Introduction
This article introduces a technique combining corticotomy and orthodontic forces, or accelerated osteogenic orthodontics, for use in patients with a Class III occlusion and a thin alveolus who will undergo orthognathic surgery.
Methods
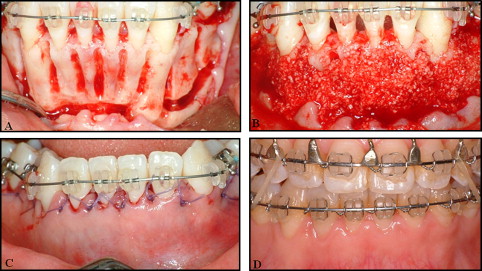
Two adults with Class III malocclusion undergoing anterior decompensation for mandibular setback surgery were selected. The first patient was treated with accelerated osteogenic orthodontics and conventional decompensation. The second patient was treated with accelerated osteogenic orthodontics and decompensation with a temporary skeletal anchorage device in concert with guided tissue regeneration. Decortication of bone was performed to the mandibular teeth with a low-speed round bur and piezosurgery. After hemostasis, bone graft material was placed into the decorticated area. In the severely thin alveolar ridge, a rigid scaffold was applied for immobilization of graft material. After approximation of the flap, an immediate orthodontic force was applied to the teeth to initiate rapid tooth movement.
Results
Rapid tooth movement into predetermined positions for orthognathic surgery was accomplished in all mandibular anterior teeth. Preoperative 3-dimensional imaging showed dehiscences on the facial aspects of the mandibular anterior teeth. Postoperative imaging demonstrated coverage of the denuded roots with radiodense material.
Conclusions
The accelerated osteogenic orthodontic technique is a safe and effective treatment option for mandibular anterior decompensation treatment of these patients. When combined with a temporary skeletal anchorage device and bone augmentation, this technique facilitated the decompression of the mandibular anterior teeth in severely compromised dentitions.
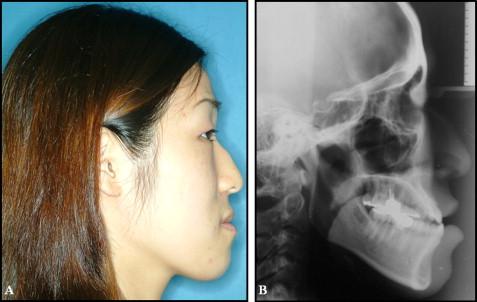
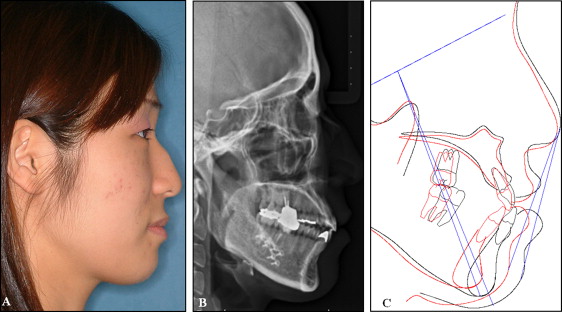
Treatment of severe skeletal Class III malocclusion in adults often requires decompensation, including labial inclination of the mandibular incisor teeth before orthognathic surgery ( Fig 1 ). Although this procedure leads to improved facial and dental esthetic outcomes, periodontal complications can result, including bony dehiscences, fenestrations, and gingival recession. The occurrence of alveolar bone loss or fenestration might be more common in skeletal Class III adult patients undergoing orthognathic surgery, especially in the mandibular anterior teeth, because of the decompensation procedure on the thin facial alveolus ( Fig 2 ). During orthodontic treatment, limiting incisor movement in the bone structure is believed to be essential for achieving better results, stability, and periodontal health, as well as for avoiding root resorption.

A thin alveolus can be encountered in any skeletal type but is most frequently found in patients with a long lower face height and a skeletal Class III malocclusion. Some researchers have shown that, in the case of a narrow and high symphysis, pronounced sagittal or anteroposterior incisor movements during routine orthodontic treatment might be critical and lead to progressive bone loss of the lingual and labial cortical plates because of the anatomic limits set by the cortical plates of the alveolus at the level of the incisor apices.
Accelerated osteogenic orthodontics has been proposed as a technique to facilitate tooth movement by a combination of corticotomy and orthodontic forces. The biologic basis of accelerated osteogenic orthodontics has been suggested to be mediated by a regional acceleratory phenomenon. It has been hypothesized that a corticotomy or an osteotomy can lead to intensified osteoclastic activity resulting in osteopenia and increased bone remodeling. This has been extrapolated to the dentoalveolar complex, suggesting that when tooth movement is preceded by surgical flap surgery and decortication, the osteopenia and increased bone turnover facilitate tooth movement. The technique entails reflection of a mucoperiosteal flap, removal of the cortical plate over the teeth, and augmentation of the alveolar bone with graft material and flap closure. Orthodontic force is immediately applied that induces not only tooth movement, but also remodeling of the bone and the graft material.
The accelerated osteogenic orthodontic approach has been applied in arch expansion, as well as for treatment of severe crowding without extractions. The application of this principle for decompensation of the mandibular anterior teeth of Class III patients undergoing orthognathic therapy has not been previously reported. When dense cortical bone is decorticated, augmented with graft material, and followed by immediate orthodontic force, we have observed similar effects characteristic of an accelerated osteogenic orthodontic procedure. Corticotomy of the alveolar bone facilitates orthodontic tooth movement compared with conventional orthodontic treatment. Decortication is performed at clinical sites without entering the cancellous bone, avoiding risk of damage to underlying structures, such as the mandibular canal and root surfaces. Sufficient bleeding in the decorticated area must be followed up, and then the bone graft material placed. We have used bovine anorganic bone (Bio-Oss; Geistlich Pharma AG, Wolhusen, Switzerland) for the augmentation. After flap repositioning, an immediate heavy orthodontic force can be applied to the teeth. It is critical to achieve primary coverage to protect the bone graft material. In patients with a severely compromised dentition and a thin alveolus, accelerated osteogenic orthodontic treatment as the sole procedure is insufficient for decompensation. The use of bone grafts combined with guided tissue regeneration can serve as a scaffold for clot formation and stabilization. This clinical report describes novel techniques for adults undergoing accelerated osteogenic orthodontic treatment alone or combined with guided tissue regeneration to repair the osseous defect caused by mandibular anterior decompensation in Class III orthognathic patients.
Clinical applications
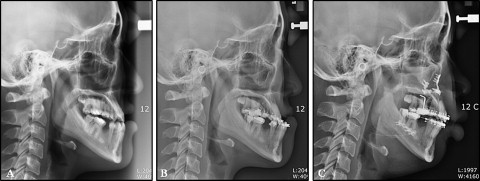
Patient 1 had mandibular anterior decompensation with accelerated osteogenic orthodontics. In this 25-year-old woman, a skeletal Class III occlusal relationship, constricted maxillary and mandibular dentitions, missing mandibular second premolars, and lingually inclined mandibular incisors were observed ( Figs 3 and 4 , A ). Her medical history was unremarkable. The patient was informed about the difference between the conventional decompensation procedure and the accelerated osteogenic orthodontics combined procedure. After learning of the option of decompensation of the lingually tipped mandibular anterior teeth, she chose the latter. Because the tooth movement required for determined decompensation was relatively small, the accelerated osteogenic orthodontic procedure and conventional orthodontic treatment were selected.
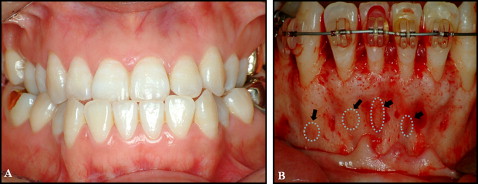
The facial flap of the mandibular anterior teeth was reflected, and accelerated osteogenic orthodontics was performed ( Figs 4 , B , and 5 ). All 6 mandibular anterior teeth exhibited reduced alveolar bone height with dehiscences in the labial cortical plate ( Fig 4 , B ). The decortication area was filled with bone graft material, and a 0.019 × 0.025-in reverse curve of Spee nickel-titanium archwire was applied to the mandibular dentition immediately after suturing ( Fig 5 , A-C ). After 5 months of decompensation, a bilateral sagittal split ramus osteotomy was performed ( Fig 5 , D ). The total active treatment period was 9 months. After active therapy, well-balanced facial harmony, and Class I canine and molar relationships were achieved ( Fig 6 ). The posttreatment lateral cephalogram and the 2-year retention cone-beam computed tomography images showed a relatively well-maintained mandibular anterior alveolus ( Fig 7 ). There were generalized probing depths of 1 to 2 mm in the mandibular anterior area after therapy.
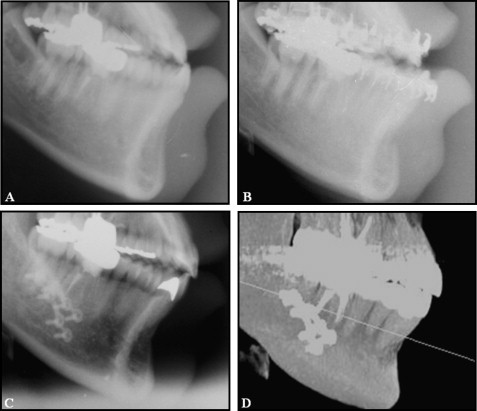
Patient 2 had mandibular anterior decompensation with accelerated osteogenic orthodontics in conjunction with a temporary skeletal anchorage device and guided tissue regeneration. In cases of severely compromised dentition, accelerated osteogenic orthodontics is not sufficient to decompensate the lingually tipped mandibular anterior teeth. To prevent root dehiscence during decompensation despite an accelerated osteogenic orthodontics procedure, a specially designed barrier for bone graft housing was used.
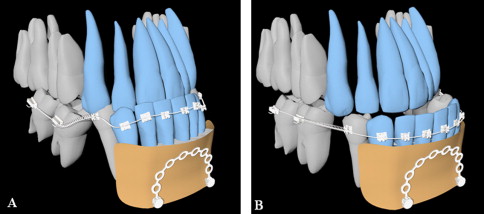
We developed a novel bone augmentation technique involving a surgical miniplate attached by 2 fixation screws (diameter, 2 mm; length, 7 mm; Jin Biomed Co., Bucheon, Korea) and an expanded Polytetrafluoroethylene nonresorbable membrane on the mandibular facial alveolar area ( Fig 8 ). This temporary skeletal anchorage device barrier provided a rigid scaffold for application of sufficient bone graft material to the decorticated area to account for the resorption of bone graft material during the decompensation procedure.