical antibiotics (e.g., chloramphenicol ointment) are definitely beneficial. (Very rarely, significant side effects of chloramphenicol have been reported, even when used topically, and in some hospitals its use is prohibited.) Elimination of local infection can reduce the chance of keloid and hypertrophic scar formation.
It is best not to leave any foreign bodies, even stitches, in the wound. If stitches are required at the subcuticular level, the first choice is plain catgut. Synthetic absorbable sutures such as Vicryl are now commonly used to avoid the potential problem of Creutzfeldt-Jakob disease. Stitches that are dissolved by hydrolysis rather than by inflammation have a lower chance of causing keloid and hypertrophic scars. The best result comes from using nonabsorbable monofilament stitches that are removed on day 3 to 7.
Tetanus passive immunization should be given if necessary. A booster dose should be given if the patient’s previous immunization was more than 10 years ago. Active immunization should be given if the wound is heavily contaminated.
Assessment of Existing Scar
Types of Scar
Good Scar
A desirable scar should be inconspicuous with the face at rest as well as in the dynamic situation. It should be flat, the same color as the surrounding skin, soft, narrow, and oriented in the same direction as the RSTL.
Bad Scar
A bad scar causes disfigurement and catches the observer’s eye. It is usually raised or depressed, hyperpigmented or hypopigmented, wide, and crossing the RSTL. However, the disfigurement may also be exaggerated in the patient’s mind. This largely depends on the patient’s gender, cultural background, profession, and attitudes. Therefore, before deciding the best method of revision of a scar deformity, it is important to communicate clearly with the patient and forestall any disappointment. It should be emphasized to the patient that a scar can only be improved or reduced and not completely erased.
Depressed Scar
A depressed scar commonly occurs running perpendicular to the RTSL as a result of wound closure under tension ( Fig. 23-5 ). Hematoma formation, wound infection, and inverted wound closure are the common causes of a depressed scar. It may also result from initially deep injury with loss of subcutaneous tissue and contracted fibrous tissue adhering to underlying fascia and muscle. Meticulous layered closure of the wound is important to prevent depressed scars. Tissue augmentation or dermabrasion or laser resurfacing can achieve recontouring of smaller depressed scars.

Z -plasty or W -plasty is used to correct the underlying tension problem, excising and elevating the scar in the same operation. Depression due to adherence of scar tissue to underlying structures requires excision of the scar, undermining of the subcutaneous tissue, and closure in layers to avoid recurrence.
Curved Scar
Healing of a curved scar produces contraction along the scar, resulting in a purse-string effect ( Fig. 23-6 ). This produces a “trapdoor” appearance of the scar. Small trapdoor scars can be excised and primarily closed, but larger trapdoor scars are best revised with Z -plasty or multiple W -plasties to realign the scar to the RSTL. Wider undermining peripheral to the trapdoor flap may also help to oppose the trapdoor deformity. The possible mechanism of this effect is the outward pulling force that acts on the scar after the revision.

Pigmented Scar
Hyperpigmentation is not a common problem in whites but occurs more frequently in Asians and dark-skinned people. During the scar maturation process, exposure to sunshine and smoking are the risk factors associated with hyperpigmentation. Topical tretinoin is useful in the treatment of hyperpigmentation, but avoidance of sunshine until the scar matures is the best way to combat this condition. Laser treatment has been used for hyperpigmentation with limited success.
Stitch Marks
Tensionless suturing is the best way to avoid stitch marks. To minimize stitch marks, the use of skin hooks rather than forceps and a subcuticular method of suturing are desirable. If a simple interrupted suturing technique is adopted, fine sutures (i.e., 7-0) should be used and early removal (i.e., 3 days) is preferred.
Step-off Deformities
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


