and Augusto Ureña1
(1)
Department of Orthodontics, Maimonides University, Buenos Aires, Argentina
Deep overbite is one of the most common and difficult malocclusions to treat and maintain stability in adult patients. It may be present with or without other dental problems. Its prevalence is 5–8 % in our population.
A very deep bite may result in damage to the soft palatal tissues and abnormal wear of the lower front teeth or on the palatal surfaces of the anterior upper incisors causing tooth sensitivity or pain.
It is fundamental to understand its etiology since it varies from patient to patient. Skeletal or dental deep bite are caused by genetic, environmental factors, or a combination of both (Geron and Vardimon 2003; Geron et al. 2004).
Exaggerated curve of Spee, abrasion, loss of posterior teeth, overeruption and retroinclination of the upper incisors, short mandibular ramus, short lower facial third, decreased gonial angle, etc. are the most common features.
The anterior facial height, chin position, amount of exposure of the maxillary and mandibular anterior teeth at rest and during function, and amount of gingival display are relevant factors to be considered in the treatment planning.
It can be corrected by extrusion of the upper or lower posterior teeth, intrusion of the upper or lower incisors, or a combination of both.
The treatment protocol differs if the posterior vertical dimension is lost or not and if a remnant growth spur is present or not.
Avoiding excessive extrusion of the maxillary molars and leveling occlusal plane would allow better control of the vertical changes. When extrusion of the lower incisors is present, lingual intrusive force is applied more closely to the center of resistance of the lower incisors producing their intrusion with little flaring.
Unfortunately, there is no specific cephalogram to determine the best plan of treatment.
Treating this malocclusion using lingual brackets with bite plane has many advantages. The temporary open bite at the anterior region provides a slight open bite on the bicuspids and molars that allows the leveling of the occlusal plane (Forsberg and Hellsing 1984; Magnus and Hellsing 1984; Carano 2008).
The discomfort caused by the bite plane of the brackets disappears within a few days after they are placed. Patients that have pain or tension in the temporomandibular joints feel relief of their symptoms in the first week.
The posterior inocclusion allows a slow eruption of the posterior teeth and helps to achieve a neuromuscular balance which is important to maintain the results.
The extrusion of the posterior teeth is recommended in patients with short lower facial height, excessive curve of Spee, and moderate to minimal incisor display. But the stability of posterior extrusion may be questionable in nongrowing patients.
Incisor intrusion is suggested with long lower facial height, excessive incisor display at rest and smile, and/or overeruption of upper incisors.
Contrary to what may be supposed, brackets don’t come off so easily since the design of the bite plane protects them (Gorman and Smith 1991).
It is important to normalize the incisor’s torque in the first phase of treatment.
The use of a 0.017″ × 0.017″ Ni-Ti-Cu followed by a 0.0175″ × 0.0175″ TMA wire helps in achieving the desired results.
It is important to remember that the major esthetic factors to be considered when planning the correction of a deep bite occlusion are incisor display, occlusal plane, and interlabial gap because the smile line becomes a crucial factor in deciding the treatment plan.
An individualized retention plan is the KEY for long-term success combining the control of the new position of the teeth as well as the muscles.
Case Study 1
A 29-year-old patient consulted because she had a significant overbite and lower anterior crowding. She had used removable appliances when she was 8–11 years old with no long-term retention plan.
The midlines were not coincident as she had Class I on the right side and Class II on the left side.
Her only chief complaint was the lower anterior crowding (Fig. 3.1a, b)..
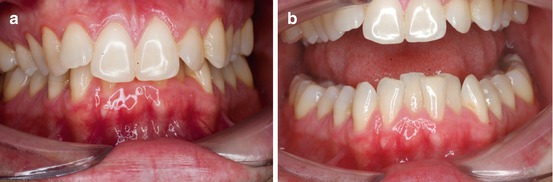
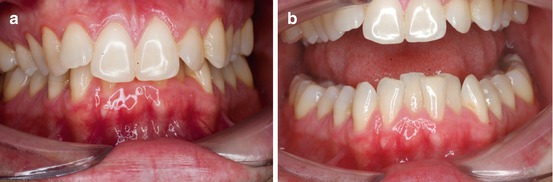
Fig. 3.1
(a, b) Pretreatment buccal front photographs. The important overbite and the lower anterior crowding were evident
Clinical examination revealed some pain at the temporomandibular joints especially when she was yawning. An important extrusion of the upper incisors was evident and the lower gingival line was uneven.
The lateral photographs confirmed that the molar relationship was Class I on the right side and Class II on the left.
The extrusion and retroinclination of the upper central incisor were confirmed.
The gingival line and the occlusal plane were not parallel (Fig. 3.2a, b).
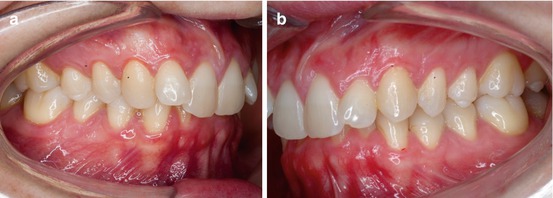
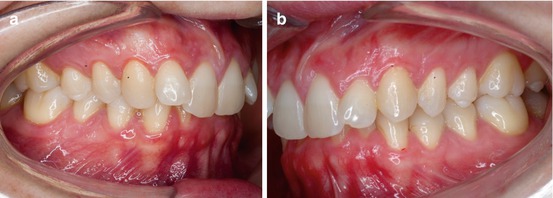
Fig. 3.2
(a, b) Lateral views at the beginning of the treatment
The upper occlusal arch was constricted, more evident on the right side. The upper lateral incisors were labial inclined, and the discrepancy was about 4 mm in the upper arch and 9 mm in the lower one (Fig. 3.3a, b).
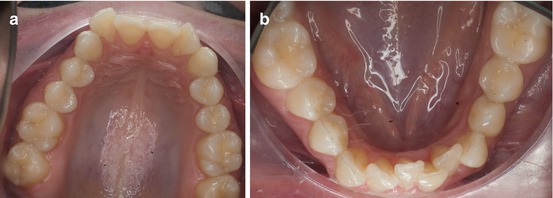
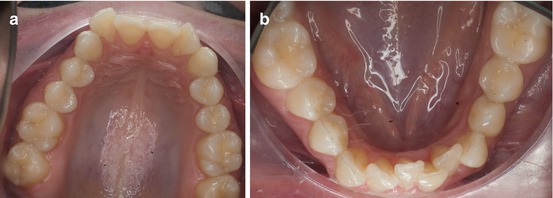
Fig. 3.3
(a, b) Upper and lower arches where the asymmetry and the lower crowding were quite evident
Cephalometric analysis showed that she is a severe braquifacial patient. Her convexity is −1 mm and the lower inferior height only 40°. The upper and lower incisors were retroinclined (+14° and +15°, respectively) and the interincisal angle was 155°.
A slight asymmetry between the right and left condyle was present (Fig. 3.4a, b).
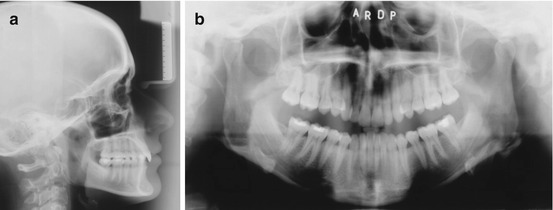
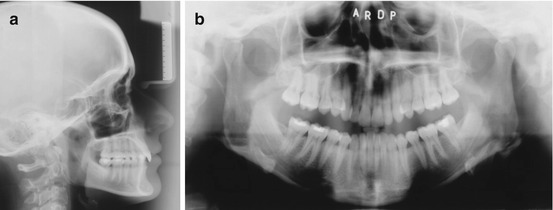
Fig. 3.4
(a, b) Pretreatment panoramic and lateral radiographs
Treatment Objectives
1.
Align and level the arches.
2.
Normalize overjet and overbite.
3.
Maintain periodontal health.
4.
Maintain Class I molar on the right side and Class II on the left side.
5.
Improve esthetics.
6.
Long-term stability.
To achieve the treatment objectives, a treatment plan without extractions was suggested.
The use of lingual brackets with a bite plane is preferable in order to open the anterior bite and allow a temporary slight posterior inocclusion.
Indirect bonding was recommended from second molar to second molar in conjunction with a low load deflection arch (Ni-Ti 0.013″) and an open coil spring to gain space for the lateral incisors (Fig. 3.5a, b).
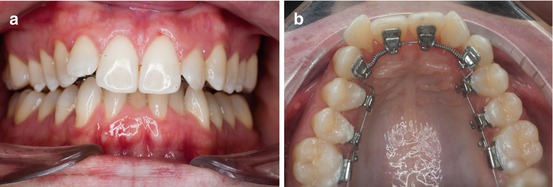
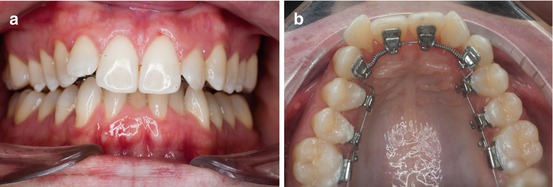
Fig. 3.5
(a, b) Front and upper occlusal arch at the beginning of the treatment
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


