http://evolve.elsevier.com/Haveles/pharmacology
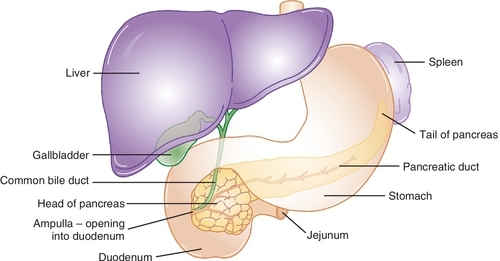
Hormones are secreted by endocrine glands and transported by the blood to target organs, where they are biologically activated. The endocrine gland discussed in this chapter is the pancreas (Figure 21-1). The hormones released by the endocrine glands help maintain homeostasis by regulating body functions and are controlled themselves by feedback systems. In most of these systems, the hormone released has a negative feedback effect on the secretion of the hormone stimulating substance. Patients with diabetes mellitus (DM) being treated in the dental office may be taking medication to help lower their plasma glucose levels.
Pancreatic hormones
Two primary hormones secreted by the islets of Langerhans of the pancreas are insulin and glucagon. Insulin promotes fuel storage (pack the bags: glucose out of blood), whereas glucagon promotes fuel mobilization (empty the bags: glucose into blood) in the body. Other hormones secreted by the pancreas are islet amyloid polypeptide (IAPP; amylin) and pancreatic peptide. Their functions have not yet been elucidated.
Diabetes mellitus
Diabetes mellitus (DM) is a group of metabolic disorders characterized by persistent hyperglycemia. DM is currently classified as types I and II (Table 21-1).
Table 21-1
Diabetes Types 1 and 2
| Property | Type 1 | Type 2 |
| Age of onset | < 30 years | > 40 years |
| Onset of symptoms | Acute | Gradual |
| Incidence of cases | 10% | 90% |
| Etiology | Autoimmune reaction | Insulin resistance, excess hepatic glucose production, diminished insulin secretion |
| Genetic influence | Just a little | Quite a bit |
| Receptors | Normal | Defective |
| Plasma insulin | No | Normal or elevated then over time reduced |
| Ketoacidosis | Yes | No |
Nearly 26 million people in the United States have diabetes. The vast majority of these people, 90-95%, are diagnosed with type 2 diabetes. Both environmental and genetic factors are believed to contribute to the pathogenesis of type 2 diabetes. It is thought that the hyperglycemia leads to the many complications of diabetes.
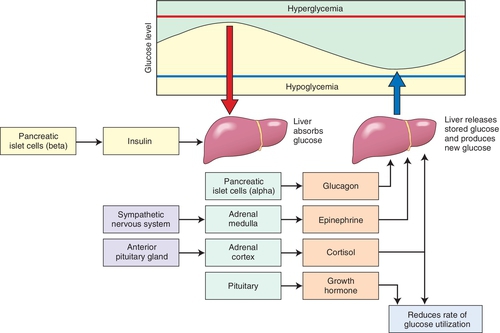
Symptoms and complications result, usually from inadequate or poorly timed secretion of insulin from the pancreas and/or insulin resistance of the pancreatic islet cells (β cells). (Figure 21-2 outlines the body’s physiologic response to changes in plasma glucose levels.) The criterion for the diagnosis of DM is (1) two consecutive fasting plasma glucose levels or the more commonly used term of fasting blood sugars (FBSs) higher than 126 mg/dl or (2) a hemoglobin A1c value of 6.5% or higher or (3) a 2-hour plasma glucose level of 200 mg/dl or higher during an oral glucose tolerance test or (4) a randomly measured plasma glucose level of 200 mg/dl or higher in a patient with the classic symptoms of hyperglycemia or hyperglycemic crisis.
Diabetes is primarily characterized by hyperglycemia and glycosuria. Other characteristics include hyperlipemia; azoturia; ketonemia; and, when the deficiency is severe, ketoacidosis. Patients usually experience general weakness, weight loss, polyphagia, polydipsia, and polyuria. Patients with type 2 diabetes often experience weight gain.
Types of Diabetes
Type 1
Type 1 diabetes usually develops in persons younger than 30 years and results from an autoimmune destruction of the pancreatic β cells. The type 1 autoimmune response may be triggered by an infection, a slow virus, environmental insults, or some as yet unknown factor. It is associated with a complete lack of insulin secretion, increased glucagon secretion, rapid onset of disease, ketosis, and severe symptoms. Type 1 diabetes must be treated with injections of insulin because the pancreas does not produce any insulin. Without insulin, type 1 DM is fatal.
Type 2
Type 2 diabetes usually develops in persons older than 40 years. However, more and more cases of type 2 diabetes are being reported in persons younger than 20 years. This development is being attributed to a much more sedentary lifestyle and lack of exercise in the U.S. population. Fast food has replaced traditional home-cooked food, and video games and television have replaced physical activity; as a result, obesity is dramatically on the rise. Obesity is a major risk factor for development of type 2 diabetes. This disease is associated with the ability of the pancreas to secrete enough insulin to prevent ketoacidosis but not enough to normalize the plasma glucose level. The insulin secreted does not reduce the glucose levels in the serum to normal levels, for a variety of possible reasons (Box 21-1).
Insulin resistance develops because of prolonged hyperglycemia and resulting hyperinsulinemia. Type 2 diabetes involves a slower onset of disease, less severe symptoms, and lack of ketoacidosis. Tissue insensitivity to insulin, a deficiency of the pancreas’s response to glucose, and obesity lead to impaired insulin action. In the presence of hyperglycemia, the resistance of the tissues to insulin and the impaired β cells’ response are exaggerated. Normal serum glucose levels improve these parameters toward normal.
Type 2 diabetes is treated first with diet and exercise, then with orally acting agents, and, if these modalities fail, with insulin. Therefore patients with type 2 diabetes may be taking insulin either with or without oral agents. Because of the etiology of the hyperglycemia in patients with type 2 diabetes, moderate improvement of diet and/or an increase in exercise can produce a large improvement in the glucose levels. Exercise increases the sensitivity of the cells to insulin. Unfortunately, these behavior modifications are difficult to carry out on a routine basis for almost all patients.
Dental Implications of Diabetes
Uncontrolled diabetes causes a pronounced susceptibility to dental caries. This is mainly occurs through decreased salivary flow (xerostomia) related to fluid loss. The loss is secondary to an increase in urination that occurs because of poor use of carbohydrates and the glucose that is excreted via the kidneys (water follows glucose). The complications of xerostomia are a result of the lack of its normal functions: lubricating, cleansing, regulating pH, destroying microorganisms and their products, and maintaining the integrity of the oral structures.
A dry, cracking oral mucosa with the presence of mucositis, ulcers, infections, and an inflamed painful tongue may result. Any change in the glucose level in saliva probably contributes little to the higher caries rate.
Xerostomia
Patients with diabetes mellitus are at a higher risk for xerostomia, especially as they age. A decrease in salivary flow can lead to mouth ulcers, inflammation of the tongue or mucosal tissues, and tooth deterioration. Diabetes causes blood vessels to thicken, thereby slowing down blood flow to the teeth and gums. As a result, teeth and gums become less healthy and less resistant to oral bacteria in dental plaque.
Periodontal Disease
Patients with uncontrolled or undiagnosed diabetes are more prone to periodontal disease. However, the periodontal status of the patient with well-controlled diabetes has been somewhat more controversial. Despite the fact that some investigators have reported a lack of correlation between diabetes and an increase in rate of periodontal disease, many other studies have come to the opposite conclusion. (It may be that if diabetes control is good, there is hardly any effect on periodontal status, whereas if diabetes control is poor, there is a greater effect.)
Periodontal findings include inflammatory and degenerative changes ranging from mild gingivitis to painful periodontitis with a widened periodontal ligament, multiple abscesses, putrescent exudates from periodontal pockets, and increased tooth mobility caused by destruction of supporting alveolar bone. Although it may be more severe, periodontal disease in diabetic patients appears to be similar to that found in nondiabetic patients. The diabetic state probably serves as a predisposing factor that can accelerate the periodontal destruction originated by microbial agents. The proposed etiology for the periodontal changes seen in the patient with diabetes includes microangiopathy of the tissues, thickening of capillary basement membranes, changes in glucose tolerance factor (more glucose), altered polymorphonuclear leukocyte function, and enhanced collagenase activity.
Issues in Dental Care
Dental appointments for diabetic patients should not interfere with meals and should involve minimal stress. In the patient with controlled diabetes, oral surgical procedures should be performed 1.5-2 hours after the patient has eaten normal breakfast and taken regular antidiabetic medication. Following surgery, the patient should receive an adequate caloric intake to prevent hypoglycemia. With general anesthesia, patients are often instructed to have nothing by mouth (NPO), should take half of their usual dose of insulin, and receive intravenous 5% glucose in distilled water (D5W).
Patients with diabetes have fragile blood vessels, delayed wound healing, and a tendency to development of infections; therefore surgical therapy in such patients should be approached with caution. Scaling and soft tissue curettage usually are tolerated well. The bulk of the literature suggests that prophylactic use of antibiotics should be avoided, although many practitioners routinely use antibiotics. If infection is present or if infection ensues, it should be aggressively treated. Measures to reduce the possibility of infection should be used (sterilize instruments, rinse mouth before procedures). The oral complications of diabetes are summarized in Table 21-2.
Table 21-2
Oral Complications of Diabetes Mellitus*
* All complications worsen with hyperglycemia, either acute or chronic. An acute fasting glucose (mg/dl) measurement with a glucose monitor are reflective of glucose at that moment, and long-term glucose levels measured by HgA1c concentration are reflective of glucose control over the previous 2 to 3 months. Oral complications of hyperglycemia are xerostomia, infection, poor healing, increased caries, candidiasis, gingivitis, periodontal diseases, periapical abscess, and burning mouth syndrome.
Cautions and Contraindications
Drugs that may decrease insulin release or increase insulin requirements, such as epinephrine, glucocorticoids, and opioid analgesics, should be used with caution in patients with diabetes. Caution should also be exercised with use of general anesthetics because of the possibility of acidosis. If diabetes is in good control, these drugs can be used.
Systemic Complications of Diabetes
The systemic complications of diabetes include actions affecting almost all the body tissues and organs.
Cardiovascular Complications
The incidence of cardiovascular problems is higher in patients with diabetes. Macroangiopathy, microangiopathy, and hyperlipidemia are common. Atherosclerosis is also more common in these patients.
Retinopathy
Because microvascular disease affects the blood supply to the retina, the functioning of the retina is impaired. In fact, diabetes is the major cause of blindness in adults.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


