Introduction
The purpose of this study was to investigate the long-term stability of deep overbite correction with mandibular incisor intrusion with utility arches in adult patients.
Methods
Pretreatment, posttreatment, and 5-years postretention lateral cephalograms of 31 patients (mean age, 26.8 years; range, 24.1-30.9 years) with Class II Division 1 malocclusion and deepbite, treated by maxillary first premolar extraction and mandibular incisor intrusion, were traced and measured.
Results
Significant decreases in overjet and overbite (6.4 ± 1.2 and 3.9 ± 0.7 mm, respectively), significant retroclination (17° ± 1.9°) and retraction (3.8 ± 1.1 mm) of the maxillary incisors, and significant increases in protrusion (0.8 ± 1.5 mm), proclination (0.6° ± 0.9°), and intrusion (2.6 ± 1.4 mm) of the mandibular incisors were observed at posttreatment. At postretention, there were statistically significant but clinically unimportant increases in overjet and overbite (0.4 ± 0.2 and 0.8 ± 0.4 mm, respectively) and extrusion of the mandibular incisors (0.8 ± 1.1 mm).
Conclusions
Correction of deepbite in nongrowing patients by mandibular incisor intrusion with a utility arch can be considered effective and stable.
Correction of deepbite is often a challenging step in orthodontic treatment. Untreated deepbite can cause increased anterior crowding, maxillary dental flaring, periodontal problems, and temporomandibular joint problems and can interfere with lateral and anterior mandibular movements.
Deepbite can be treated orthodontically by intrusion or flaring of the incisors, extrusion or passive eruption of the buccal segments, or a combination of these. The choice of treatment depends on several factors. Extrusion of the posterior dentition, although an effective method of bite opening in growing patients, is not indicated in patients with normal incisor display or normal or long lower facial height; its stability is questionable in nongrowing patients with average to low mandibular plane angles. Intrusion of the maxillary incisors is indicated in patients with excessive incisor and gingival display and a large interlabial gap. Considering these facts, mandibular incisor intrusion is the most suitable deepbite treatment for adults with normal incisor and gingival display and a normal or high mandibular plane angle.
Although many studies have examined the stability of deepbite treatment, most included growing subjects. In some studies, different malocclusions or different treatment methods were assessed together, and in others the follow-up durations were short. Two studies of nongrowing subjects did not include information about long-term follow-up results and treatment stability.
The purpose of this study was to investigate the long-term stability of deepbite correction with mandibular incisor intrusion with utility arches in adult patients. The null hypothesis was that dental deepbite correction with mandibular incisor intrusion in adults is stable.
Material and methods
In this retrospective longitudinal study, pretreatment (T1), posttreatment (T2), and postretention (T3) lateral cephalograms of 31 patients (24 women, 7 men) with Class II Division 1 malocclusion treated with a 1-phase maxillary first premolar extraction protocol by either of the first 2 authors were used. Their mean age at the beginning of treatment was 26.8 years (range, 24.1-30.9 years). The inclusion criteria were (1) standardized lateral cephalograms available at 3 time periods, T1, T2, and T3; (2) deepbite of at least 4.5 mm; (3) normal vertical dimension represented by lower face height of 47° ± 3°; (4) 3 to 4 mm or less of maxillary incisor display at rest; (5) overjet of at least 6 mm; and (6) 4 mm or less crowding in the maxillary and mandibular arches.
Because of the retrospective nature of the study and because no additional x-rays were taken, ethical approval was not needed; informed consent had been obtained at T1 from all patients as the routine protocol.
The treatment protocol included intrusion of the mandibular incisors to correct the deepbite and extraction of the maxillary first premolars to correct the overjet. All patients had transpalatal arches on the maxillary first molars before the extractions. All patients had 0.018-in slot preadjusted metal brackets with the Roth prescription. In the maxillary arch, after alignment, the canines were retracted with nickel-titanium coil springs (Sentalloy; GAC International, Central Islip, NY) exerting 150 g of force on 0.016 × 0.022-in stainless steel archwires (Accuform; GAC International). The incisors were retracted by 0.017 × 0.025-in beta-titanium alloy archwires (Resolve; GAC International) with mushroom loops.
The mandibular incisors and premolars were leveled by 0.016-in nickel-titanium segments if necessary. After leveling, custom-made mandibular utility arches (0.016 × 0.022-in Blue Elgiloy wires; Ormco, Glendora, Calif), activated to exert 40 g of force, were used for incisor intrusion. During this period, 0.016 × 0.022-in stainless steel stabilizing sections extending from the first molars to the first premolars were placed. The intrusive force of 40 g was checked before tying the archwire, and the force levels were checked every 4 weeks. Intrusion was considered complete when a 2-mm overbite was achieved, and a 0.016 × 0.022-in Blue Elgiloy stabilization utility arch was placed. At this point, the mandibular canines were tied to the stabilizing utility arch with elastic thread if their intrusion was necessary; 0.017 × 0.025-in stainless steel wires were used for finishing in both arches. The mean active treatment time was 2.7 years (range, 2.4-3 years). Immediately after debonding, maxillary and mandibular wraparound retainers were delivered. The patients were instructed to wear the retainers 24 hours a day for the first year and only at night after that. The retention period lasted 1.5 years.
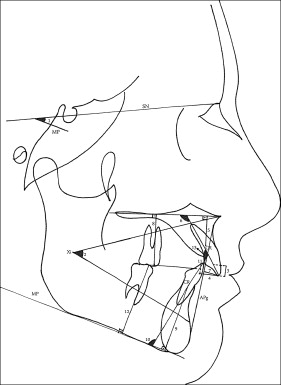
The same author (S.K.V.) hand-traced the lateral cephalograms and identified all landmarks. All hand-tracings were scanned with a scanner at 200 dpi, and Dolphin software (version 10; Dolphin Imaging & Management Solutions, Chatsworth, Calif) was used to obtain the cephalometric measurements. The measurements are shown in the Figure and Table I . The center of resistance (a point located at one-third of the distance of the root length apical to the alveolar crest) was used to evaluate the vertical positions of both the mandibular and maxillary central incisors.
| SN to MP (°) | Angle formed by the sella-nasion line and mandibular plane ∗ (MP) |
| ANS to Xi/Xi-PM (°) | Angle formed by the line extending from anterior nasal spine to Xi † and corpus axis (Xi-PM ‡ ) |
| Overbite (mm) | Distance between incisal edges of maxillary and mandibular central incisors, perpendicular to occlusal plane § (OP) |
| Overjet (mm) | Distance between incisal edges of maxillary and mandibular central incisors, parallel to OP |
| U1CR to PP (mm) | Perpendicular distance between the center of resistance ‖ (CR) of maxillary central incisor and palatal plane (PP) |
| U1 to PP (°) | Angle formed by the long axis of maxillary central incisor and palatal plane |
| U1 to APg (mm) | Perpendicular distance from maxillary incisor incisal edge to A-point–pogonion line |
| U6 to PP (mm) | Perpendicular distance from the mesiobuccal cusp tip of maxillary first molar to PP |
| L1CR to MP (mm) | Perpendicular distance between the CR of mandibular central incisor and mandibular plane (MP) |
| L1 to MP (°) | Angle formed by the long axis of mandibular central incisor and MP |
| L1 to APg (mm) | Perpendicular distance from mandibular incisor incisal edge to A-point–pogonion (APg) line |
| L6 to MP (mm) | Perpendicular distance from the mesiobuccal cusp tip of mandibular first molar to MP |
| U1 to L1 (°) | Angle formed by the long axes of maxillary and mandibular incisors |
∗ Mandibular plane (MP): formed by a line through menton, tangent to the lower border of the angle of the mandible.
† Xi: the geometric center of the ramus of the mandible.
‡ PM: protuberance menti point selected at the anterior border of the symphysis between Point B and pogonion where the curvature changes from concave to convex.
§ Occlusal plane (OP): formed by a line bisecting the overlapping cusps of the first molars and the incisal overbite.
‖ Center of resistance (CR): a point located at one-third of the distance of the root length apical to the alveolar crest.
Sixty randomly chosen lateral cephalograms were retraced and redigitized, and method error was calculated with Dahlberg’s formula.
Statistical analysis
Statistical analysis was completed using the Statistical Package for Social Sciences (version 13; SPSS, Chicago, Ill).
Because the Shapiro-Wilks test showed that all data were normally distributed, treatment (T2-T1), postretention (T3-T2), and overall changes (T3-T1) were compared by repeated measurements analysis of variance (ANOVA), followed by multiple comparisons with the Bonferroni adjustment. The significance level was set at P <0.05.
Results
The method error ranged from 0.15 mm (U1CR to PP) to 0.55 mm (L6 to MP) for the linear measurements, and from 0.25° (L1 to MP) to 0.45° (U1 to L1) for the angular measurements.
Because the sample size was 31 subjects and the 0.8-mm change in overbite in postretention period was statistically significant, the power of the study at a significance level of 0.05 was 0.86.
The mean values for the cephalometric measurements at T1, T2, and T3 are shown in Table II , and the treatment, postretention, and overall changes and their comparisons are shown in Table III .
| Measurement | Pretreatment | Posttreatment | Postretention |
|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | |
| SN to MP (°) | 32.7 ± 2.4 | 33.2 ± 2.6 | 33.4 ± 2.3 |
| ANS to Xi/Xi-PM (°) | 47.1 ± 1.9 | 47.3 ± 1.2 | 47.3 ± 1.9 |
| Overbite (mm) | 5.9 ± 0.7 | 2.0 ± 0.1 | 2.8 ± 0.4 |
| Overjet (mm) | 8.6 ± 1.3 | 2.1 ± 0.3 | 2.3 ± 0.2 |
| U1CR to PP (mm) | 12.9 ± 1.8 | 12.6 ± 2.1 | 12.8 ± 1.6 |
| U1 to PP (°) | 132.2 ± 5.4 | 115.2 ± 5.1 | 115.3 ± 5.4 |
| U1 to APg (mm) | 8.1 ± 1.4 | 4.3 ± 0.7 | 4.3 ± 0.6 |
| U6 to PP (mm) | 28.5 ± 4.1 | 28.4 ± 3.9 | 28.6 ± 3.9 |
| L1CR to MP (mm) | 28.2 ± 2.9 | 26.4 ± 2.1 | 27.3 ± 2.9 |
| L1 to MP (°) | 94.2 ± 2.8 | 94.6 ± 2.5 | 94.4 ± 2.6 |
| L1 to APg (mm) | 2.1 ± 0.9 | 2.8 ± 0.8 | 2.8 ± 0.6 |
| L6 to MP (mm) | 36.0 ± 2.5 | 36.9 ± 2.7 | 36.5 ± 2.6 |
| U1 to L1 (°) | 110.2 ± 3.8 | 131.7 ± 3.9 | 131.6 ± 4.1 |
| Measurement | Treatment changes (T2-T1) | Postretention changes (T3-T2) | Overall changes (T3-T1) | |||
|---|---|---|---|---|---|---|
| Mean ± SD | Sig | Mean ± SD | Sig | Mean ± SD | Sig | |
| SN to MP (°) | 0.5 ± 1.6 | NS | −0.2 ± 1.3 | NS | 0.6 ± 1.6 | NS |
| ANS to Xi/Xi-PM (°) | 0.2 ± 3.7 | NS | −0.1 ± 3.7 | NS | 0.2 ± 3.8 | NS |
| Overbite (mm) | −3.9 ± 0.7 | * | 0.8 ± 0.4 | * | −3.1 ± 0.8 | * |
| Overjet (mm) | −6.4 ± 1.2 | * | 0.4 ± 0.9 | * | −6.3 ± 1.2 | * |
| U1CR to PP (mm) | −0.3 ± 0.9 | NS | 0.1 ± 0.6 | NS | −0.2 ± 0.9 | NS |
| U1 to PP (°) | −17.0 ± 1.9 | * | −0.2 ± 0.8 | NS | −16.9 ± 0.4 | * |
| U1 to APg (mm) | −3.8 ± 1.1 | * | 0.1 ± 1.3 | NS | −3.7 ± 1.0 | * |
| U6 to PP (mm) | −0.1 ± 0.8 | NS | 0.2 ± 0.6 | NS | 0.1 ± 0.8 | NS |
| L1CR to MP (mm) | −2.6 ± 1.4 | * | 0.8 ± 1.1 | * | −2.1 ± 0.9 | * |
| L1 to MP (°) | 0.6 ± 0.9 | * | −0.2 ± 0.9 | NS | 0.3 ± 0.8 | NS |
| L1 to APg (mm) | 0.8 ± 1.5 | * | −0.1 ± 1.3 | NS | 0.7 ± 1.1 | * |
| L6 to MP (mm) | 0.8 ± 0.6 | * | −0.3 ± 0.5 | NS | 0.5 ± 0.6 | * |
| U1 to L1 (°) | 21.5 ± 5.1 | * | −0.1 ± 1.7 | NS | 21.4 ± 5.2 | * |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


