Clinicians do not frequently see impacted dilacerated maxillary incisors in their patients. When they do, there are several diagnostic and management challenges for correcting root dilacerations. An unfavorable esthetic outcome might occur as a result of soft-tissue complications during surgical eruption procedures. We present 2 patients with an impacted and dilacerated maxillary central incisor. Computed tomography scans with 3-dimensional reformation were used to accurately assess the positions of the dilacerated teeth, the degree of dilaceration, and the stage of root formation. The therapy primarily involved 2-stage crown exposure surgery combined with orthodontic traction. An apicoectomy was performed on 1 dilacerated tooth; the other exhibited pulp vitality. This article highlights the periodontal surgical strategies for the esthetic management of inverted crowns. Through periodontal plastic surgery and interdisciplinary cooperation, the impacted dilacerated central incisors were properly aligned, and successful esthetic results were achieved.
Tooth dilaceration is a dental anomaly manifested by a sharp angulation of the longitudinal axis of a tooth. Maxillary incisor dilaceration is relatively rare and estimated to occur in up to 1% of all permanent dentitions. The dilacerated root can curve in a labiolingual or mesiodistal direction. The most common orientation of a dilacerated maxillary incisor is with the crown directed upward and labially. Therefore, surgical exposure and orthodontic forced eruption of impacted dilacerated incisors are particularly challenging because the dilacerated tooth can erupt in an awkward position. Moreover, the curved root can affect adjacent teeth or penetrate the labial cortical plate with sequelae of pulpal and periapical problems.
Although previous reports showed successful realignment of such teeth, unesthetic gingival contours of the exposed incisors might occur if periodontal problems are not properly managed. However, there is only a limited amount of illustrated literature on the soft-tissue management of impacted dilacerated incisors. The purpose of this article is to report the periodontal surgical strategies for the esthetic management of 2 patients with an impacted dilacerated maxillary central incisor. Comprehensive plans and treatment procedures were developed, and successful results were obtained with the cooperation of various specialists.
Case reports
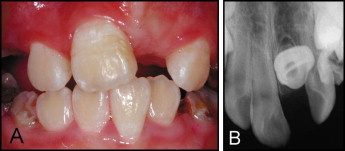
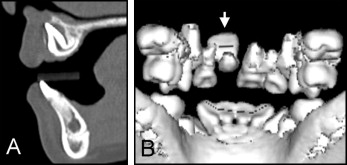
Patient 1, an 8-year-old girl with a complaint of delayed eruption of the maxillary left central permanent incisor, was referred to the Department of Orthodontics at Taipei Veterans General Hospital in Taiwan. She was physically healthy and had no history of dental trauma. She had an Angle Class I occlusion, with an overjet of 7 mm and an overbite of 3 mm. The maxillary left central permanent incisor was unerupted, and the adjacent teeth had migrated into this unoccupied space ( Fig 1 , A ). The periapical radiograph showed that the maxillary left central permanent incisor was impacted, and the crown edge was directed upward ( Fig 1 , B ). The 3-dimensional reformatted computed tomography images showed that the dilacerated incisor with the crown had rotated about 90°, its incisal tip was just below the floor of the nasal cavity, and its root formation was almost complete ( Fig 2 ).
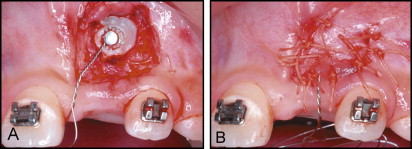
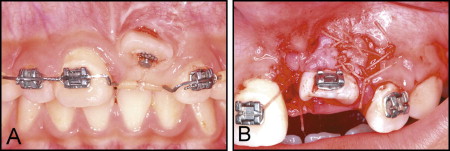
Our treatment plan involved surgical exposure and orthodontic eruption of the dilacerated tooth. Because of the severity of the dilacerated incisor root, the patient’s parents were informed that an apicoectomy during the tooth traction might be needed. After space redistribution and recreation of adequate space for the dilacerated incisor, surgical exposure with a closed-eruption technique was performed. An incision was made on the labial surface in the maxillary left central incisor region, and the flap was raised. A lingual button with a presecured ligature wire was bonded to the palatal surface of the exposed crown, which faced the oral cavity ( Fig 3 , A ). The flap was repositioned and closed with sutures ( Fig 3 , B ). A ligature wire was tied to the main archwire with an elastic thread. The soft tissues healed in 2 weeks, after which traction of the impacted incisor began.
The incisal edge of the impacted incisor was extruded outside the alveolar mucosa 4 months after tooth eruption, resulting in no keratinized tissue on the labial side of the crown ( Fig 4 , A ). To augment the keratinized mucosa, periodontal plastic surgery by using a double papilla flap from the interdental area of the adjacent teeth was performed ( Fig 4 , B ). In the meantime, the lingual button was replaced with a bracket bonded to the labial side of the crown, and traction was continued with an 0.018 × 0.022-in stainless steel wire. The root apex of the dilacerated incisor could be palpated just under the alveolar mucosa ( Fig 5 , A ) 3 months after surgery, and the patient complained of discomfort in this area. This tooth exhibited percussion pain and negative responses to the cavity test. The patient was transferred to the endodontist for root canal treatment and an apicoectomy with mineral trioxide aggregate retrograde filling ( Fig 5 , B and C ). Orthodontic treatment was restarted 2 months later, and the impacted incisor was then moved into a normal position. Total treatment time was about 19 months.

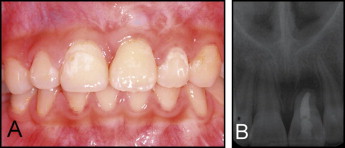
Through a 2-stage crown exposure surgery, the impacted maxillary left central incisor was successfully protracted into proper alignment with an acceptable gingival contour. The width of the keratinized gingiva was 3 mm ( Fig 6 , A ). A posttreatment radiograph 1 year later showed no specific pathology of the tooth or its periapical tissue ( Fig 6 , B ).
Patient 2, an 8-year-old girl, was referred for orthodontic consultation regarding an unerupted maxillary left central permanent incisor. She had experienced trauma in the maxillary deciduous incisor region at the age of 4 or 5 years.
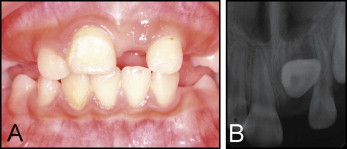
The clinical examination showed that she had mixed dentition, with an Angle Class II molar relationship and a maxillary dental midline that deviated to the left side. A severe space deficiency in the bimaxillary arch was also noted. Overjet was 4 mm, and overbite was 5 mm ( Fig 7 , A ). A periapical radiograph showed that the maxillary left central incisor was impacted ( Fig 7 , B ). A computed tomography scan showed that the dilacerated incisor had a crown-root angle of 120°, with less than one-third of normal root formation ( Fig 8 ).