Distraction osteogenesis is an alternative treatment option for patients with facial asymmetry and mandibular hypoplasia. New bone is formed between bone segment surfaces that are gradually separated by incremental traction. The purpose of this article is to report the treatment of a 22-year-old man with hemifacial microsomia, facial asymmetry, and a skeletal Class II profile. The patient’s left mandibular ramus was lengthened with distraction osteogenesis, and miniscrew-assisted rapid palatal expansion was used to correct the maxillary transverse deficiency. Postoperative orthodontic treatment achieved tooth alignment and closure of the posterior open bite. The total treatment period was 27 months. These therapeutic treatments improved the patient’s facial appearance.
Hemifacial microsomia is the second most frequent form of isolated facial birth disorder, after cleft lip and palate. Hemifacial microsomia is a congenital skeletal malformation in which there is a deficiency on 1 side of the face; characteristic features include maxillomandibular hypoplasia and facial asymmetry. It is primarily a syndrome of the first brachial arch, involving underdevelopment of the ear, mandible, maxilla, zygoma, temporal bone, and the associated musculature and soft tissues. The exact etiology of hemifacial microsomia has not yet been determined, but laboratory studies suggest that the clinical features might be caused by early loss of neural crest cell-related formation of the first brachial arch.
In adults with hemifacial microsomia, mild skeletal deformities—such as mandibular hypoplasia and facial asymmetry—have traditionally been treated with bimaxillary surgery, whereas autogenous costochondral grafting is used for more severe malformations. In 1988, Ilizarov first described distraction osteogenesis, an alternative treatment process in which new bone is formed between bone segment surfaces that are gradually separated by incremental traction. In 1992, McCarthy et al used mandibular lengthening by distraction osteogenesis in patients with hemifacial microsomia. Because of the slow lengthening procedure, the soft tissues adapt gradually; this is advantageous because it minimizes the risk of relapse for hemifacial microsomia patients who lack both bone and soft tissues.
In this case report, we describe the treatment with the combination of distraction osteogenesis and orthodontics, as well as miniscrew-assisted rapid palatal expansion, for a man with a skeletal Class II malocclusion, hemifacial microsomia, and a maxillary transverse deficiency.
Diagnosis and etiology
A 22-year-old man visited the orthodontic department at Yonsei University Dental Hospital in Seoul, Korea, with a chief complaint of facial asymmetry. The clinical and radiographic examination results indicated that he had Pruzansky-Kaban type I left hemifacial microsomia with well-formed but small temporomandibular joint and ramus. His medical history included a right orbital wall fracture 3 years previously and removal of a skin tag on his left ear during childhood. He had no family history of craniofacial deformities and no temporomandibular joint-related symptoms.
The pretreatment facial photographs showed that his face was asymmetrical with a mildly underdeveloped left side, a chin point that was deviated 8.0 mm toward the affected side, and a retrusive chin in profile view, in addition to lip canting and incompetence. There was no significant difference between the levels of his right and left eyes. The intraoral examination showed frontal canting of the occlusal plane and a mandibular midline deviation of 2.0 mm to the left. He had severe Class II canine and molar relationships, with an 11.0-mm overjet, a 3.0-mm overbite, and a transverse deficiency with a narrow V-shaped maxillary arch ( Figs 1 and 2 ).
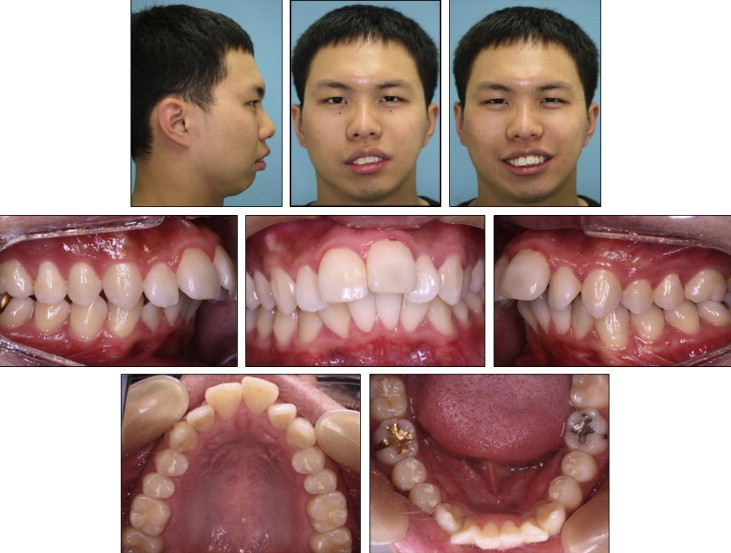
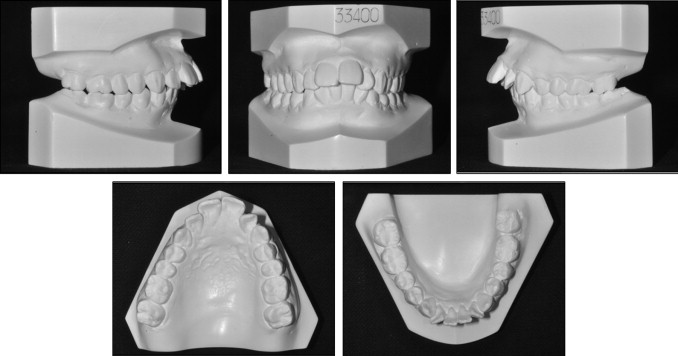
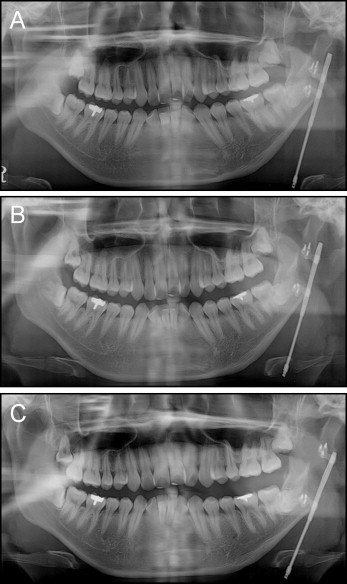
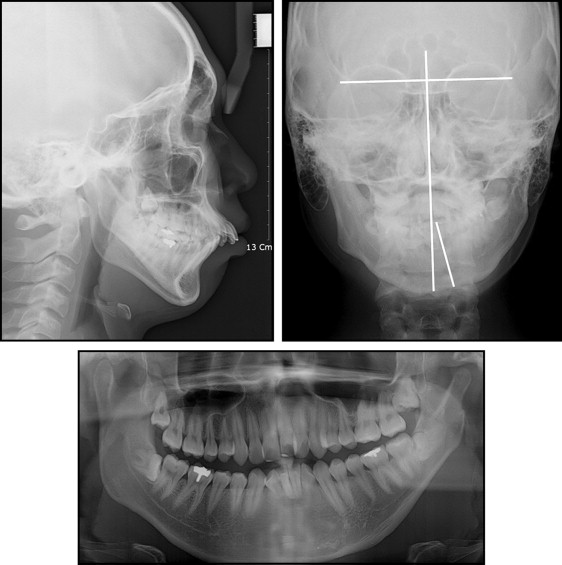
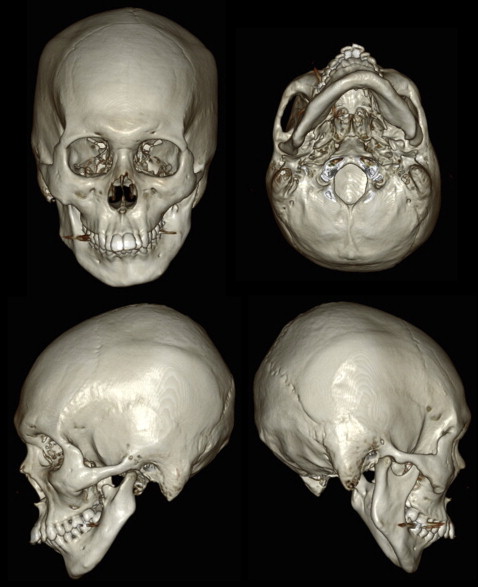
The lateral cephalometric analysis showed an SNA angle of 82.2°, an SNB angle of 75.0°, and an ANB angle of 7.2°. The mandibular plane angle was 47.6°, and the ramus height was 45.4 mm ( Fig 3 , Table I ). The maxillary incisors were labially inclined at an angle of 120.6° to the SN plane. The upper and lower lips were protrusive with respect to the E-line. The posteroanterior cephalometric analysis showed that the maxillary molars were extruded by 3.1 mm more on the right side compared with the left, and the chin was deviated by 12.0 mm to the left. The panoramic radiograph showed differences in the sizes of the ramus, condyle, and coronoid between the left and right sides as well as impaction of all 4 third molars with complete root formation. Clinically, the patient’s periodontal tissues were healthy. Three-dimensional computed tomography images showed deficiencies of the left condylar and coronoid processes, along with ramus hypoplasia and chin deviation. The angle of the mandible was also underdeveloped ( Fig 4 ).
| Measurement | Norm | Pretreatment (22 y 3 mo) | Postdistraction (22 y 10 mo) | Posttreatment (24 y 6 mo) |
|---|---|---|---|---|
| Skeletal | ||||
| SNA (°) | 82.4 ± 3.2 | 82.2 | 82.4 | 83.6 |
| SNB (°) | 80.4 ± 3.1 | 75 | 80.1 | 79.3 |
| ANB (°) | 2.0 ± 1.7 | 7.2 | 2.3 | 4.3 |
| SN-GoGn (°) | 32.0 ± 5.0 | 47.6 | 41.9 | 42.1 |
| Gonial angle (°) | 117.1 ± 6.7 | 139.5 | 138.6 | 134.9 |
| Ramus height (mm) | 57.6 ± 5.2 | 45.4 | 54.5 | 53 |
| Go-Me (mm) | 79.0 ± 5.0 | 72.6 | 76.6 | 75.9 |
| Dental | ||||
| U1-SN (°) | 107.0 ± 5.0 | 120.6 | 121.8 | 113.6 |
| U1-NA (°/mm) | 25.0/7.0 | 38.3/13 | 39.4/13 | 30/8.9 |
| L1-NB (°/mm) | 27.0/6.9 | 36.6/12.6 | 34.2/11.9 | 37.4/12.3 |
| L1-GoGn (°) | 95.0 ± 5.0 | 94 | 92.2 | 96 |
| Soft tissues | ||||
| E-line (mm) | 1.0 ± 2.0 | 6.3 | 2.1 | 2 |
| Upper lip/lower lip | 2.0 ± 3.0 | 9.8 | 6.1 | 6.7 |
Treatment objectives
Because of the mild Pruzansky-Kaban type I hemifacial microsomia on the left side, the patient expressed concern about his facial asymmetry. Thus, the treatment objectives were established as follows: (1) correct the patient’s facial asymmetry by lengthening the affected ramus, and coordinate the facial, maxillary, and mandibular dental midlines; (2) correct the skeletal Class II anteroposterior jaw relationship; (3) coordinate the widths of the dental arches; (4) correct the canted occlusal plane and achieve dental Class I canine and molar relationships; and (5) relieve the proclined incisor position and achieve an ideal overjet and overbite relationship.
Treatment objectives
Because of the mild Pruzansky-Kaban type I hemifacial microsomia on the left side, the patient expressed concern about his facial asymmetry. Thus, the treatment objectives were established as follows: (1) correct the patient’s facial asymmetry by lengthening the affected ramus, and coordinate the facial, maxillary, and mandibular dental midlines; (2) correct the skeletal Class II anteroposterior jaw relationship; (3) coordinate the widths of the dental arches; (4) correct the canted occlusal plane and achieve dental Class I canine and molar relationships; and (5) relieve the proclined incisor position and achieve an ideal overjet and overbite relationship.
Treatment alternatives
Based on the treatment objectives, the following treatment alternatives were considered: (1) maxillary and mandibular orthognathic surgery with anteroposterior impaction, with or without segmental surgeries; (2) maxillary orthognathic surgery with anteroposterior impaction, with or without segmental surgeries, and distraction osteogenesis to advance the mandibular body and lengthen the shorter ramus; (3) an iliac bone graft to level the canting of the maxillary left side, and distraction osteogenesis to advance the mandibular body and lengthen the shorter ramus; or (4) combined orthodontic treatment, with or without extraction of the 4 first premolars, and distraction osteogenesis.
The patient did not want to undergo orthognathic surgery and wanted minimal surgeries and bone grafting. He did not agree to extraction of the 4 first premolars because he was not concerned about lip protrusion. Therefore, the fourth option without extractions was chosen.
Treatment progress
The treatment plan was to correct the mandibular asymmetry and the occlusal plane canting by distraction osteogenesis of the ramus on the affected side, followed by orthodontic treatment to align the teeth and establish a functional occlusion. The patient was hospitalized, and surgery for the distraction osteogenesis was performed under general nasotracheal anesthesia. Through an intraoral incision, a horizontal ramus osteotomy was performed on the left at the level of the occlusal plane. The distractor was placed with a vector parallel to the posterior border of the ramus. After 7 days of latency, the distraction device was activated by 1 mm per day for 24 days, until the mandibular midline deviation was overcorrected by up to one third of the initial discrepancy. The distraction device was maintained for 90 days ( Fig 5 ). In the consolidation phase, a resin occlusal bite-block was placed on each arch because of a surgically created posterior unilateral open bite on the elongated side. At the end of this consolidation phase, the patient had a posterior open bite and a crossbite on both sides ( Figs 6-8 ).