
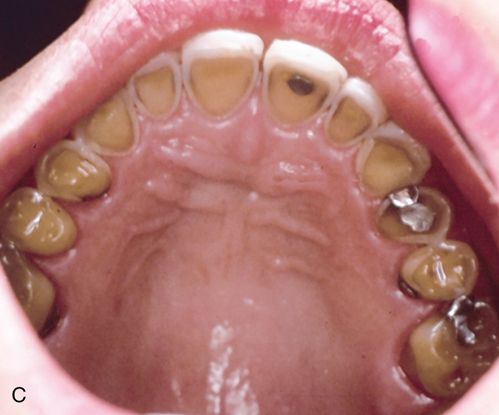


In eating disorders that involve frequent purging, perimylolysis12 is often associated with the excessive self-induced vomiting that occurs (Figs. 29-1 C,D).
Sufferers of ED often consume an excessive amount of caffeinated and/or carbonated drinks, sweetened beverages, sweets, and/or sugared chewing gum (often used to quickly boost energy levels and to decrease reflex hunger pangs through inducing stomach dilation.)9
Chronic purging can lead to dental erosion on all tooth-related surfaces (palatal, labial, lingual, and buccal surfaces). 12 The eroded enamel has a texture that is smooth, shiny, and hard and if extensive enough the yellowish color of the dentin becomes more prominent and observable and the teeth might become hypersensitive to temperature changes.
Mucosal lesions
Mucosal lesions may lead to generalized mucosal atrophy, stomatitis and oral ulcers.13 Oral lesions are particularly evident on the tongue, buccal mucosa, and the floor of the mouth.14
In eating disorders, erythematous mucosal lesions of the soft palate may be the direct result of gastric acid contact during vomiting (epithelial erosion) or the trauma caused by the object used to induce purging such as fingers, fingernails, toothbrushes, etc. (Fig. 29-1 E).
Periodontal manifestations
Periodontal manifestations are more frequently observed in adults, but can also be detected in teen and pediatric ED sufferers. Compromised oral hygiene can lead to gingival inflammation and future periodontitis.15 Based on the clinical and anecdotal observations of the author, patients prone to depression and who binge eat and/or purge, often care little about proper oral care.
Salivary and salivary gland manifestations
Sialadenosis, a noninflammatory enlargement of the salivary glands caused by peripheral autonomic neuropathy can be a marker of ED (Fig. 29-2 A).


This often results in acinar enlargement and functional impairment. In addition, salivary flow may be reduced.9 At times dry mouth may be associated with medications used in the treatment of ED (e.g., Prozac (fluoxetine) and Lexapro (escitalopram oxalate) or the earlier generation of tricyclic antidepressants (e.g., amitriptyline).16-18
In addition, necrotizing sialometaplasia has been reported to be associated with bulimia.9
Dermatologic manifestation
Self-induced vomiting by finger stimulation of the palatal gag reflex can result in callouses on the knuckles (Russell’s sign; Fig. 29-2 B).19 This occurs when the incisal edges of the maxillary anterior teeth repeatedly contact the knuckles during this manipulation.
Considerations when approaching a patient presenting with suspected symptoms of an eating disorder
Generally speaking, when a covert disorder or disturbance is suspected on either a sensitive medical or dental issue manifest in a discussion with a patient, a defensive posture or response on the part of the patient is to be expected. If a dental practitioner raises concerns with a patient that an eating disorder may be present, such emotional responses as resentment, denial, or resistance towards suggestions for treatment intervention is to be expected. Notwithstanding such possible negative or avoidant responses on the patient’s part, the practitioner has a professional obligation to address potential or probable medical or health concerns. For example, if a patient presents symptoms suggestive of COPD, the dentist should address this concern, including follow-up recommendations for appropriate care. No less concern should be registered when an eating disorder is suspected.
What is most distressing concerning patients who appear to meet criteria consistent with a diagnosable eating disorder is that, based on one comprehensive study, fewer than half actually obtain medical care from a medical provider, and only approximately 28% consulted with a mental health care professional.20
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


