Resin Composite
Bond strength (MPa)
Failure location (%)
A
8
100 – adhesive
B
18
100 – cohesive in resin composite
C
26
100 – cohesive in enamel
In this experiment, the bond strength of resin composite A was lower than its cohesive strength and the resin composite separated cleanly from the tooth. The relatively low bond strength of resin composite A might suggest that this resin composite bonds poorly to enamel, or that the enamel surface was contaminated, resulting in an inferior bond. In contrast, there were cohesive failures in the resin composite for resin composite B and in the enamel substrate for resin composite C. The relatively high values of “bond strength” demonstrate that these resin composites bonded well to enamel, although the actual values of bond strength are not known; however, the 100 % cohesive failure in resin composite B might indicate that it was poorly polymerized. The 100 % cohesive failure in the enamel substrate for resin composite C might indicate that the enamel substrate was thin or cracked.
Bond Strength Measurement by Tensile and Shear Testing
Bond strength testing typically is performed in tension or shear, using a screw-driven or servohydraulic universal testing machine [1]. In tensile testing the restorative material is pulled perpendicularly from the enamel substrate. Two popular tensile bond tests include the inverted, truncated cone test (Fig. 3.1) [2] and the microtensile test (Fig. 3.2) [3]. In a study of two bonding agents bonded to enamel, superficial dentin and deep dentin for wet, moist, and dry conditions, microtensile bond strengths were found overall to be approximately 30 % higher than inverted cone bond strengths (p = 0.002, r2 = 0.45; Table 3.2) [4]. The higher bond strengths observed with the microtensile test may be related to the smaller diameter of the bonded interface.
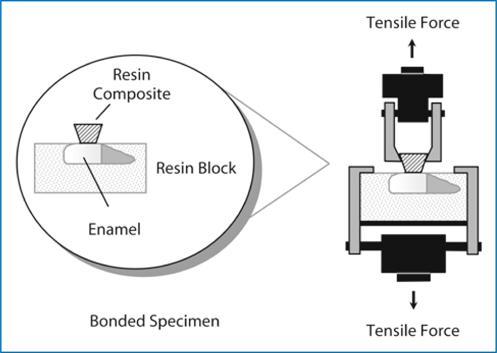
Fig. 3.1.
Test assembly (isolated interface model) for debonding adhesive from human enamel in tension. (From [15])
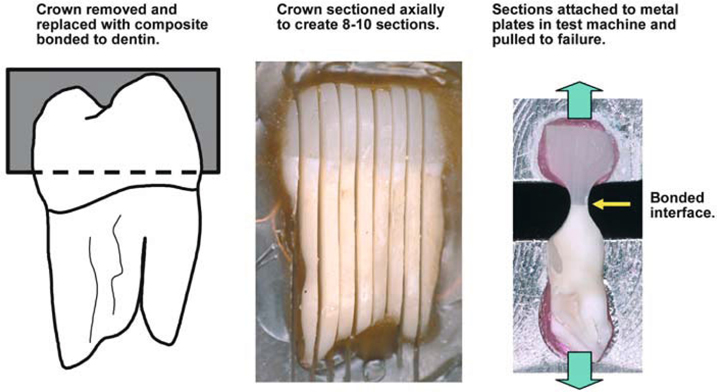
Fig. 3.2.
Test assembly for microtensile bond test. (From [1])
Table 3.2.
Comparison of two in vitro tensile bond tests for measurement of bond strengths (MPa) of two bonding agents and a resin composite bonded to wet, moist, and dry human enamel. (From [4])
|
Bonding agent
|
Wet
|
Moist
|
Dry
|
|---|---|---|---|
|
Inverted cone tensile test
|
|||
|
Fifth generation (Single Bond)
|
21.0
|
20.2
|
26.6
|
|
Sixth generation (EXL 542)
|
20.2
|
25.0
|
19.8
|
|
Microtensile test
|
|||
|
Fifth generation (Single Bond)
|
31.6
|
38.5
|
32.2
|
|
Sixth generation (EXL 542)
|
15.7
|
24.5
|
14.8
|
In shear testing, the bonded bracket is loaded by a blade in tension or compression or by a wire loop in tension, so that the bracket slides parallel to the enamel surface [1]. Pure shear loading is difficult to achieve, and most shear testing also includes components of peeling, tension, and torsion.
Both tensile and shear loading modes are valid tests for studying bond strengths of restorative materials. The goal in bond testing should be to achieve a coefficient of variation [(standard deviation/mean) × 100 %] in the range of 20-30 %. Typically, tensile testing produces a lower coefficient of variation than the most common shear tests.
Bond testing using teeth involves many variables that can affect the measured bond strength. These variables include: (a) type of tooth (e.g., incisor, molar, human, bovine); (b) fluoride content of tooth; (c) disinfection and storage media of tooth before bonding; (d) elapsed time of storage following bonding; (e) type of loading (shear, tension); (f) configuration of specimen testing jig; (g) crosshead speed of mechanical testing machine; and (h) bonding area of the specimen. A technical specification (dental materials – testing of adhesion to tooth structure, ISO/TS 11405 N355) currently is under development to standardize testing protocols for bond strength measurements.
Experimental Models for Evaluating Bond Strength
Evaluation of bond strength can be studied in vitro using a simulated clinical model. A more fundamental test is the isolated substrate model in which bonding of an adhesive-to-tooth structure or a restorative material is studied independently. Retention of restorations or bond failures can be studied clinically using prospective or retrospective clinical models.
Clinical Simulation Model
In this model, for example, an orthodontic bracket would be bonded to an extracted tooth using an orthodontic resin cement [5]. Then, the bracket-tooth system would be loaded in a testing machine to cause a bond failure. This technique appears to be clinically relevant. The disadvantage of this simulated test is that bond failures often occur at several interfaces (bracket/cement, tooth/cement), so it is difficult to isolate variables that may affect bond failure.
Isolated Interface Model
Clinical Studies
The randomized clinical trial is an experimental study in which the investigator selects and controls the treatments under study in order to draw conclusions about whether a particular treatment produced an effect [6]. The converse of the prospective study is the retrospective (observational) study, which involves the examination of previous treatment records to obtain data for analysis. The investigator thus obtains research data by observing treatment events without controlling them. Advantages and disadvantages of prospective and retrospective clinical studies are summarized in Table 3.3 [6].
Table 3.3.
Summary of advantages and disadvantages of prospective and retrospective clinical studies. (From [6])
|
Type of study
|
Advantages
|
Disadvantages
|
|---|---|---|
|
Prospective
|
Randomization reduces bias
|
Patients lose choice of treatment
|
|
Conclusions may be stronger
|
Patients may drop out of study Ethical concerns if one treatment is perceived as inferior
|
|
|
Retrospective
|
Minimal expenses
|
Variations in patients may cause confounding effects
|
|
Easy to perform (record review)
|
Interpretation of charts (possible bias)
|
Variables Affecting in Vitro Bond Strength
Differences Among Teeth
Differences in shear bond strength among maxillary teeth (6-13 MPa) and among mandibular teeth (9-13 MPa) have been reported [7]. Permanent teeth tend to produce similar or slightly higher bond strengths than primary teeth (Table 3.4) [8, 9, 10].
Table 3.4
In vitro tensile bond strengths (MPa) of self-etching adhesive systems and resin composite to human enamel
|
Adhesive system
|
Permanenta
|
Primaryb
|
|---|---|---|
|
Self-etching primer and adhesive (Clearfil SE Bond)
|
29
|
19
|
|
Self-etching adhesive (Prompt L-Pop)
|
22
|
19
|
Table 3.5.
Range of in vitro tensile bond strengths (MPa) of resin composite with four generations of bonding agents bonded to moist human enamel and superficial dentin. (From [14])
|
Bonding agent
|
Enamel
|
Superficial dentin
|
|---|---|---|
|
Fourth generation
|
23-32
|
21-24
|
|
Fifth generation
|
19-33
|
18-22
|
|
Sixth generation
|
17-29
|
17-35
|
|
Seventh generationa
|
22
|
15
|
Phosphoric Acid
In restorative dentistry the highest possible bond strength to tooth structure is desirable. Bond strengths of resin composites used with fourth-, fifth-, sixth-, and seventh-generation bonding agents to human enamel and dentin are considered satisfactory [11–14]. Generally, bond strengths to enamel are higher than those to superficial dentin (Table 3.5). Additional information on sixth- and seventh-generation bonding agents is presented in the next section of this chapter.
In contrast, the orthodontic bond strength must be sufficient to retain the brackets but low enough to allow easy cleanup of adhesive when the case is completed and the brackets are removed. Some factors that influence acid etching of enamel for orthodontic bonding include the type and concentration of the acid and the time of etching [6].
Compomers (polyacid-modified resins) bond well to enamel (Table 3.6) [15]. The highest bond strengths are achieved with the use of phosphoric acid etching and a bonding agent, although there is limited bonding of the compomer by itself to moist enamel.
Table 3.6.
In vitro tensile bond strengths (MPa) of a compomer (Compoglass F) bonded to moist and wet human enamel as affected by etching with phosphoric acid and use of a bonding agent. (From [15])
|
Phosphoric acid
|
Bonding agent*
|
Moist
|
Wet
|
|---|---|---|---|
|
Yes
|
Yes
|
20.3a
|
19.8a
|
|
Yes
|
No
|
15.5b
|
0.0
|
|
No
|
Yes
|
15.2b
|
10.8
|
|
No
|
No
|
3.5
|
0.0
|
Hybrid ionomers (resin-modified glass ionomers) also bond to enamel (Table 3.7) [16]. The highest bond strengths of hybrid ionomers to enamel are observed when the enamel is etched with phosphoric acid. Etching with a polyacrylic acid conditioner (10 or 20 %) typically produces lower bond strengths than etching with phosphoric acid. Some hybrid ionomers are self-adhesive, although bond strengths are usually < 15 MPa.
Table 3.7.
In vitro tensile bond strengths (MPa) of hybrid ionomers bonded to human enamel as affected by etching with phosphoric acid. [From (16)]
|
Phosphoric acid
|
Fuji Ortho
|
Fuji Ortho LC
|
Vitremer
|
|---|---|---|---|
|
Yes
|
26.7a
|
22.1
|
16.8
|
|
No
|
25.4a
|
14.6
|
8.4
|
Acidic Primers and Adhesives
An alternative to etching enamel with phosphoric acid is to use self-etching bonding agents, often referred to as sixth- or seventh-generation bonding agents. The sixth-generation bonding agents include the self-etching primer and adhesive (apply primer, then apply adhesive) and the self-etching adhesive (mix components, then apply adhesive). The seventh-generation bonding agents are no-mix, self-etching adhesives (apply adhesive). With these bonding agents, no phosphoric acid is used and no rinsing is necessary, and bond strengths to enamel and superficial dentin can be adequate (Table 3.8) [8].
Table 3.8.
In vitro tensile bond strengths (MPa) of a resin composite bonded to human enamel treated with a self-etching bonding agent. [From (8)]
|
Resin Composite
|
Enamel
|
Superficial Dentin
|
Deep Dentin
|
|---|---|---|---|
|
Adper Prompt L-Pop
|
22.4
|
8.4
|
5.7
|
|
Clearfil SE Bond
|
29.1
|
27.3
|
20.2
|
|
Etch & Prime
|
21.5
|
3.2
|
1.3
|
Several fifth-generation bonding agents (One-Step Plus, Optibond Solo Plus) have the option of using either phosphoric acid or a self-etching primer before application of the adhesive. In general, the bond strengths are comparable (Table 3.9). [17].
Table 3.9.
In vitro tensile bond strengths (MPa) of resin composites bonded to human enamel treated with either phosphoric acid or a self-priming etchant and a fifth-generation bonding agent. (From [17])
|
Resin Composite
|
Phosphoric acid/One-Step Plus
|
Tyrian SPE/One-Step Plus
|
|---|---|---|
|
Filtek Z250
|
19.4
|
19.1
|
|
TPH Spectrum
|
17.7
|
16.3
|
|
Tetric Ceram HB
|
18.6
|
17.0
|
The bond strength of light-cured bonding agents can be affected by the use of self-cured resins. In particular, bonding agents with acidic components may exhibit reduced bond strengths with a self-cured, orthodontic resin cement (Table 3.10) [18].
Table 3.10.
In vitro tensile bond strengths (MPa) of light-cured (Transbond) or self-cured (Concise Orthodontic) orthodontic resin cements bonded to human enamel treated with self-etching bonding agents. (From [18])
|
Bonding agent
|
Light-cured cement
|
Self-cured cement
|
|---|---|---|
|
Phosphoric acid (control)
|
12.9
|
21.4
|
|
Self-etching primer + adhesive (Clearfil SE Bond)
|
22.7
|
13.3
|
|
Self-etching adhesive (Prompt L-Pop)
|
17.0
|
0.0
|
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


