http://evolve.elsevier.com/Haveles/pharmacology
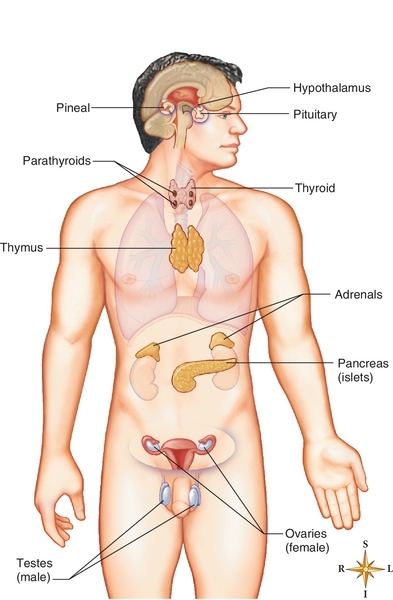
Hormones are secreted by endocrine glands and transported by the blood to target organs, where they are biologically active. Endocrine glands include the pituitary, thyroid, parathyroids, pancreas, adrenals, gonads, and placenta (Figure 22-1). They help maintain homeostasis by regulating body functions and are controlled themselves by feedback systems. In most of these systems, the hormone released has a negative feedback effect on the secretion of the hormone-stimulating substance. Patients being treated in the dental office may be taking these hormones to treat various diseases.
Drugs that affect the endocrine system include the hormones secreted by the endocrine glands, synthetic hormone agonists and antagonists, and substances that influence the synthesis and secretion of hormones. The most important clinical application of these drugs is their use in replacement therapy, such as in the treatment of diabetes mellitus (DM) (insulin) (see Chapter 21) and hypothyroidism (levothyroxine). Additional applications include diagnostic procedures, contraception, and the treatment of glandular hyperfunction, cancer, and other systemic disorders.
Pituitary hormones
The pituitary gland (hypophysis) is a small endocrine organ located at the base of the brain. It has been called the master gland because of its regulatory effect on other endocrine glands and organs of the body. It secretes peptide hormones that regulate the thyroid, adrenal, and sex glands; the kidney and uterus; and growth.
In addition to their regulatory effect, the pituitary hormones have a trophic effect that is necessary for the maintenance of many systems. For example, without the gonadotropins, the entire reproductive system fails; without growth hormone and thyrotropin, normal growth and development are impossible.
The secretion of pituitary hormones is influenced by peripheral endocrine glands via hormonal feedback mechanisms and by neurohumoral substances from the hypothalamus. When the hypothalamus releases specific hormone-releasing substances, the specific pituitary hormone is released.
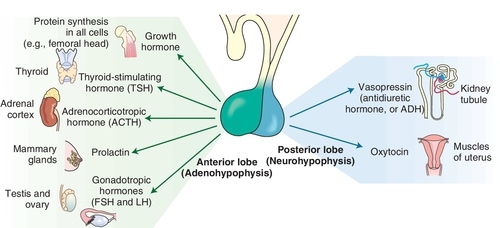
Pituitary deficiency (hypopituitarism) can produce a loss of secondary sex characteristics, decreased metabolism, dwarfism, diabetes insipidus, hypothyroidism, Addison’s disease, loss of pigmentation, thinning and softening of the skin, decreased libido, and retarded dental development. Hypersecretion of pituitary hormones can produce sexual precocity, goiter, Cushing’s disease, acromegaly, and giantism. There are two parts to the pituitary gland: the anterior lobe (adenohypophysis) and the posterior lobe (neurohypophysis).
Anterior Pituitary
The anterior lobe of the pituitary gland secretes growth hormone, or somatotropin; luteinizing hormone (LH); follicle-stimulating hormone (FSH); thyroid-stimulating hormone (TSH), or thyrotropin; adrenocorticotropic hormone (ACTH), or corticotropin; and prolactin (Figure 22-2). β-Lipotropin, secreted by the pituitary, is a precursor to β-endorphin (see Chapter 6).
Genetic engineering has been able to produce human growth hormone since 1987. Human growth hormone is used medically to treat children who lack it and illicitly by body builders and weight lifters to develop muscles. (Some say that in athletic events at which the contestant’s urine is tested, for example, the Olympics, growth hormone cannot be detected as easily as the androgenic steroids.)
Pharmaceutical gonadotropin-releasing hormone (GnRH) is a synthetic analog. One example, leuprolide, stimulates the pituitary function and is used to treat infertility. GnRH agonists are used to treat prostate cancer and endometriosis. The secretions from the anterior pituitary that stimulate other glands are used to test the function of the stimulated glands.
FSH-like products, which stimulate follicle growth, and LH-like products, which induce ovulation, are used in the treatment of infertility. Although LH itself is not available, human chorionic gonadotropin (hCG), which is almost identical in structure, can be used as an LH substitute for deficiency. Human menopausal gonadotropin (hMG) contains FSH and LH and is commercially available as menotropin (Pergonal). This preparation is used in infertility to stimulate development of ovarian follicles. When follicular maturation has occurred, the hMG is discontinued and hCG is given to induce ovulation.
Bromocriptine
Bromocriptine (broe-moe-KRIP-teen) (Parlodel), an ergot derivative, inhibits pituitary function. Although not a hormone, it is a dopamine agonist that suppresses prolactin levels. Bromocriptine is used to treat prolactin-secreting adenomas (hyperprolactinemia), acromegaly, and Parkinson’s disease.
Posterior Pituitary
The posterior pituitary gland secretes two hormones: vasopressin (antidiuretic hormone [ADH]) and oxytocin. Vasopressin (vay-soe-PRES-in) (Pitressin) has vasopressor and antidiuretic hormone activity and is used for treatment of transient diabetes insipidus. Synthetic analogs of vasopressin (desmopressin [DDAVP, Stimate] and lypressin [Diapid]) are used for long-term treatment of pituitary diabetes insipidus and to treat certain clotting disorders (hemophilia A and von Willebrand’s disease). Available as nasal solutions, these two analogs have the same action as vasopressin but are longer acting.
Oxytocin (oks-i-TOE-sin) (Pitocin, Syntocinon), administered either by injection or intranasally, is used to induce labor, control postpartum hemorrhage, and induce postpartum lactation.
Thyroid hormones
The thyroid gland secretes two iodine-containing thyroid hormones: triiodothyronine (T3) and tetraiodothyronine (T4, thyroxine). Calcitonin, another hormone secreted by the thyroid, regulates calcium metabolism. Thyroid hormones act on virtually every tissue and organ system of the body and are important for energy metabolism, growth, and development. Vulnerability to stress, altered drug response, and altered orofacial development are all possible manifestations of thyroid dysfunction. The head and neck examination performed by dental practitioners can identify some thyroid abnormalities. Swallowing can accentuate the thyroid to allow palpitation. The consistency of the gland varies with the abnormality.
Thyroid hormones are synthesized from iodine and tyrosine and stored as a complex protein until TSH stimulates their release. The actions of the thyroid hormones include those on growth and development, calorigenic effects, and metabolic effects. In frogs, thyroid hormone can transform a tadpole into a frog.
Iodine
Normal function of the thyroid gland requires an adequate intake of iodine (approximately 50-125 mg per day). Without it, normal amounts of thyroid hormones cannot be made, TSH is secreted in excess, and the thyroid hypertrophies. This thyroid hypertrophy is called simple goiter or nontoxic goiter. Because iodine is not abundant in most foods, simple goiter is prevalent in some areas of the world. Marine life is the only common food that is naturally rich in iodine. Use of iodized salt (contains potassium iodide [KI]) has decreased the incidence of simple goiter in many countries. Iodine is currently used in conjunction with an antithyroid drug in hyperthyroid patients being prepared for surgery.
Iodide in high concentrations suppresses the thyroid in a still poorly understood manner. It may produce gingival pain, excessive salivation, and sialadenitis as side effects.
Hypothyroidism
In the small child, hypofunction of the thyroid is referred to as cretinism. In the adult, this condition is called myxedema or simple hypothyroidism. The main characteristics are mental and physical retardation. Such patients are usually drowsy, weak, and listless and exhibit an expressionless, puffy face with edematous tongue and lips. Oral findings in children usually include delayed tooth eruption, malocclusion, and increased tendency to development of periodontal disease. The teeth are usually poorly shaped and carious. The gingiva is either inflamed or pale and enlarged. The cretinous child is often uncooperative and difficult to motivate for plaque control. Diagnostic radiographs and routine dental prophylaxis in these patients may require special assistance.
Hypothyroid patients have difficulties withstanding stress and tend to be abnormally sensitive to all central nervous system (CNS) depressants, including the opioids and sedatives. If opioid analgesics are used, their doses should be reduced. Hypothyroid pregnant women tend to produce offspring with large teeth.
Thyroid hypofunction is rationally and effectively treated by oral administration of exogenous thyroid hormones. The most common thyroid hormone used for replacement therapy is levothyroxine (lee-voe-thye-ROX-een). Box 22-1 lists preparations used for thyroid hormone replacement therapy.
Hyperthyroidism
Diffuse toxic goiter (Graves’ disease) and toxic nodular goiter (Plummer’s disease) are the two forms of thyroid hyperfunction. Diffuse toxic goiter is characterized by a diffusely enlarged, highly vascular thyroid gland. It is common in young adults and is considered a disorder of the immune response. Toxic nodular goiter is characterized by nodules within the gland that spontaneously secrete excessive amounts of hormone while the rest of the glandular tissue is atrophied. It occurs primarily in older patients and usually arises from long-standing nontoxic goiter.
Hashimoto’s disease, a chronic inflammation of the thyroid associated with an autoimmune response, causes hyperthyroidism. Antithyroglobulin antibody can be detected. It occurs in middle-aged women, often concomitantly with other autoimmune diseases.
Excessive levels of circulating thyroid hormone produce thyrotoxicosis. The adverse effects include excessive production of heat, increases in sympathetic activity, neuromuscular activity, and sensitivity to pain, ophthalmopathy, exophthalmos (protruding eyes), and anxiety. Oral manifestations are accelerated tooth eruption, marked loss of the alveolar process, diffuse demineralization of the jawbone, and rapidly progressing periodontal destruction.
The cardiovascular system is especially hyperactive because of a direct inotropic effect, increased peripheral oxygen consumption, and greater sensitivity to catecholamines. Epinephrine is relatively contraindicated in patients with hyperthyroidism. The potentiating effects of excess thyroid hormone and epinephrine on each other could result in cardiovascular problems such as angina, arrhythmias, and hypertension. β-Blockers, such as propranolol, are used to counteract the tachycardia.
In addition to their greater sensitivity to pain, hyperthyroid persons have an increased tolerance to CNS depressants. They may require higher than usual doses of sedatives, analgesics, and local anesthetics.
No treatment should be begun to any patient with a visible goiter, exophthalmos, or a history of taking antithyroid drugs until approval is obtained from the patient’s physician. Medical management of the condition is important before any elective surgery is performed. A surgical procedure or an acute oral infection could precipitate a hyperthyroid crisis known as thyroid storm. Hydrocortisone should be administered intravenously, and cold towels should be placed on the patient. The use of epinephrine should be avoided in poorly treated or untreated thyrotoxic patients. The cardiac dose of epinephrine can be used carefully. Even in patients with controlled hyperthyroid disease who are considered to be euthyroid, stress should be kept at a minimum, preoperative sedation should be considered, and the dental team should be alert for signs of hypothyroidism or hyperthyroidism.
Treatment of hyperthyroidism usually includes one of the options highlighted in Box 22-2. The two most common treatments are radioactive iodine (131I) and thyroidectomy. 131I is usually the drug of choice for patients older than 21 years. It is taken internally and sequestered by the gland; localized destruction of thyroid tissue results. Thyroidectomy is the surgical approach to hyperthyroidism. Both radioactive iodine and thyroidectomy usually result in hypothyroidism because a dose that produces an inadequate effect would require repeating the procedure. If a patient has been adequately treated for hyperthyroidism with either radioactive iodine or thyroidectomy and is taking supplemental thyroid (as needed [prn]), then that patient may be treated like a euthyroid patient.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


