http://evolve.elsevier.com/Haveles/pharmacology
Diseases of the respiratory tract are common, so dental hygienists are sure to encounter patients taking drugs for these diseases (Figure 19-1). Because the medications given to treat these diseases can affect dental treatment, the dental hygienist should be aware of the effects of these drugs on the patient and how these drugs can alter the dental treatment plan.
Diseases that are treated with respiratory drugs include asthma, chronic obstructive pulmonary disease (COPD), and upper respiratory tract infections (Figure 19-2). Respiratory drugs come from a wide range of drug groups, from adrenergic drugs for bronchodilation to corticosteroids for reducing inflammation. Drugs that increase expectoration and reduce coughs are also included in this discussion. Many drugs used to treat respiratory problems are administered topically via the lungs by the use of a metered-dose inhaler (MDI).
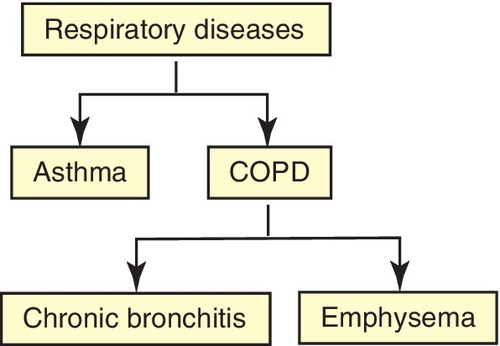
Respiratory diseases
Noninfectious respiratory diseases are divided into two groups: (1) asthma and (2) COPD (see Figure 19-2). COPD is further divided into chronic bronchitis and emphysema. Other respiratory problems are related to respiratory infections, principally viral or bacterial.
Asthma
One common respiratory disease is asthma. It is characterized by reversible airway obstruction and is associated with reduction in expiratory airflow. A few hours later, inflammation occurs, resulting in an increase in secretions in the lungs and swelling in the bronchioles. Asthma is classified as being either intermittent or persistent. Persistent asthma is further categorized as mild, moderate, or severe. Patients with intermittent asthma experience symptoms less than two times a month and the symptoms do not interfere with normal activity. Persistent asthma occurs anywhere from more than twice a week to all day long. Persistent asthma can cause minor limitation of normal activities, and severe persistent asthma can severely limit the patient’s normal activities. When asthma is treated, both components of the disease must be addressed. The National Asthma Education and Prevention Program Expert Panel Report 3, published in October 2007, presents the latest recommendations of the National Heart Lung and Blood Institute regarding asthma therapy. Table 19-1 reviews the stepwise approach for managing asthma in children older than 12 years and adults.
Table 19-1
Treatment of Asthma
ICS, inhaled corticosteroid; LM, leukotriene modifier; LABA, long-acting β2-agonist; SABA, short-acting β2-agonist.
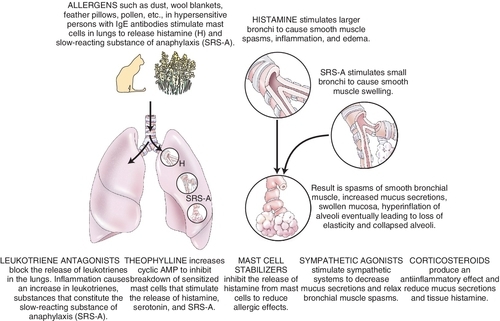
Asthma may be precipitated by allergens, pollution, exercise, stress, or upper respiratory infection (allergic reaction to viruses). The patient with status asthmaticus has persistent life-threatening bronchospasm despite drug therapy. Environmental pollution may also play an important role in the increase in asthma. The dental hygienist should manage dental patients with asthma so as to induce minimal stress. Patients should bring their fast-acting β2-agonist inhalers to be used prophylactically or in the management of an acute asthmatic attack in the dental office. Signs of asthma include shortness of breath and wheezing. By observing and asking the patient about asthma control before the dental appointment, the dental hygienist can prevent an acute attack. β2-adrenergic agonists, xanthines, cromolyn, corticosteroids, leukotriene (LT) altering agents, and anticholinergics are used to treat this disease (Figure 19-3).
Chronic Obstructive Pulmonary Disease
COPD is characterized by irreversible airway obstruction, which occurs with either chronic bronchitis or emphysema. Smoking is associated with almost all cases of COPD. Chronic bronchitis is a result of chronic inflammation of the airways and excessive sputum production. Emphysema is characterized by alveolar destruction with air space enlargement and airway collapse. Tables 19-2 and 19-3 review the recommended treatment regimens for COPD. The anticholinergics are the first-line agents, but β2-adrenergic agonists are also used to produce bronchodilation in patients with this disease. In many instances patients receive a combination metered-dose inhaler containing an anticholinergic drug and a β2 agonist. COPD is associated with an increase in the incidence of bronchospasm and with fixed airway obstruction. Patients with upper respiratory tract infections also often take β2 adrenergic agonists for bronchoconstriction, antihistamines to reduce secretions, expectorants to thin sputum, and antitussives to control coughing. Each drug group is discussed separately in the section on respiratory infections.
Table 19-2
FDA-Approved Drugs Used to Manage Asthma
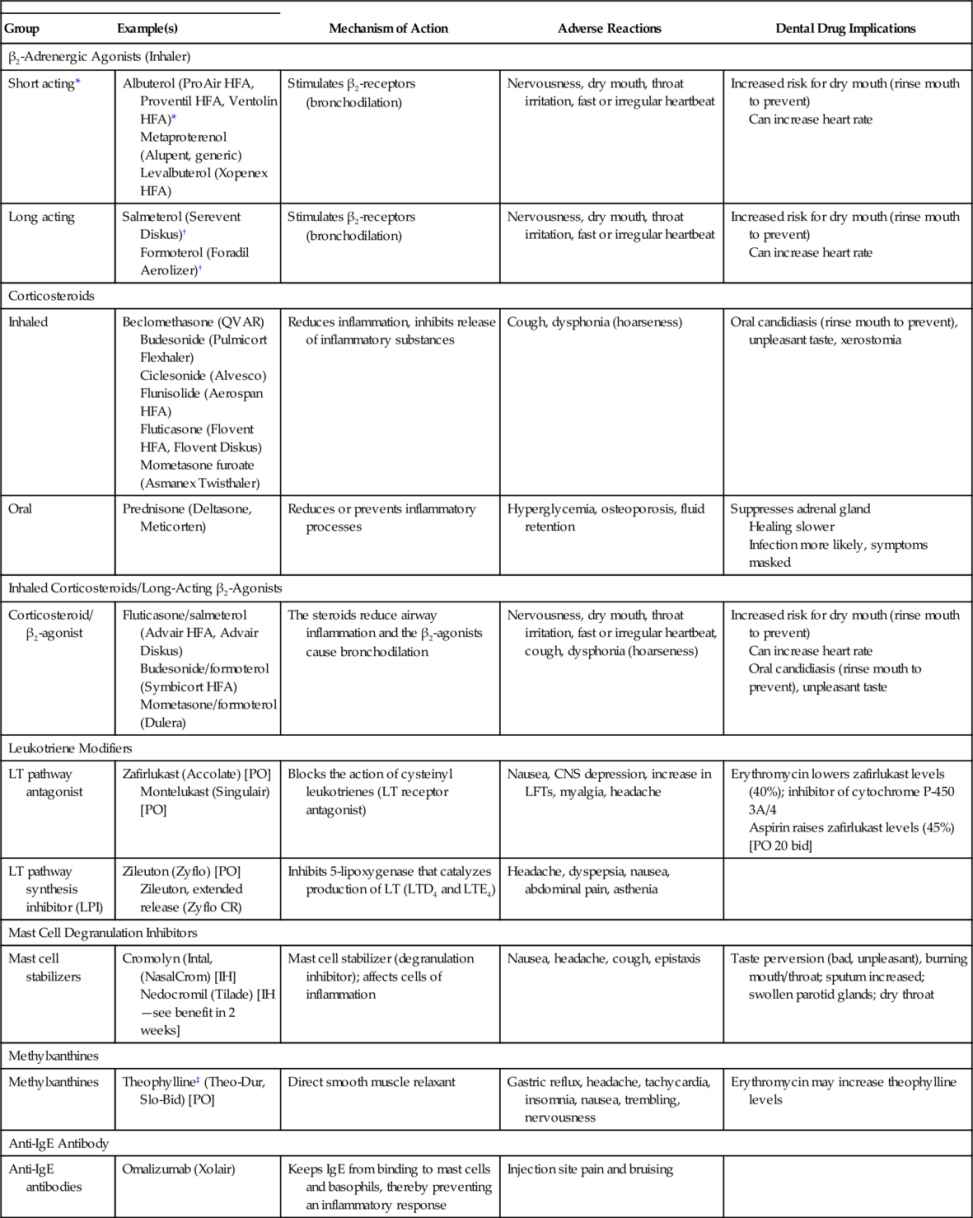
bid, twice a day; BP, blood pressure; CNS, central nervous system; IH, inhalation; IgE, immunoglobulin E; LFTs, liver function tests; LT, leukotriene; PO, by mouth.
* Use for an acute attack.
† Do not use in an emergency, delayed onset (> 1 hr), prolonged effect (12 hr).
‡ Relative of caffeine found in coffee and cola beverages.
Table 19-3
Treatment of Chronic Obstructive Pulmonary Disease
ICS, inhaled corticosteroid; LABA, long-acting β2-agonist; PDE4, phosphodiesterase-4; SABA, short-acting β2-agonist.
In the normal person, the drive for ventilation (breathing) is stimulated by an elevation in the partial pressure of carbon dioxide (Paco2). The partial pressure of oxygen (Pao2) can vary widely without stimulating ventilation in the normal patient. Patients with COPD, because their ventilation is compromised, experience a gradual rise in Paco2 over time. Because this mechanism becomes resistant to changes in Paco2, a new stimulus emerges, the partial pressure of Pao2. The patient’s ventilation is then driven by a decrease in Pao2. If a patient with COPD is given oxygen and the Pao2 rises, the stimulant to breathing is removed, and apnea may be induced. For patients with severe COPD, it is suggested that the rate of oxygen administration be limited to less than 3 L/min. Other literature recommends that in the patient with severe COPD, oxygen by nasal cannula be used during a dental appointment, especially if pain or stress is expected (increased oxygen demand).
Drugs used to treat respiratory diseases
Metered-Dose Inhalers
The MDI, developed in the 1950s, provides a useful method to administer certain medications to the respiratory tree (Figure 19-4). It is the preferred route of delivery for most asthma drugs. Its advantages include the following:

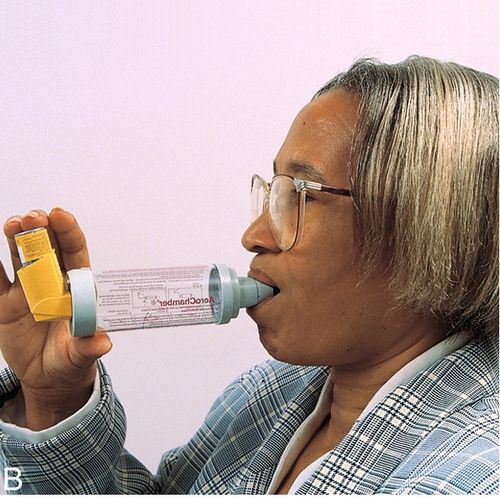
Disadvantages of MDIs are that they are difficult to use properly (particularly for children) and they can be abused, with a resultant decrease in response. Additional patient education is required to get the most from this dose form. Often, a “spacer” is placed between the MDI and the mouth to increase the amount of drug delivered to the lungs (see Figure 19-4B). Medications currently available in MDIs include β-agonists, both specific and nonspecific; corticosteroids; cromolyn; and anticholinergic drugs.
Chlorofluorocarbons (CFCs), which have ozone-depleting properties, have been phased out as propellants in MDIs. Nonchlorinated hydrofluoroalkane (HFA) propellants, which do not deplete the ozone layer, have replaced CFCs.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


