http://evolve.elsevier.com/Haveles/pharmacology
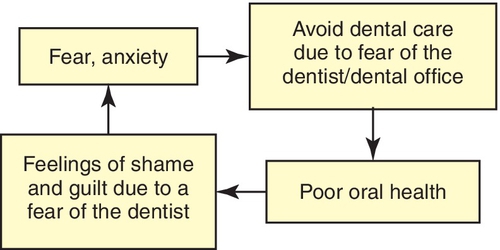
Many patients who require dental care never go to the dental office because of fear and apprehension. Almost 20% of Americans seek oral health care only when absolutely necessary, whereas approximately 7% refuse to seek any care because they are afraid. Those patients who avoid maintenance oral health care examinations and those who come in only when in severe pain further raise their levels of anxiety. Patients who delay treatment are now faced with longer appointments that may require oral injections; all of these factors lead to increased anxiety levels (Figure 11-1).
Both the dental hygienist and the dentist recognize the value of a relaxed patient. Often, patient anxiety is sufficiently reduced by a calm, patient, confident, and understanding attitude on the part of the dental health care team. However, individual responses to dental treatment vary widely, ranging from total relaxation and even sleeping to severe apprehension and the inability to approach the dental office, much less the dental chair. Each dental patient should be provided with the most pleasant experience possible within the limits of safety. When the patient is relaxed, appointments can be more productive, and the dentist, hygienist, and patient all benefit.
Dental hygienists and dentists can help a patient overcome his or her fears by meeting with the patient in the office and not in the treatment chair. They should discuss the procedure and all concerns that the patient may have and let the patient get to know them. Some patients are fearful of the instruments and their noises. If possible, allow the patient to hold the instruments and encourage the patient to bring in ear plugs or music to listen to during the appointment. Other patients may feel uncomfortable lying completely back during an oral examination. In this instance, simply putting the patient in a semireclined position may alleviate the fears. Ask the patient’s opinion, allowing the patient to feel in control of the situation. All of these actions helps dental health care team develop empathy toward the patient and provide for a much more stress-free visit.
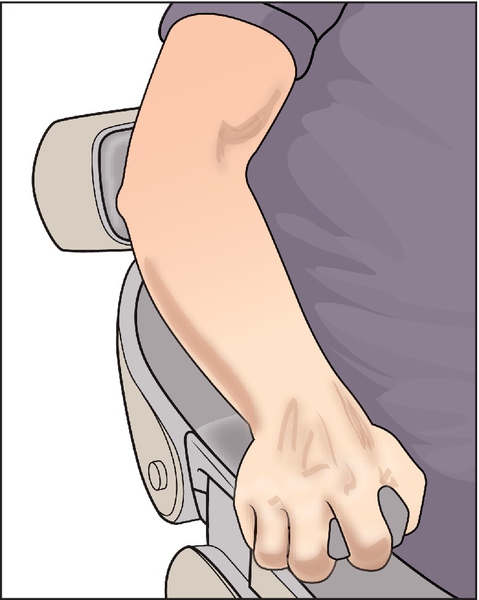
The appropriate use of antianxiety agents might encourage more patients to seek needed dental treatment. It is necessary to objectively assess each patient’s anxiety on both the first and subsequent visits. A patient who is clutching the dental chair arms and has white knuckles is not in a relaxed state (Figure 11-2). By questioning and observing the patient, the dental care team can determine the need for antianxiety agents. Thus the patient can feel comfortable and relaxed during subsequent dental appointments. The dental health professional should remember that whatever procedure is performed, he or she has performed it many times. However, for many patients, this may be the first experience with the procedure, and their reactions may be altered by their interpretation of what is happening (e.g., “that sharp, pointy thing is going to hurt!” or “What are those gunlike things?”).
As there are many different drugs available to treat anxiety, the dental practitioners should become familiar with one or two drugs and use them repeatedly. In the long run, this practice will produce greater benefits than changing from drug to drug. The dose of a particular antianxiety agent that is effective for a particular patient is vastly variable, involving both intrapatient and interpatient variations. Predicting the correct dose is a guess at best. The amount needed is poorly related to the patient’s anxiety level or the dental procedure to be performed. The normal sedative dose (calms normal patient without dental appointment) is not expected to produce calmness in a dental patient, but the hypnotic dose (induces sleep in the normal patient) can often achieve the desired degree of sedation before dental treatment.
Definitions
The sedative-hypnotic agents can produce varying degrees of central nervous system (CNS) depression, depending on the dose administered. A small dose causes mild CNS depression described as sedation (reduction of activity and simple anxiety). This level of CNS depression has some anxiolytic effects. A larger dose of the same drug, the hypnotic dose (inducing sleep), produces greater CNS depression. Thus the same drug may be either a sedative or a hypnotic, depending on the dose administered.
This chapter discusses the benzodiazepines, the barbiturates, and the nonbenzodiazepine-nonbarbiturate sedative-hypnotics. The benzodiazepines are discussed first because they are used most often.
Benzodiazepines
The benzodiazepines (ben-zoe-dye-AZ-e-peens) are the most commonly prescribed antianxiety drugs. The members of this group differ mainly in onset and duration of action, dose, and dose forms available (Table 11-1).
Table 11-1
Benzodiazepines and Miscellaneous Sedative-Hypnotic Agents
* Used as an adjunct to treat certain kinds of seizures.
† Injectable form contains propylene glycol—can produce thrombophlebitis.
‡ Available parenterally.
§ Midazolam administered intravenously in United States.
|| Sublingual dose form.
Chemistry
These drugs are named benzodiazepines because of their structure: a 1,4-benzodiazepine nucleus.
Pharmacokinetics
The benzodiazepines are well absorbed when administered by the oral route. The rapid onset of action of the benzodiazepines is related to their lipid solubility. Diazepam, which is highly lipid soluble, has a quick onset and is concentrated in the adipose tissue. Storage in adipose tissue prolongs the action of lipid-soluble benzodiazepines. The benzodiazepines are available in the following dose forms: tablets, capsules, oral solution, rectal gel, and injectable forms. The intramuscular (IM) route, for benzodiazepines other than midazolam, gives slow, erratic, and unpredictable results. In contrast, the IV route, for those available in parenteral form, produces a rapid, predictable response that makes them ideal for conscious sedation. Once a benzodiazepine is absorbed, the rate at which it crosses into the cerebrospinal fluid (CSF) through the blood-brain barrier depends on protein binding, lipid solubility, and the ionization constant of the compound. Most benzodiazepines are highly protein bound and are present in the un-ionized, lipid-soluble form. They easily cross the blood-brain and placental barriers to have effects in the CNS and on the fetus (U.S. Food and Drug Administration [FDA] categories D or X), where they can accumulate with repeated doses.
After absorption, the benzodiazepines are metabolized in the liver by either phase II metabolism or phase I followed by phase II metabolism. Phase I metabolism is decreased in the elderly, in patients taking certain drugs that inhibit hepatic metabolism, and in the presence of hepatic disease. Phase I metabolism results in active metabolites that, with repeated administration, can accumulate. Benzodiazepines that undergo only phase II metabolism are much less affected by drugs or hepatic disease. Age does not seem to affect phase II metabolism. However, one should still use caution when prescribing these drugs for elderly persons.
Mechanism of Action
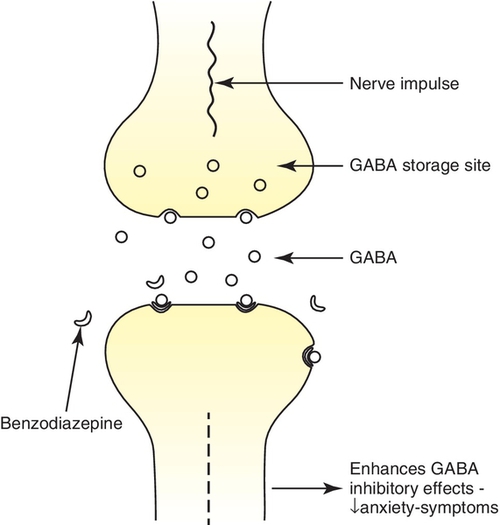
Benzodiazepines enhance or facilitate the action of the neurotransmitter γ-aminobutyric acid (GABA), a major inhibitory transmitter in the CNS (Figure 11-3). It acts at the limbic, thalamic, cortical, and hypothalamic levels of the CNS. Benzodiazepines act as agonists at the benzodiazepine receptor site, thereby reducing the symptoms of anxiety.
Pharmacologic Effects
The pharmacologic effects of the various benzodiazepines have qualitatively similar actions but vary in potency.
Behavioral Effects
The clinical effects of these agents in humans are anxiety and panic reduction at lower doses and production of drowsiness and sleep at higher doses. Repeated doses of benzodiazepines reduce rapid eye movement (REM) sleep. Usual doses cause a marked reduction in stages 3 and 4 sleep (deep sleep), which, after long-term use, can interfere with restorative sleep.
Antiseizure Effects
The benzodiazepines, such as diazepam, have antiseizure activity (i.e., they increase the seizure threshold). Diazepam, used parenterally, has been shown to be an effective antiseizure drug for the prevention of seizures associated with local anesthetic toxicity and for the treatment of status epilepticus. Clonazepam, an oral benzodiazepine, is used in combination with other antiseizure drugs to manage partial seizures. The benzodiazepines prevent the spread of seizures in tissues surrounding the anatomic seizure focus (when such a focus exists) but have little effect on the discharges at the focus itself.
Muscle Relaxation
Like all CNS depressants, benzodiazepines can produce relaxation of skeletal muscles. Some studies show benzodiazepines to be superior to other skeletal muscle relaxants for relief of musculoskeletal pain; other studies show the pain relief effect of benzodiazepines to be no better than that of aspirin or placebo. Benzodiazepines are effective for muscle spasticity secondary to pathologic states such as cerebral palsy and paraplegia.
Adverse Reactions
In general, benzodiazepines used alone have a wide margin of safety. They have similar adverse effects but differ in the frequency of these effects. Agents with long-elimination half-lives tend to accumulate and produce more side effects.
Central Nervous System Effects
The most common side effect attributed to benzodiazepines is CNS depression, manifested as fatigue, drowsiness, muscle weakness, and ataxia. These side effects are more likely to occur in elderly persons. The patient may also experience lightheadedness and dizziness. Tolerance to this effect occurs over time. Paradoxical CNS stimulation that produces talkativeness, anxiety, nightmares, tremulousness, hyperactivity, and increased muscle spasticity can occur. This reaction is more common in psychiatric patients, and benzodiazepines should be discontinued if this reaction occurs.
When benzodiazepines are used in dentistry to produce conscious sedation, the CNS depression, normally a side effect, is used as the primary effect. The amount of the benzodiazepine used to provide conscious sedation is titrated to the patient’s response. The appearance of ptosis is used as an initial endpoint for the dose administered. These agents have a rapid onset of action and an initial effect of 45 minutes to 1 hour.
Diazepam was the benzodiazepine most commonly used parenterally until newer benzodiazepines were developed. Diazepam’s long half-life and its metabolism to an active metabolite prolonged its duration of action. Its effect lasted past the dental appointment time and even into the next day.
Midazolam, a water-soluble benzodiazepine, is metabolized primarily to inactive metabolites. This feature is an advantage over diazepam for IV use in conscious sedation. Because these benzodiazepines are inactivated either directly by metabolism or indirectly by metabolism of their active metabolites, the duration and depth of sedation can be magnified by administration of drugs that inhibit the hepatic microsomal enzymes. Agents that inhibit these enzymes include cimetidine and erythromycin.
Anterograde Amnesia
It can be easily demonstrated that parenteral benzodiazepines, such as diazepam and midazolam, cause amnesia beginning when the drug is taken. This effect is used to therapeutic advantage in patients scheduled for an unpleasant dental procedure. Clinical use of several benzodiazepines has produced episodes of amnesia that can sometimes last several hours. Oral triazolam seems to have a greater likelihood to produce amnesia than other oral benzodiazepines. Patients should be warned not to sign important papers or make important decisions after benzodiazepines are administered. The mechanism of amnesia results from an impairment of consolidation processes that store the information in the brain.
Respiratory Effects
Usual doses of benzodiazepines have no adverse effect on respiration. However, doses of diazepam administered for outpatient dental procedures have been occasionally reported to cause respiratory depression. An isolated case of apnea after IV diazepam has also been observed. These respiratory effects are more common in elderly patients. The minimal respiratory depression can be exacerbated by opioids or alcohol.
Cardiovascular Effects
Therapeutic doses of benzodiazepines have no adverse effect on circulation. The relief of anxiety may result in drops in blood pressure and pulse rate. The pulse rate has also been reported to rise (tachycardia) and then return to normal after a few minutes.
Visual Effects
Benzodiazepines are contraindicated in angle-closure (narrow- angle) glaucoma and can produce other visual changes, such as diplopia, nystagmus, and blurred vision. They may be used in treatment of wide-angle glaucoma, which is the most common kind of glaucoma.
Dental Effects
The benzodiazepines have been reported to cause xerostomia, increased salivation (note that these are opposite effects), swollen tongue, and a bitter or metallic taste.
Thrombophlebitis
Parenteral diazepam can produce thrombophlebitis. Because diazepam is poorly soluble in water, the vehicle propylene glycol is used to solubilize it. The vehicle is responsible for the thrombophlebitis. The incidence is lower when the IV infusion is given in the antecubital space rather than the dorsum of the hand (more blood and faster blood flow). Because midazolam is soluble in water and propylene glycol is not used to solubilize it, it is much less likely to have this effect. With parenteral use of benzodiazepines, apnea, hypotension, bradycardia, and cardiac arrest have been reported. These are more frequent with rapid administration. Equipment for respiratory and cardiovascular assistance must be available if these agents are to be used parenterally (e.g., for conscious sedation in the dental office). Special training of the dental team administering benzodiazepines is required.
Other Effects
Benzodiazepines can affect the gastrointestinal tract, producing cramps or pain, and the genitourinary tract, causing difficulty in urination. They can also produce allergic reactions, including rash and itching.
Pregnancy and Lactation Considerations
An increased risk of congenital malformation in infants of mothers taking benzodiazepines in the first trimester has been reported. Rates of cleft lip, cleft palate, microencephaly, and gastrointestinal and cardiovascular abnormalities were greater in the group taking benzodiazepines in the study. Most of these agents are classified as FDA pregnancy category D drugs; triazolam and temazepam are in FDA pregnancy category X (see Chapter 25).
Near-term administration of benzodiazepines to the mother has resulted in floppy infant syndrome—consisting of hypoactivity, hypotonia, hypothermia, apnea, and feeding problems. Because these agents are seldom absolutely needed (except for treatment of epilepsy), they should be avoided in women who are or may become pregnant and in nursing mothers. Before a benzodiazepine is administered to a female dental patient, her pregnancy status should be determined. The first trimester, often before the patient knows that she is pregnant, is the time benzodiazepines are most likely to be teratogenic or to cause problems in the fetus.
Abuse and Tolerance
Overview
Benzodiazepines can be abused, and physical dependence and tolerance have been documented. Physiologic addiction can occur if large doses are taken over an extended period. However, their abuse and addiction potential is less than that of the other sedative-hypnotic agents such as the barbiturates.
Prolonged intake of large doses of benzodiazepines can result in a degree of CNS tolerance. Cross-tolerance also exists between the benzodiazepines and other CNS depressants. This may explain why benzodiazepines can be substituted for ethyl alcohol to relieve the symptoms of delirium tremens precipitated by acute alcohol withdrawal.
One advantage of benzodiazepines over barbiturates is the wider therapeutic index, or range of safe dose. Overdose poisoning with benzodiazepines has been rare and appears to be difficult to achieve when they are used alone, although apnea has rarely been reported. In most instances, excessively large doses must be ingested to produce respiratory or central vasomotor depression. Combining benzodiazepines with other CNS depressants can reduce their safety, so the combination can be lethal. The addition of alcohol can result in coma, respiratory depression, hypotension, or hypothermia.
Treatment of Overdose
Rarely does the ingestion of a benzodiazepine alone result in severe symptoms. Supportive therapy should be undertaken if symptoms occur. With recent ingestion, emesis may be induced. Activated charcoal and a saline cathartic may be administered. The patient’s respiration and blood pressure should be monitored.
To reverse some of the effects of a benzodiazepine, flumazenil (floo-MA-zee-nill) (Romazicon), a benzodiazepine antagonist available for IV administration, may be used. It has been shown to reverse the sedating and psychomotor effects, but its reversal of the respiratory depression produced by the benzodiazepines is incomplete. The amnesia is not consistently reversed. Flumazenil has an initial half-life of about 10 minutes and a terminal half-life of about 60 minutes. Side effects include pain at the injection site, agitation, and anxiety. The patient’s pain level does not increase as this drug takes effect. [Some patients experience increased pain with anxiety.] Some patients have been found to have been resedated before the end of 3 hours when high doses of long-acting benzodiazepines were ingested (the antagonist wore off before the agonist had been metabolized and excreted). Administering flumazenil to benzodiazepine-dependent individuals could precipitate withdrawal symptoms (like to effect of naloxone in opioid-dependent patients).
Drug Interactions
Like other antianxiety agents, benzodiazepines interact in an additive fashion with other CNS depressants, notably alcohol, barbiturates, anticonvulsants, and phenothiazines. Because diazepam and desmethyldiazepam are cytochrome P-450 2C enzyme substrates, enzyme inducers may increase their metabolism and enzyme stimulators may decrease their metabolism.
Smoking diminishes the effectiveness of the benzodiazepines. The tars produced by smoking cigarettes stimulate the hepatic microsomal enzymes in the liver. The greater number of liver enzymes raises the rate of metabolism of the benzodiazepines, so a higher dose of a benzodiazepine is required to have the same effect.
Drugs such as cimetidine, disulfiram, isoniazid, and omeprazole may increase the effects of benzodiazepines. Valproic acid may displace diazepam from binding sites, possibly resulting in an increase in sedative effects. Selective serotonin reuptake inhibitors (e.g., fluoxetine, sertraline, paroxetine) have greatly raised diazepam levels by altering its clearance. Benzodiazepines may reduce the effectiveness of levodopa, and parkinsonism has been exacerbated in patients with Parkinson’s disease. Benzodiazepines may augment the effect of digoxin, phenytoin, and probenecid.
Medical Uses
Benzodiazepines are useful in short-term treatment of anxiety, panic attacks, insomnia, and alcohol withdrawal. They are used for the acute treatment of seizures. Some neuromuscular diseases can be treated with the benzodiazepines. These agents are also used in conscious sedation, in general anesthesia, and during surgery.
Anxiety Control
Generalized anxiety disorder and panic disorder are common indications for use of benzodiazepines in general medicine. Anxiety produces a physiologic response resembling fear, with manifestations including restlessness, tension, tachycardia, and dyspnea. Most well-controlled clinical trials have shown that the antianxiety effects of benzodiazepines is better than those of placebo, barbiturates, and meprobamate. Benzodiazepines also cause less sedation than the classic sedative-hypnotic agents.
Conscious Sedation
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


