Introduction
A deepbite malocclusion should not be approached as a disease entity; instead, it should be viewed as a clinical manifestation of underlying discrepancies. The aim of this study was to investigate the various skeletal and dental components of deep bite malocclusion, the significance of the contribution of each, and whether there are certain correlations between them.
Methods
Dental and skeletal measurements were made on lateral cephalometric radiographs and study models of 124 patients with deepbite. These measurements were statistically analyzed.
Results
An exaggerated curve of Spee was the greatest shared dental component (78%), significantly higher than any other component ( P = 0.0335). A decreased gonial angle was the greatest shared skeletal component (37.1%), highly significant compared with the other components ( P = 0.0019). A strong positive correlation was found between the ramus/Frankfort horizontal angle and the gonial angle; weaker correlations were found between various components.
Conclusions
An exaggerated curve of Spee and a decreased gonial angle were the greatest contributing components. This analysis of deepbite components could help clinicians design individualized mechanotherapies based on the underlying cause, rather than being biased toward predetermined mechanics when treating patients with a deepbite malocclusion.
A deep overbite is a common malocclusion encountered in an orthodontic practice. Severe deepbites (overbite ≥5 mm) are found in nearly 20% of children and 13% of adults, representing about 95.2% of vertical occlusal problems. A deepbite malocclusion overlies a multitude of hidden skeletal or dental discrepancies. Accordingly, a deepbite should not be approached as a disease entity; instead, it is a clinical manifestation of an underlying skeletal or dental discrepancy.
Previous studies addressing deep overbite focused on detecting the changes in the dentoalveolar morphology accompanying the changes in overbite. Other studies aimed to evaluate the effect of age on the change in overbite and relate the increase in bite depth to other malocclusions.
Ceylan and Eroz studied some components of deep overbite in 4 groups of patients (20 patients in each group) with variable bite depths. Among their significant findings was that the gonial angle was the largest in the open-bite group and smallest in the deepbite group. Baydas et al studied the effect of the depth of the curve of Spee on bite depth in a sample of 137 subjects. They were divided into 3 groups; normal, flat, and deep curves of Spee, and the groups were compared. The results showed statistically significant correlations between the depth of the curve of Spee and overjet and overbite.
Although certain components were deemed to share in a developing deepbite malocclusion, thus classifying deepbite into dental and skeletal deepbite according to the causative factor, yet the various components of a deepbite malocclusion and the significance of their contributions to the problem have not been well investigated.
Regarding dental deepbite, a deep curve of Spee and an increased buccal root torque of the maxillary incisors were proven to be correlated with deepbite malocclusions. The overerupted maxillary and mandibular anterior alveolar basal heights and the undereruption of the maxillary and mandibular posterior segments were also shown to have positive correlations with deepbite malocclusions. Extraction of the mandibular incisors leads to a collapse of that arch with consequent deepening of the bite.
A skeletal deepbite could result from a discrepancy in the vertical position of the maxilla, the mandible, or their cant. Few studies have dealt with the components of skeletal deepbite; it was shown that the vertical component of mandibular growth has a more remarkable effect than the rotational component, and that the mandibular skeletal changes were twice as important as the mandibular dental changes and about 2.5 times as important as the maxillary changes in inducing overbite changes.
In this study, we aimed to explore the different components of deepbite malocclusion and determine their actual contributions in its development.
Material and methods
The sample comprised pretreatment lateral cephalograms and study models of 124 patients with deepbite, selected from approximately 2000 patient records at the outpatient clinic of the Department of Orthodontics of Cairo University in Egypt. The subjects were aged from 14 to 22 years, and their selection was based on following criteria: (1) deep overbite more than 5 mm, (2) complete eruption of the second molars, (3) no history of orthodontic treatment, (4) no severe craniofacial disorders, and (5) no missing teeth.
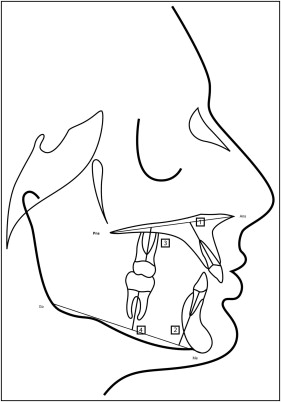
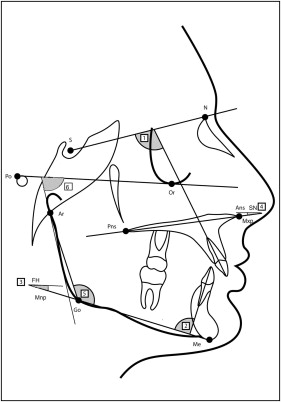
Cephalometric dental and skeletal measurements ( Table I ; Figs 1 and 2 ) were used in this study. A new skeletal measurement, ramus/Frankfort horizontal, was made between a tangent to the posterior border of the mandibular ramus and the Frankfort horizontal plane. Measuring this angle in the deepbite sample aimed to test whether the direction of growth and the angulation of the mandibular ramus have significant roles in developing deepbite malocclusions.
| Measurement | Definition |
|---|---|
| Dental | |
| Maxillary anterior alveolar and basal height (Mx-AABH, mm) | Distance between the midpoint of the alveolar meatus of the maxillary central incisor and the intersection point between the palatal plane and the long axis of the maxillary central incisor |
| Maxillary posterior alveolar and basal height (Mx-PABH, mm) | Perpendicular distance between the midpoint of the alveolar meatus of the maxillary first molar and the palatal plane |
| Inclination of the upper incisors (U1/SN, °) | Angle formed between the extension of the long axis of the maxillary incisor and the sella-nasion plane |
| Mandibular anterior alveolar and basal height (Md-AABH, mm) | Distance between the midpoint of the alveolar meatus of the mandibular central incisor and the intersection point between the mandibular plane and the long axis of the mandibular central incisor |
| Mandibular posterior alveolar and basal height (Md-PABH, mm.) | Perpendicular distance between the midpoint of the alveolar meatus of the mandibular first molar and the mandibular plane |
| Inclination of the mandibular incisors (L1/MP, °) | Angle formed between the extension of the long axis of the mandibular incisor and mandibular plane |
| Skeletal | |
| Mandibular plane angle (MndP-FH, °) | Angle formed between the mandibular plane and the Frankfort horizontal plane |
| Gonial angle (Ar-Go-Me, °) | Angle formed at the gonial area between the posterior border of the ramus and a corpus line |
| Maxillary plane angle (SN-MxP, °) | Angle formed between the maxillary plane and the sella-nasion plane |
| Ramus/FH (°) | A new skeletal measurement made between a tangent to the posterior border of the mandibular ramus and the Frankfort horizontal plane |
Cephalometric and dental cast measurements of 10 patients were repeated by the same observer (M.D.) after 4 weeks and by a second observer (M.F.) to measure the intraobserver and interobserver reliabilities ( Table II ).
| Measurement | Definition |
|---|---|
| Length of the clinical crown of the maxillary central incisors | Line formed between the midpoint of the cervical margin of the tooth and the midpoint of the incisal edge |
| Length of the clinical crown of the mandibular central incisors | Line formed between the midpoint of the cervical margin of the tooth and the midpoint of the incisal edge |
| Curve of Spee | Line formed between the deepest point on the mandibular buccal segment and a horizontal line formed between the most overerupted mandibular incisor and the most overerupted molar |
Statistical analysis
Descriptive statistics were calculated, including the mean and standard deviation of each dental and skeletal component of deepbite malocclusion, with the percentage of contribution of each component.
Inferential statistics included the hypothesis test (paired t test) used to compare the significance of the contribution of each component to a deepbite malocclusion.
The Pearson correlation coefficient was used to correlate the various deepbite components. The concordance correlation coefficient was used to calculate the intraobserver and interobserver reliabilities.
Results
The statistical analysis of the measurements showed the following results.
The means, standard deviations, and percentages of contribution of the dental and skeletal components of deep overbite are given in Table III .
| Component | n | Minimum | Maximum | Mean | SD | Coefficient of variation |
|---|---|---|---|---|---|---|
| U1 inclination (°) | 124 | 78.00 | 133.00 | 105.94 | 10.58 | 10.0% |
| L1 inclination (°) | 124 | 61.00 | 119.00 | 95.38 | 8.76 | 9.2% |
| Mandular plane (°) | 124 | 14.00 | 40.00 | 27.20 | 5.23 | 19.2% |
| U1 overeruption (mm) | 124 | 19.00 | 39.00 | 26.13 | 3.91 | 14.9% |
| L1 overeruption (mm) | 124 | 25.00 | 45.00 | 36.07 | 3.90 | 10.8% |
| U6 undereruption (mm) | 124 | 14.00 | 33.00 | 23.32 | 2.93 | 12.5% |
| L6 undereruption (mm) | 124 | 21.00 | 43.00 | 32.21 | 4.19 | 13.0% |
| U1 length (mm) | 124 | 7.00 | 12.50 | 10.34 | 1.21 | 11.7% |
| L1 length (mm) | 124 | 5.00 | 12.00 | 8.62 | 1.16 | 13.5% |
| Curve of Spee (mm) | 124 | 0.10 | 6.70 | 2.63 | 1.12 | 42.5% |
| Maxillary plane (°) | 124 | 3.00 | 24.00 | 10.56 | 3.78 | 35.8% |
| Gonial angle (°) | 124 | 109.00 | 146.00 | 124.91 | 6.60 | 5.3% |
| Ramus/FH (°) | 124 | 64.00 | 94.00 | 82.06 | 5.54 | 6.8% |
Among the dental components ( Fig 3 ), an exaggerated curve of Spee showed the highest contribution to a deepbite malocclusion (78%), followed by the overeruption of the maxillary incisors (66.1%), the undereruption of the mandibular buccal segment (50%), the undereruption of the maxillary posterior segment (41.1%), the overeruption of the mandibular incisors (37.1%), the increased clinical crown length of the maxillary incisors (32.3%), the retroclination of the maxillary incisors (24.2%), and the retroclination of the mandibular incisors (21.8%), and the least contributing factor was the increased clinical crown length of the mandibular incisors (12.1%).
Among the skeletal components ( Fig 4 ), a decreased gonial angle was found to contribute the most to a deepbite malocclusion (37.1%), followed by the maxillary plane’s clockwise rotation (32.2%) and the mandibular plane angle (19.3%).
The mean of the new measurement, ramus/Frankfort (°) horizontal, was 82.06° ± 5.54° in deepbite patients, representing the mean of the angulation of the mandibular ramus with respect to the Frankfort horizontal.
Regarding the contribution of the dental components ( Table IV ) to a deepbite malocclusion, the curve of Spee was significantly the highest of all other components ( P = 0.0335). The overeruption of the maxillary incisors was the second highest shared dental component in deepbite malocclusions and significantly higher than all other shared components ( P = 0.0101). The undereruption of the mandibular posterior segment was significantly higher than other smaller components ( P = 0.0404). The undereruption of the maxillary posterior segment, the overeruption of the mandibular incisors, and the increased clinical crown length of the maxillary incisors were the fourth level dental components that share in deepbite malocclusion and were significantly higher than the other smaller components ( P = 0.0275). The fifth level of shared dental components included lingually inclined maxillary and mandibular incisors, which were significantly greater in their contributions to deepbite malocclusion ( P = 0.0135) than the least contributing component, which was the increased clinical crown length of the mandibular incisors.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


