Facial nerve paralysis is one of the most devastating peripheral nerve injuries, and patients with facial palsy suffer from massive functional and esthetic problems.
Aims
For every patient, an individualized solution has to be made considering the underlying disease, the patient’s desire, age, and life expectancy. The aim must be to provide the patient with the best possible esthetic appearance of the face at rest and during motion. Usually, combinations of procedures have to be used. Static procedures alone aim at an improved appearance of the face at rest but fail to rehabilitate the patient when expressing emotions and for swallowing and speaking. Some static procedures improve the patient’s situation for a defined time period only.
Anatomy Of The Facial Nerve
Injuries of the facial nerve not only cause a paresis of the target muscles. Because the facial nerve is responsible for the range of facial expressions, injuries to the nerve cause serious disturbances in social life due to impairment in the translation of emotions to others.
The facial nerve is a mixed motor and sensory nerve with the main function of innervation of the muscles of voluntary facial expression. It originates from the homolateral facial nucleus in the caudal pons. Cortical projections to the facial nuclei pass through the internal capsule into the pons, where they diverge, innervating both the contralateral and the homolateral nucleus.
Autonomic fibers from the greater petrosal nerve reach the sphenopalatine ganglion and supply the lacrimal and nasal minor salivary glands. Next within the facial canal, the nerve to the stapedius muscle exits, followed by the chorda tympani nerve, which provides taste efference from the anterior tongue and secretor motor efference to the submandibular gland approximately 5 mm proximal to the stylomastoid foramen.
Because the facial nerve travels through the labyrinthine segment of the facial canal and the greater petrosal nerve (exiting anteriorly) and the geniculate ganglion resides anterior to the somatic motor fibers, turning at the first genoposteriorly into the tympanic or horizontal segment, the facial canal is smallest in diameter in this segment ( Fig. 28-1 ). More than 90% of facial nerve injuries from blunt temporal bone trauma occur in this region as a result of the traction forces exerted by its three branches.
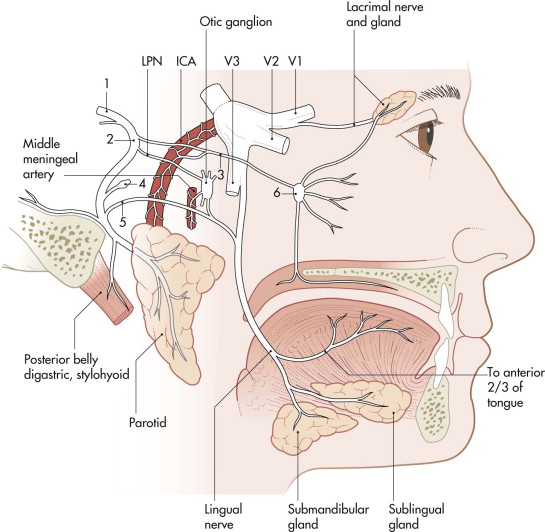
Lesions proximal to the meatus and within segments of the fallopian canal cause disturbances of tear and saliva production and taste sensation, impairment of the stapedius muscle, and various patterns of facial paralysis. Lesions distal to the stylomastoid foramen result in selective dysfunction of the facial muscles.
At the exit from the stylomastoid foramen, the facial nerve divides into the temporofacial and the cervicofacial branches (see Fig. 28-1 ). At the pes anserinus, five classic distal branches: temporal, zygomatic, buccal, mandibular, and cervical. The temporofacial branch anastomoses with the auriculotemporal nerve (cranial nerve V3) and divides into branches destined for the cutaneous muscles of the skull and face. It leaves as the:
- •
superior buccal branches (buccinator, upper part of the orbicularis oris muscles).
- •
infraorbital branches (greater and lesser zygomatic muscles, levators of the upper lip and nasal alae, transverse and dilator nasal muscles).
- •
frontal and palpebral branches (palpebral part of the orbicularis oculi, frontal part of the epicranius muscles).
- •
temporal branches (muscles of the outer aspect of the external ear).
After the anastomosis of the cervicofacial branch with the auricular branch of the cervical plexus, the branch divides into several others in the region of the mandibular angle:
- •
Inferior buccal branches (lower half of the orbicularis oris muscle)
- •
Cervical branch (platysma)
Anatomy Of The Facial Nerve
Injuries of the facial nerve not only cause a paresis of the target muscles. Because the facial nerve is responsible for the range of facial expressions, injuries to the nerve cause serious disturbances in social life due to impairment in the translation of emotions to others.
The facial nerve is a mixed motor and sensory nerve with the main function of innervation of the muscles of voluntary facial expression. It originates from the homolateral facial nucleus in the caudal pons. Cortical projections to the facial nuclei pass through the internal capsule into the pons, where they diverge, innervating both the contralateral and the homolateral nucleus.
Autonomic fibers from the greater petrosal nerve reach the sphenopalatine ganglion and supply the lacrimal and nasal minor salivary glands. Next within the facial canal, the nerve to the stapedius muscle exits, followed by the chorda tympani nerve, which provides taste efference from the anterior tongue and secretor motor efference to the submandibular gland approximately 5 mm proximal to the stylomastoid foramen.
Because the facial nerve travels through the labyrinthine segment of the facial canal and the greater petrosal nerve (exiting anteriorly) and the geniculate ganglion resides anterior to the somatic motor fibers, turning at the first genoposteriorly into the tympanic or horizontal segment, the facial canal is smallest in diameter in this segment ( Fig. 28-1 ). More than 90% of facial nerve injuries from blunt temporal bone trauma occur in this region as a result of the traction forces exerted by its three branches.
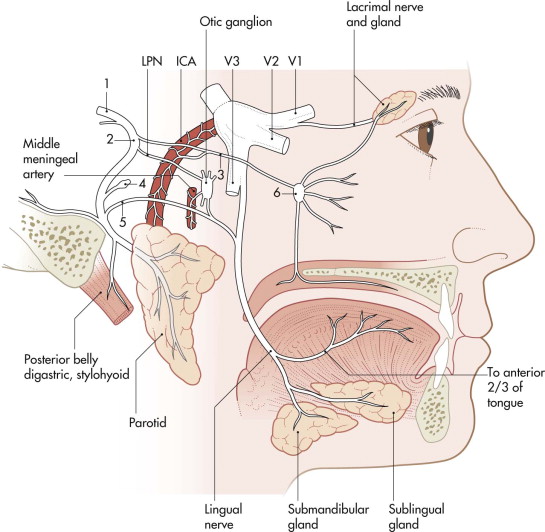
Lesions proximal to the meatus and within segments of the fallopian canal cause disturbances of tear and saliva production and taste sensation, impairment of the stapedius muscle, and various patterns of facial paralysis. Lesions distal to the stylomastoid foramen result in selective dysfunction of the facial muscles.
At the exit from the stylomastoid foramen, the facial nerve divides into the temporofacial and the cervicofacial branches (see Fig. 28-1 ). At the pes anserinus, five classic distal branches: temporal, zygomatic, buccal, mandibular, and cervical. The temporofacial branch anastomoses with the auriculotemporal nerve (cranial nerve V3) and divides into branches destined for the cutaneous muscles of the skull and face. It leaves as the:
- •
superior buccal branches (buccinator, upper part of the orbicularis oris muscles).
- •
infraorbital branches (greater and lesser zygomatic muscles, levators of the upper lip and nasal alae, transverse and dilator nasal muscles).
- •
frontal and palpebral branches (palpebral part of the orbicularis oculi, frontal part of the epicranius muscles).
- •
temporal branches (muscles of the outer aspect of the external ear).
After the anastomosis of the cervicofacial branch with the auricular branch of the cervical plexus, the branch divides into several others in the region of the mandibular angle:
- •
Inferior buccal branches (lower half of the orbicularis oris muscle)
- •
Cervical branch (platysma)
Functional Problems
Causes Of Injuries
Unilateral palsy or paralysis of the face can be divided into damage above the upper motor neuron and damage involving the lower motor neuron and its distal termination on the facial musculature. Supranuclear palsy spares the frontalis muscle because of the bilateral innervation of the nucleus from both cerebral hemispheres. In these supranuclear palsies, the facial involvement is often the most minor part of the patient’s problems.
Lesions of the lower motor neuron usually involve the entire face. Nuclear lesions usually involve adjacent brainstem structures (abducens, trigeminal nerve). The part of the nerve most commonly damaged appears to lie within the facial canal and at each end of the canal.
The largest etiological category of facial palsy is idiopathic facial palsy (Bell’s palsy), which is often diagnosed by exclusion of other etiologies. It is characterized by a rapid onset of unilateral facial palsy including movements of the forehead, orbicularis oculi, perioral muscles, and platysma. Defective taste sense (anterior two thirds of the tongue) and hyperacusis may additionally be present. The etiology of Bell’s palsy is unknown. There are a number of other causes of facial nerve palsies, which are listed in Box 28-1 .
Congenital
Moebius syndrome (congenital nuclear aplasia) (possibly + palsy of external rectus muscles)
Myotonic dystrophy
Melkersson-Rosenthal syndrome + lingua plicata, swelling of the face/upper lip
Congenital cholesteatoma/congenital facial nerve palsy
Neurological
Myasthenia gravis
Multiple sclerosis
Guillain-Barré syndrome
Neoplastic
Facial nerve tumors (schwannoma, neurofibroma, neurogenic sarcoma)
Glomus tumors (glomus jugulare/tympanicum)
Others (meningioma, acoustic neuroma)
Parotid tumors
Temporal bone/external auditory canal tumors
Infectious
Otitis media
Bacterial causes (diphtheria, tuberculosis)
Viral causes (herpes zoster oticus, mumps, infectious mononucleosis)
Other Causes
Toxic
Metabolic
Idiopathic
Iatrogenic
Parotidectomy
Rhytidectomy
Lateral skull base surgery
Traumatic
Temporal bone fractures (longitudinal, transverse)
Penetrating trauma (gunshot)
Facial lacerations
High altitude palsy
Central upper facial nerve injuries may occur as a result of tumor surgery at the cerebellopontine angle or from skull base fractures or trauma. In its extracranial course, the facial nerve is most often injured by sharp lacerations. However, the most frequent cause of injury is iatrogenic, occurring during resection of tumors in the parotid gland. Under these conditions, immediate microsurgical repair, including the use of grafts, is indicated. Resection of malignant parotid gland or skull base tumors may necessitate resection of branches of the facial nerve or the nerve itself. It must be decided on an individual basis whether a primary reconstruction of the facial nerve using nerve grafts is indicated. In trauma situations with obvious separation of the facial nerve or its branches, an immediate coaptation must be performed. If during primary trauma care, injury is only suspected or not proved, an expectant attitude should be preferred.
Investigation Of Facial Nerve Functions
In the clinical investigation of a patient with a facial palsy, determination of onset characteristics is very important. In patients with Bell’s palsy, an acute onset (e.g., on waking in the morning after normal facial motion the night before) is typical. Sudden onset may also be present in infectious or inflammatory conditions affecting the facial nerve (e.g., herpes zoster oticus, multiple sclerosis). Patients with tumors usually demonstrate progressive paresis over long periods with initially mild symptoms (e.g., weakness of the labial depressor muscle).
In trauma patients, a delayed onset of facial palsy carries a significantly better prognosis than immediate onset. Associated symptoms may also indicate certain diseases. Oral pain, respiratory infections, and hearing loss may accompany acute otitis media, whereas initial fever, arthritis, and neuropathies may be indicative of Lyme disease. Herpes zoster oticus shows typical additional symptoms (i.e., vesicular eruptions, severe pain).
Temporal bone neoplasms may cause other cranial nerve involvements (cochlear/vestibular nerves and cranial nerves IX, X, and XI → jugular foramen; cranial nerves V, VI, and VII → temporal bone). Lesions of the second, third, fourth, and sixth cranial nerves may suggest multiple sclerosis.
First, a careful observation of voluntary facial movements is undertaken. The symmetry of forehead wrinkling is investigated when the patient is asked to raise the brows. A functioning orbicularis oculi muscle allows for complete closure of the eyelids and absence of visible upward rotation and exposure of the sclera (Bell’s phenomenon).
A forced wide smile distinguishes symmetries of the perioral muscles depending on the buccal and marginal mandibular branches. Comparison of the depth of the nasolabial folds and the symmetrical contraction of the platysma muscle is also important. The Schirmer test measures tear production over a 5-minute period.
Objective methods of determining the secretory function of the parotid and submandibular glands exist. Pure taste sensation may be investigated by using samples of sweet, bitter, acid, and salty substances on the anterior tongue. An audiological investigation may reveal the dysacusis caused by a nonfunctional stapedius muscle, which usually moves the tympanic membrane inward for sound absorption. Laboratory tests of sedimentation rate, treponemal antibody titer, and Lyme disease titer are scheduled. High-resolution computed tomography (CT) is indicated for patients with suspected temporal bone disease (e.g., skull base fracture). Magnetic resonance imaging (MRI) is indicated to detect lesions at the cerebellopontine angle. The typical symptoms of facial nerve injuries are listed in Box 28-2 .
-
Complete peripheral facial paralysis:
- •
Ipsilateral forehead: absence of frontalis function
- •
Brow ptosis
- •
No closure of upper eyelid
- •
Drooping of lower eyelid
- •
In closing the eyelids, the globe rotates upward, resulting in a visible sclera (Bell’s phenomenon)
- •
Absence of nasolabial fold; corner of mouth droops downward
- •
Generalized flattening of the face
- •
-
Central facial paralysis (cerebral vascular accident; tumor above the level of the facial nucleus):
- •
Function of frontalis muscles and orbicularis oculi preserved (uncrossed fibers maintain innervation to the upper face)
- •
Bell’s phenomenon not present
- •
Involuntary expression of emotion often preserved
- •
-
Lesion of the facial nucleus in the pons:
- •
Symptoms like those of peripheral paralysis
- •
Tear and saliva production preserved
- •
Taste sensation of the anterior two thirds of the tongue preserved (intermedial nerve enters the facial nerve caudally)
- •
-
Facial nerve lesions at the cerebellopontine angle cephalad to internal auditory meatus (i.e., acoustic neuroma):
- •
Complete peripheral facial paralysis
- •
Tearing, salivation, and taste often abnormal (intermedial nerve approaches the internal auditory meatus)
- •
Stapedius muscle function impaired
- •
-
Facial nerve lesion caudal to the geniculate ganglion, cephalad to the nerve stapedial branch:
- •
Complete peripheral facial paralysis (e.g., lesion at the internal auditory meatus)
- •
Exception: lacrimal gland production preserved (greater petrosal and sphenopalatine ganglion)
- •
Lesions between the stapedial nerve and the chorda tympani: normal tear production, normal stapedial muscle function with complete peripheral facial paralysis
- •
Lesions caudal to the chorda tympani: peripheral extracranial paralysis
- •
-
Facial nerve lesion at the stylomastoid foramen:
- •
Complete peripheral nerve paralysis (no disturbance of tear/saliva production, taste, stapedius muscle function)
- •
-
Lesions occurring within the confines of the parotid gland:
- •
Selective paralysis of voluntary motor functions
- •
Paralysis of temporal branch: asymmetrical motion of the forehead, some dysfunction of the upper and possibly the lower eyelid
- •
Paralysis of zygomatic branch: paralysis of the muscles zygomaticus major, zygomaticus minor, levator anguli oris, levator superioris—impairment of smile
- •
Paralysis of buccal branch: buccinator muscle, orbicularis oris muscle distortion—buccozygomatic connections make complete branch dysfunction rare
- •
Paralysis of mandibular branch: innervates muscles triangularis, risorius, quadratus labii inferioris, mentalis, orbicularis oris—asymmetry of smile, affected commissure pulled upward and internally rotated
- •
Paralysis of cervical branch: innervation of platysma, little functional loss in cases of injury
- •
The House-Brackmann classification is often used for rating facial palsy. Grade I refers to normal function without weakness; slight facial asymmetry with a minor degree of synkinesis is classified as grade II. Obvious but not disfiguring asymmetry (e.g., with contracture or hemifacial spasm but residual forehead movement) is judged as grade III. Grade IV represents obvious, disfiguring asymmetry with lack of forehead motion and incomplete eye closure. Asymmetry at rest and only slight facial movement is rated as grade V. Complete absence of tone or motion is grade VI.
Electromyography (EMG) and electroneurography are routinely employed. In cases of acute injury, nerve excitability tests are used, but normal results are less reliable than abnormal results, because functional deficits may occur at a later time. EMG analyzes the function of the muscles during needle insertion and gives information on the existence of spontaneous activity (action potentials) arising from voluntary muscle contraction. Spontaneous activity indicates a pathological process within the nerve, whereas fibrillation potentials may be a sign of nerve disruption.
During evoked EMG, a supramaximal stimulus is applied at the skin surface near the stylomastoid foramen. Intact axons will provide action potentials that can be recorded distally. In facial nerve injury, the amplitude of the action potential is defined as a percentage of the amplitude on the normal side. Magnetic transcranial and electrical stylomastoid stimulation procedures allow for differentiation of lesions and distinction between central and peripheral facial nerve palsies.
Principles
Surgical Management
If the distal facial nerve branches and musculature are intact, reinnervation from the proximal facial nerve is ideal. Reinnervation using another motor nerve may be indicated if the proximal facial nerve cannot be identified. Cases with partial return of nerve function are always problematical. The risk of destruction of functional nerve branches during surgery must be weighed against the possible advantages of reconstructive procedures.
The following basic strategies are applied most frequently for surgical correction of facial paralysis and its sequelae.
In light of the types of nerve injury and the general chance of a spontaneous regeneration in neurapraxia and axonotmesis, exact information about the mechanism of the facial nerve injury is mandatory. In cases of a sharp transection in the absence of significant adjacent soft tissue trauma or infection, immediate primary management by a well-trained operating team may be indicated.
Often, it is not known what type of nerve injury is present. Although peripheral dissected facial nerve branches may be identified under magnification or with electrical stimulation, the clinical consequences of these injuries often cannot be judged immediately. Therefore, during primary wound closure, suspected branches of the facial nerve are marked with non-resorbable sutures. The suture material is positioned at the external wound surface to help identify the nerve fibers at a later stage. This allows assessment of the clinical consequences of a nerve injury and performance of micronerve anastomosis under sterile conditions. Primary nerve grafting procedures are avoided.
Nerve reconstruction is performed immediately or within 2 months after the injury through the use of direct nerve coaptation or placement of a nerve graft.
Reconstructions of the facial nerve are limited by the atrophy of the musculature that occurs 6 to 12 months after the injury. Reanimation procedures such as faciofacial and 7th-to-12th nerve (VII-XII) anastomosis are performed not earlier than 6 to 12 months after the trauma. In long-standing facial nerve palsy, muscle grafts are often necessary due to the increasing atrophy of the facial muscles. A suggested algorithm of a staged facial reanimation is shown in Box 28-3 (modified after Volk et al. ).
- 1
Early reconstruction:
-
Direct nerve suture
-
Interpositional graft
-
Lid loading
-
(Additional soft tissue procedures)
-
- 2
Early/delayed reconstruction (eventual impossibility of performing step 1):
-
Hypoglossal/facial jump anastomosis
-
Lid loading
-
Cross-face nerve suture
-
Masticatory muscle transfer
-
(Eyebrow lift/nasolabial fold creation/eyebrow lift)
-
- 3
Late reconstruction:
-
Mimic musculature existing
-
Hypoglossal/facial jump anastomosis
-
Lid loading
-
Cross-face nerve suture
-
Mimic musculature not existing
-
Microvascular muscle transfer
-
Temporalis muscle transfer (nasolabial fold creation/eyebrow lift/face-lift)
-
Microsurgical Techniques
In all microsurgical techniques for facial nerve reconstruction, attempts should be made to get impulses from the ipsilateral facial nerve, such as by a surgical preparation of the nerve out of the tumor or by the use of nerve grafts. If these possibilities do not exist, other procedures (e.g., VII-XII procedures) may be considered.
In cases of primary or early secondary nerve reconstruction after a defined injury, direct identification and preparation of the nerve stumps is usually possible. Coaptation or grafting techniques can then be performed easily.
In secondary microsurgical nerve repair, exploration of the site of the lesion and the stumps of the facial nerve always follows a certain order, especially in cases of peripheral facial nerve palsies in which the extent of the injury is uncertain.
It is easy to identify the facial nerve stumps that have been marked with sutures beforehand. In older secondary lesions, this is not possible, and in these cases, the first step is the systematic preparation of the extratemporal course of the central facial nerve. The identification of the nerve at the stylomastoid foramen is the approach of choice, and tracing the nerve back from the periphery should be attempted only if the central approach is not possible.
The preauricular skin incision runs in an anteriorly curved fashion into the submandibular neck fold. The skin can then be dissected away from the fascia of the parotid gland. The cartilaginous auditory canal and the pointer, anterior to the tragus cartilage, are identified. The main trunk of the facial nerve lies approximately 1 cm caudal to that pointer at the transition level between the cartilaginous and the osseous auditory canal. If the origin of the sternocleidomastoid muscle at the mastoid and the biventer muscle are additionally prepared, the facial nerve trunk will be found to lie cranial to the angle created by these two muscles ( Fig. 28-2 ).
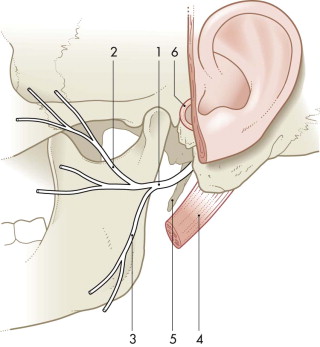
For further preparation, the fibrous tissue fibers between the parotid gland and the osseous auditory canal are separated step by step, and crossing vessels are carefully coagulated. Fatty tissue cranial to the facial nerve is mobilized anteriorly. Then, the approximately 2-mm-thick facial nerve stump is identified with the help of a nerve stimulator. The division into its main branches usually occurs after 1 cm. With a small trunk scissors, the tissue overlying the nerve is dissected away from the nerve and elevated. With a second scissors, this tissue is transected. In this manner, the branches are traced into the periphery of the gland. Among the peripheral branches, the marginal branch may be identified most easily. It lies lateral to the superficial neck fascia and crosses the facial artery and vein. Via the submandibular skin incision, it can be identified at the lateral surface of the submandibular gland and then traced dorsally.
At the superior border of the parotid gland, the temporal and zygomatic branches leave the parotid gland and are identified below the zygomatic arch in the subcutaneous tissue. The buccal branches are found cranial to Stensen’s duct.
After identification of the nerve branches, the first procedure in surgical intervention is external neurolysis with preparation of the tissue surrounding the nerve and resection of the scarred perineurium. If the nerve itself is scarred, intraneural neurolysis is performed to remove cicatricial compression of the nerve fiber bundles caused by an epineural or paraneural scar. Healthy perineurium is left intact so as not to interrupt the blood supply to the individual nerve bundles and the exchange of fibers among the various fascicles.
After neurolysis, the nerve is moved away from the scar tissue bed and placed into healthy tissue to avoid further scar formation.
Direct Nerve Suture Nerve Grafts
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


