In the past century of orthodontic history, diagnosis and treatment planning have focused primarily on the anteroposterior (AP) skeletofacial dimension. Not surprisingly, the current classification system of malocclusions remains as described by Edward Angle, which in essence does not provide any information regarding the vertical or transverse dimension.
It took decades before the importance of the vertical facial dimension was highlighted. Sassouni and S. Nanda were among the first to describe the vertical proportions of the face and the skeletal characteristics associated with open bites and deep bites. Nanda later found that the vertical facial pattern was established early in life and maintained through growth. Therefore, this finding implied that in order to affect the vertical growth pattern, a therapeutic intervention was necessary.
Although the vertical dimension lends itself to mechanical control, alteration of the vertical facial pattern is difficult, and instability with treatment may be expected. Many have contended that adequate control of the vertical dimension is crucial for a successful AP correction. A clear reciprocity exists between the dimensions.
There are two extremes in the vertical facial pattern: (1) excessive vertical growth and (2) deficient vertical facial height. Many terms have been used to describe excessive facial height, including hyperdivergency, high angle, dolichofacial pattern, and leptoprosopic pattern. Likewise, terms used to describe reduced facial height have included hypodivergency, low angle, brachyfacial pattern, and euryprosopic pattern. The dolichofacial pattern is often associated with an open-bite malocclusion and the brachyfacial pattern with a deep-bite malocclusion.
It is important to be aware that the occlusal relationship does not always follow the facial pattern because dental compensations are usually found at both extremes. Additionally, there are ranges of vertical excess, and some patients may not present with an extreme type of vertical pattern, but rather with a slight or moderate tendency toward one of the two extremes.
The purpose of this chapter is to describe the characteristics of excessive vertical skeletofacial pattern and outline different mechanics for its correction. Also, the soft tissue, skeletal, and dental characteristics of a vertical skeletofacial pattern are discussed, as well as their influence on the outcome of the vertical facial form. Different treatment alternatives are presented, each addressing the problem from a different perspective. Furthermore, the importance of timing is emphasized because treatment decisions differ significantly between growing and nongrowing patients.
ETIOLOGY OF DOLICHOFACIAL PATTERN
The dolichofacial pattern can be attributed primarily to genetic factors, although environmental factors are also considered important in establishing this pattern. The heritability of the facial heights has been studied in monozygotic and dizygotic twins, in whom the lower facial height appears to be under strong genetic influence. Research studies evaluating the environmental causes of the dolichofacial pattern have attributed abnormal function such as mouth breathing, abnormal swallowing, and tongue posture as primary etiologic factors. However, the concept of environmental causes as the sole etiology responsible for establishment of the dolichofacial pattern is strongly debated.
The influence of the soft tissues is evident in the dolichofacial pattern via the muscle architecture. Indeed, it has been suggested the masticatory muscles in individuals with a vertical excess exert a diminished occlusal force compared to individuals with a normofacial or brachyfacial pattern. Boyd et al. described the masseter muscles in these individuals as having a higher percentage of type II (fast) fiber muscles. On the contrary, Rowlerson found greater percentages of type II fibers in the brachyfacial sample. Korfage et al. noted that the discrepancy in these findings may be caused by the large intraindividual and interindividual variability. Analyzing and identifying the type of muscle fiber may ultimately be important in the treatment of these patients, but it may also have connotations in the long-term stability of treatment.
CHARACTERISTICS OF VERTICAL EXCESS
Vertical excess has specific skeletal, dental, and soft tissue characteristics. The soft tissue characteristics can be evaluated clinically, anthropometrically, and cephalometrically. The analysis of the vertical dimension is possible from a frontal and a profile view. The absolute length measurements in the vertical distances between anatomic landmarks are not as important as the proportions of the face. To evaluate these proportions, the face is initially divided into equal thirds, with the middle and lower third being the most important because they contain the majority of facial structures. More specifically, the lower third is of utmost importance because is it is the facial area that can be significantly altered with orthodontic treatment.
The lower third of the face can be further divided into thirds: the inferior two thirds from stomium to menton and the superior one third from subnasale to stomion. Existing disproportions can be evaluated though the analysis of these measurements, but clinically one of the most important characteristics of the vertical facial excess is found in the lower facial third: a large “interlabial gap” at rest. The presence of a large interlabial gap can be further confirmed when the patient closes the lips lightly and mentalis muscle strain is noticed. Another clinical characteristic associated with a large interlabial gap in patients with vertical facial excess is an excessive gingival display on smile. Keep in mind that the large interlabial gap and excessive gingival display may not result exclusively from vertical facial excess, but rather may be caused partially or totally by a short upper lip. Comparison of a patient’s lip length to normative data can help determine any deficiencies.
The lateral cephalometric radiograph is the most common means used to evaluate, quantify, and classify a patient with vertical facial excess. These radiographic findings can be correlated with the clinical and anthropometric analysis. Other useful skeletofacial measurements and ratios may be obtained by a lateral cephalogram; for example, upper and lower hard tissue facial heights can be determined. Ideally, the face should be divided anteriorly into two halves, with the upper half slightly smaller than the lower half (45 : 55). Using the lateral cephalogram, the relationship between the anterior and posterior facial height may also be evaluated. On average, the posterior facial height measured from sella to gonion should be approximately 60% of the anterior facial height.
One of the most common cephalometric measurements used to classify a patient as “hyperdivergent” is the inclination of the mandibular plane. An angle measurement above 36 degrees to the sella-nasion plane is usually an important indicator of vertical facial excess. Other characteristics suggestive of this pattern, as described by Björk, are growth indicators that anticipate the development of extreme facial excess. He believed that these features serve as predictive characteristics of what has been described as “backward growth,” which ultimately develops into a dolichofacial pattern.
Finally, in the lateral cephalogram, vertical dental characteristics can be measured and compared to normative data. Of these, the dentoalveolar heights in the maxilla and the mandible are measured to the palatal plane and the mandibular plane, respectively. The occlusal table of the first molar to these reference lines usually is excessive in these patients, especially the maxillary molar to the palatal plane. Anteriorly, the distance from this reference plane may also be excessive, that is, palatal plane to the maxillary central incisor. In this case, although a vertical facial pattern is evident, an open bite would not be seen anteriorly because the incisors may have supraerupted, compensating for the posterior vertical excess. It is important to note that although a patient may have a dolichofacial pattern, only a small percentage of these patients have a corresponding anterior open bite.
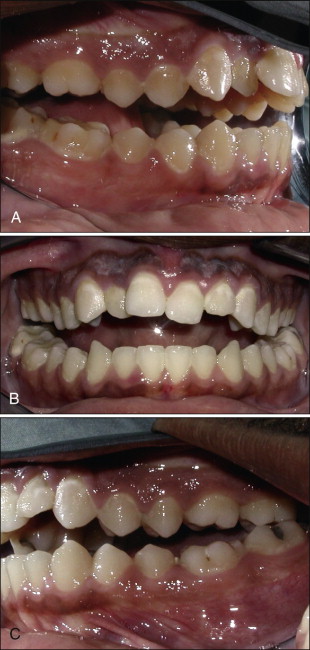
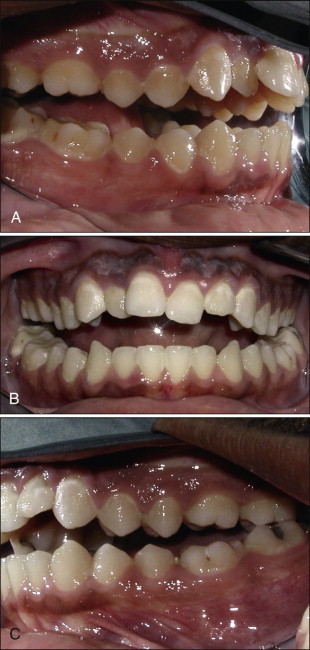
The differentiation between a skeletal and a dental open bite has been controversial. As just described, the major characteristics of a skeletal open bite are determined through cephalometric measurements. Usually a dental open bite is related to a habit that inhibited the vertical development of the incisors. The open bite can also be initiated or perpetuated by a tongue thrust. Diverging occlusal planes anterior to the premolars is a feature that may be indicative of a dentoalveolar open bite. This clinical and cephalometric feature is usually caused by a finger habit. On the contrary, skeletal open bites generally display two occlusal planes that start diverging more posteriorly than the first premolar, usually from the second premolar or first molar ( Fig. 15-1 ).
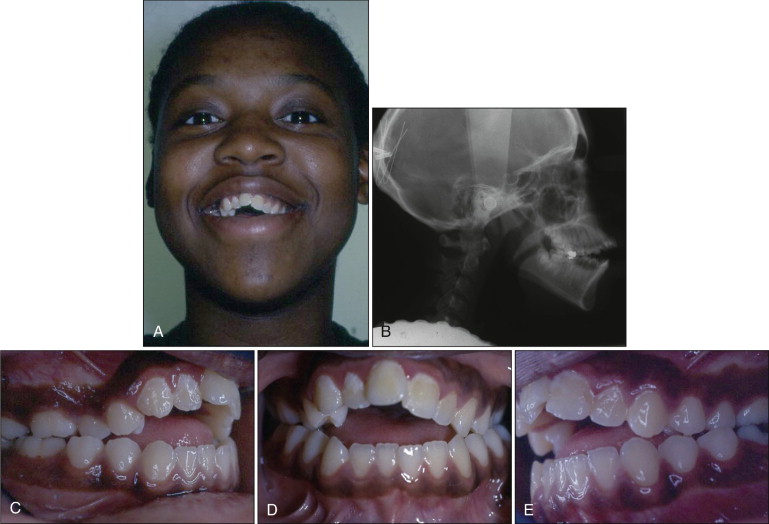
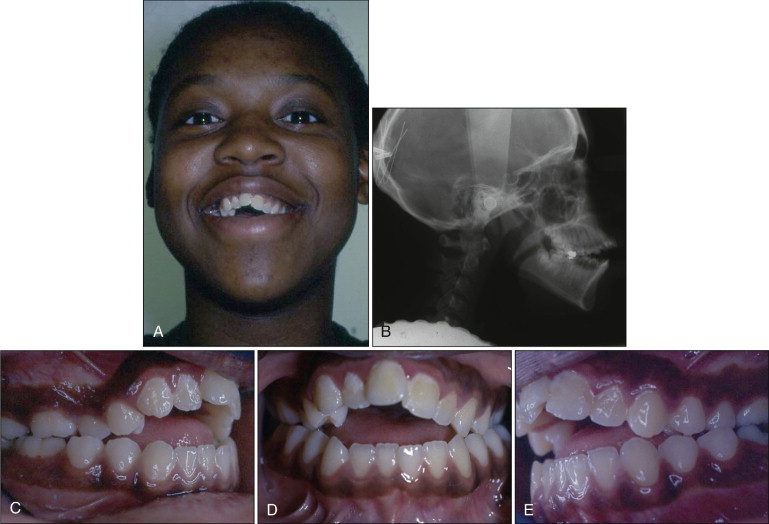
A clear distinction between the two types is generally not obvious, and often some individuals with vertical facial excess may have a habit (e.g., thumb sucking) and thus features of both skeletal and dental open bite ( Fig. 15-2 ).
CHARACTERISTICS OF VERTICAL EXCESS
Vertical excess has specific skeletal, dental, and soft tissue characteristics. The soft tissue characteristics can be evaluated clinically, anthropometrically, and cephalometrically. The analysis of the vertical dimension is possible from a frontal and a profile view. The absolute length measurements in the vertical distances between anatomic landmarks are not as important as the proportions of the face. To evaluate these proportions, the face is initially divided into equal thirds, with the middle and lower third being the most important because they contain the majority of facial structures. More specifically, the lower third is of utmost importance because is it is the facial area that can be significantly altered with orthodontic treatment.
The lower third of the face can be further divided into thirds: the inferior two thirds from stomium to menton and the superior one third from subnasale to stomion. Existing disproportions can be evaluated though the analysis of these measurements, but clinically one of the most important characteristics of the vertical facial excess is found in the lower facial third: a large “interlabial gap” at rest. The presence of a large interlabial gap can be further confirmed when the patient closes the lips lightly and mentalis muscle strain is noticed. Another clinical characteristic associated with a large interlabial gap in patients with vertical facial excess is an excessive gingival display on smile. Keep in mind that the large interlabial gap and excessive gingival display may not result exclusively from vertical facial excess, but rather may be caused partially or totally by a short upper lip. Comparison of a patient’s lip length to normative data can help determine any deficiencies.
The lateral cephalometric radiograph is the most common means used to evaluate, quantify, and classify a patient with vertical facial excess. These radiographic findings can be correlated with the clinical and anthropometric analysis. Other useful skeletofacial measurements and ratios may be obtained by a lateral cephalogram; for example, upper and lower hard tissue facial heights can be determined. Ideally, the face should be divided anteriorly into two halves, with the upper half slightly smaller than the lower half (45 : 55). Using the lateral cephalogram, the relationship between the anterior and posterior facial height may also be evaluated. On average, the posterior facial height measured from sella to gonion should be approximately 60% of the anterior facial height.
One of the most common cephalometric measurements used to classify a patient as “hyperdivergent” is the inclination of the mandibular plane. An angle measurement above 36 degrees to the sella-nasion plane is usually an important indicator of vertical facial excess. Other characteristics suggestive of this pattern, as described by Björk, are growth indicators that anticipate the development of extreme facial excess. He believed that these features serve as predictive characteristics of what has been described as “backward growth,” which ultimately develops into a dolichofacial pattern.
Finally, in the lateral cephalogram, vertical dental characteristics can be measured and compared to normative data. Of these, the dentoalveolar heights in the maxilla and the mandible are measured to the palatal plane and the mandibular plane, respectively. The occlusal table of the first molar to these reference lines usually is excessive in these patients, especially the maxillary molar to the palatal plane. Anteriorly, the distance from this reference plane may also be excessive, that is, palatal plane to the maxillary central incisor. In this case, although a vertical facial pattern is evident, an open bite would not be seen anteriorly because the incisors may have supraerupted, compensating for the posterior vertical excess. It is important to note that although a patient may have a dolichofacial pattern, only a small percentage of these patients have a corresponding anterior open bite.
The differentiation between a skeletal and a dental open bite has been controversial. As just described, the major characteristics of a skeletal open bite are determined through cephalometric measurements. Usually a dental open bite is related to a habit that inhibited the vertical development of the incisors. The open bite can also be initiated or perpetuated by a tongue thrust. Diverging occlusal planes anterior to the premolars is a feature that may be indicative of a dentoalveolar open bite. This clinical and cephalometric feature is usually caused by a finger habit. On the contrary, skeletal open bites generally display two occlusal planes that start diverging more posteriorly than the first premolar, usually from the second premolar or first molar ( Fig. 15-1 ).
A clear distinction between the two types is generally not obvious, and often some individuals with vertical facial excess may have a habit (e.g., thumb sucking) and thus features of both skeletal and dental open bite ( Fig. 15-2 ).
VERTICAL EXCESS AND SMILE ESTHETICS
Smile esthetics has always been a common goal among all the disciplines in dentistry. In the past, orthodontics emphasized the attainment of good occlusion as the primary goal, and alignment of the dental arches was the most important factor in achieving esthetics.
Recently, more characteristics have been defined to describe the esthetic smile. One of these characteristics related to the vertical dimension is the incisor display or gingival tissue display at rest and smile. This characteristic can be categorized as excessive, normal, or deficient. The excessive display may be caused by excessive vertical height of the maxilla, supraeruption of the upper incisors, short upper lip, or a combination of all these factors. The clinical diagnosis of the vertical excess is evaluated in the posed smile; therefore a differential diagnosis is necessary through the evaluation of lip mobility. A hypermobile lip will give the appearance of vertical maxillary excess because a significant amount of gingival tissue will be displayed at smile, even though the amount of incisor display at rest may be normal. Thus a patient may have excessive gingival display at smile without vertical facial excess ( Fig. 15-3 ).

When evaluating the gingival display at smile, another differential diagnosis of vertical maxillary excess is altered passive eruption. In this situation the crowns of the incisors appear to be short in height because of inadequate apical migration of the dentogingival complex, resulting in more apparent gingival tissue on smiling. Again, the clinical analysis of the smile must be correlated with the cephalometric and anthropometric data to obtain a complete diagnosis.
TREATMENT STRATEGIES
After reviewing all the multiple etiologies for the hyperdivergent facial profile, treatment strategies need to include soft tissue, dental, and skeletal evaluations. The vertical dimension can readily be altered by controlling the posterior teeth. In these patients the ultimate goal is either to intrude or to maintain the vertical position of the molars.
The methods available to achieve the vertical control of the molars vary depending on the age of the patient. The specific aim of treatment in the growing patient is to hold the vertical position of the molars while normal vertical maxillary and mandibular growth is occurring. Generally, the different orthodontic appliances for the vertical control are targeted to the maxillary molars, although vertical control of the mandibular molars has also been described.
Appliances
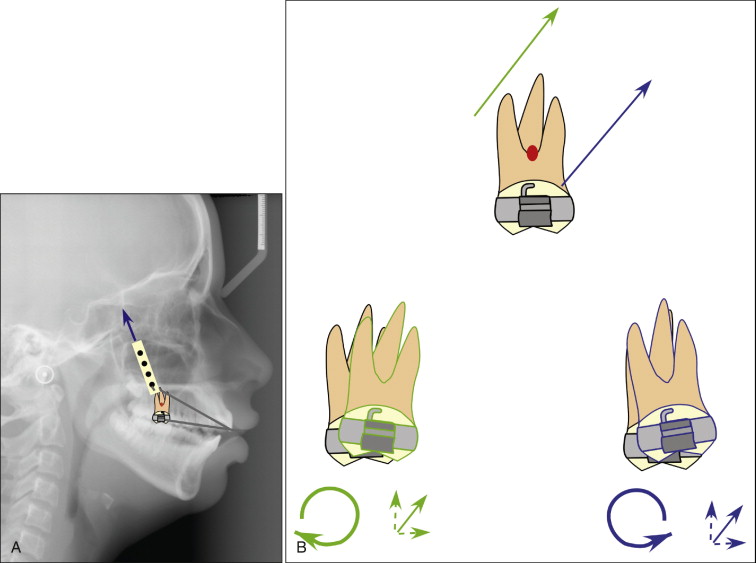
Different appliances have been used to restrict the vertical maxillary growth and inferior displacement of the molars. These appliances apply the force directly or indirectly to the first molars. Headgear is the classic example of an appliance that delivers a force directly to the molar in an intrusive direction. Occipital and vertical-pull headgears have been recommended because both types have a vertical component to the force. Although the occipital type does not provide a purely vertical force, the distally directed component of the force may be indicated in patients with vertical maxillary excess and a convex profile. To deliver this type of force vector, the pulling force of the headgear should approximate the center of resistance of the maxillary molar. This is obtained by adjusting the height and the length of the outer bow. Key ridge serves as an anatomical landmark to estimate the center of resistance of the maxillary molar. Any vector of the force that does not go through the center of resistance of the molar will generate a clockwise or counterclockwise rotation of the molar ( Fig. 15-4 ). This tipping movement of the molar can be used favorably in certain sagittal occlusal relationships (i.e., Class II molar).
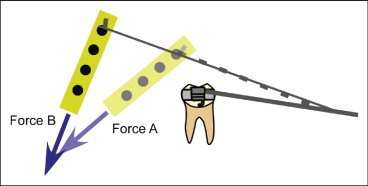
Another appliance that aids in controlling the vertical dimension has been proposed by Pearson and involves the application of mandibular headgear. This design controls the eruption of the lower molar, especially when using Class II elastics. By inhibiting the lower molar eruption, the vertical dimension is, in theory, more readily controlled. Reportedly, lower alveolar height increases more than the maxillary molar height during orthodontic treatment, in which case mandibular headgear becomes particularly attractive. The only disadvantage of this appliance is that a purely vertical force cannot be delivered; a distal component of the force is always present. This distal component of the force can be decreased by lengthening the outer bow ( Fig. 15-5 ). However, this adjustment would also tend to increase the distal tipping effect on the molar because of the moment of the force. Mandibular headgear could certainly be a treatment option for vertical control, but it is not a popular modality.
Indirect Delivery of Force
The maxillary and mandibular molars can also be controlled vertically in the growing patient though indirect delivery of the force. This can be accomplished through the different muscles during normal function. The two primary muscle groups involved in these indirect forms of force delivery are the masticatory muscles and the muscles of the tongue.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


