A
Abscess Pathologic process that is an enclosed collection of purulent exudates (pus) in tissues, organs, or confined spaces in the body. Signs of infection, swelling, and inflammation are typical. See also: Acute abscess; Chronic abscess; Gingival abscess; Periodontal abscess; Residual abscess.
Absorbable See: Bioabsorbable material.
Absorption Uptake of substances into or across tissues (eg, skin, mucosa, intestine, or renal tubules).
Abutment Tooth, tooth root, or implant component that serves as support and/or retention for a dental prosthesis.1 See also: Anatomic healing abutment; Angled/angulated abutment; CAD/CAM abutment; Castable abutment; Ceramic abutment; Healing abutment; Nonangled abutment; Nonrotating abutment; Prefabricated abutment; Preparable abutment; Standard abutment; Temporary abutment; Transmucosal abutment; UCLA abutment.
Screw design of a. Prosthetic implant component manufactured with threads at the apical portion of the element. This term refers to the manufacture of a specific thread pattern unique to a particular implant company.
Tightness of a. Amount of clamping force present within the body of an abutment screw following placement. See also: Preload.
Abutment clamp Instrument used to handle or hold the implant abutment. The concave design is such that when engaged, the clamp fits circumferentially around the component.
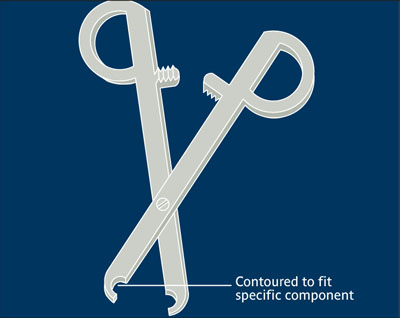
Abutment clamp.
Abutment connection Act of connecting an abutment to an endosseous implant.2,3 See also: External abutment connection; Internal abutment connection; Morse taper connection.
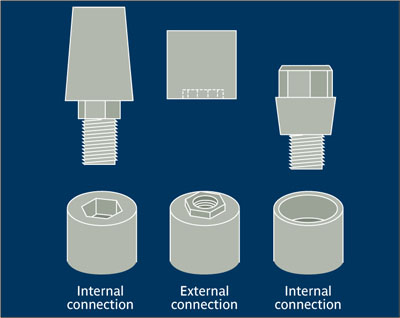
Abutment connection.
(Redrawn from Yanase and Preston2 with perission.)
Abutment-implant interface Common contact surface area between an implant abutment and the supporting implant.3
Abutment screw Single-piece implant component with a threaded apical portion that can be connected directly to the implant. No additional screw is required to connect and secure the abutment component.
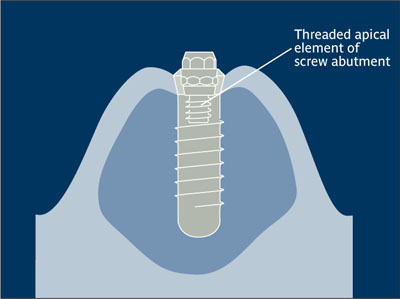
Abutment screw.
Access hole Opening in a replacement tooth’s occlusal or lingual surface of an implant-retained prosthesis that provides entrance for abutment or prosthesis screw placement or removal.3

Access hole.
(Reprinted from Watzek4 with permission.)
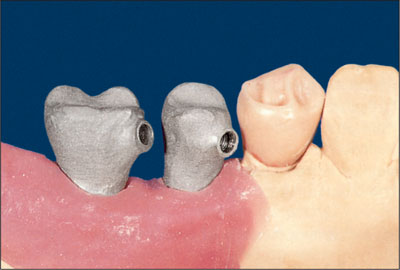
Access hole.
(Reprinted from Watzek4 with permission.)
Acellular Limited in or devoid of cells.
Acellular dermal allograft Skin graft made of a thin split-thickness of dermis that has undergone a tissue-preparation process to remove cellular material.
Acid-etched implant External surface of an implant body that has been modified by the chemical action of an acidic medium. The subtractive surface is intended to enhance osseointegration.
Acid etching Act of modifying an implant surface by exposure to an acidic medium with the intention of enhancing osseointegration. See also: Etching.
Acquired immunity Specialized form of immunity involving antibodies and lymphocytes. Active immunity develops after exposure to a suitable agent (eg, by an attack of a disease or by injection of antigens), and passive immunity occurs with transfer of antibodies or lymphocytes from an immune donor.
Acquired immunodeficiency syndrome See: AIDS.
Acrylic crown See: Acrylic restoration.
Acrylic resin Thermoplastic resin produced by polymerizing esters of acrylic or methyl-methacrylate acids.
Acrylic restoration Tooth or other prosthetic restoration fabricated from acrylic resin, such as an acrylic crown.
Actinobacillus actinomycetemcomitans Gram-negative, fermentative, nonmotile, coccoid or rod-shaped bacterium of the family Pasteurellaceae, part of the normal mammalian microflora. This bacterium has been associated with periodontal infections and, in particular, early-onset, aggressive forms of periodontal disease.
Acute abscess Abscess of relatively short duration, typically producing local swelling, inflammation, and pain.
Acute infection Infection with a rapid onset and usually a severe course.5 See also: Infection.
Additive surface treatment Implant surface modification created by the addition of material. Surface modification may also be accomplished by subtractive surface treatment. Compare: Substracted implant surface.
Adhesive Intervening substance used to unite adjoining surfaces. In maxillofacial prosthetics, adhesives have been used for border adaptation, marginal seal, and the retention of facial, auricular, nasal, or orbital prostheses. Systems commonly used include biphase adhesive tape and medical-grade adhesives.6,7
Adhesive retention See: Cementation.
Adjunctive treatment Supplementary therapeutic procedure to augment a main therapeutic procedure in an additive, usually incremental, manner.
Adjustable attachment system Stud-shaped attachment in which the stud (easily replaced) serves as the patrix, and the matrix consists of a metal housing. The base of the patrix can be cast-to or soldered as part of a coping, and the matrix can be incorporated into the dental prosthesis. The patrix is adjustable using a special tool to modify the spread of the patrix width.8,9
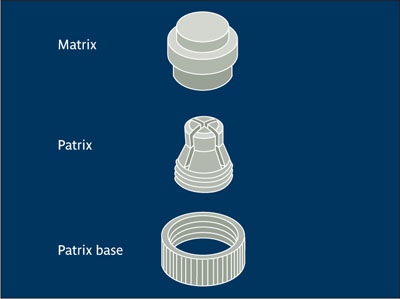
Adjustable attachment system.
(Redrawn from Staubli and Bagley9 with permission.)
Adjustment Modification of a tooth or prosthetic restoration to improve its appearance, fit, or function.10
AIDS Acronym for acquired immunodeficiency syndrome, caused by HIV (human immunodeficiency virus), that leaves the body vulnerable to a host of life-threatening illnesses. There is no cure for AIDS, but treatment with antiviral medication can suppress symptoms. The virus attacks selected cells of the immune, nervous, and other systems, impairing their proper function and rendering the subject highly vulnerable to life-threatening conditions (eg, Pneumocystis carinii pneumonia) and those that can become life threatening (eg, Kaposi sarcoma). Oral lesions may include necrotizing ulcerative gingivitis (NUG), necrotized ulcerative periodontitis (NUP), linear gingival erythema (LGE), candidiasis, hairy leukoplakia, herpes simplex, and rapidly progressive periodontitis.
Alendronate sodium Oral bisphosphonate used in the treatment of different types of osteoporosis with a reasonably high degree of treatment success in prevention of fractures of the vertebral column.
Algae See: Calcified algae.
Algipore See: Calcified algae; Porous marine-derived coralline hydroxyapatite.
Alkaline phosphatase Enzyme found in high concentrations in osteoblasts; commonly located on cytoplasmic processes extending into the osteoid. The level of alkaline phosphatase in serum is a systemic indicator for bone formation.
Allodynia Pain resulting from a nonnoxious stimulus that does not normally provoke pain.
Allogeneic bone graft Graft between genetically dissimilar members of the same species. Iliac cancellous bone and marrow, freeze-dried bone allograft (FDBA), and demineralized freeze-dried bone allograft (DFDBA) are available commercially from tissue banks. Called also allograft.
Allograft Graft between genetically dissimilar members of the same species.11,12 See also: Acellular dermal allograft; Allogeneic bone graft; Soft tissue augmentation.
Integration with a. Independent of allograft or bone substitute use for osseous reconstruction, implants will always have newly formed host bone in juxtaposition to the implants as part of the process of osseointegration.
Alloplast Inorganic, synthetic, or inert foreign material implanted into tissue.11,12
Alloplastic graft Graft material such as hydroxyapatite (HA), tricalcium phosphate (TCP), polymethylmethacrylate (PMMA) and hydroxyethyl-methacrylate (HEMA) polymer, or bioactive glass that is derived either synthetically or from a foreign, inert source. See also: Alloplast.
Aluminum oxide Oxide ceramic (Al2O3) used in single-crystal form as implant material. Because it is biocompatible and has a hardness similar to that of the gem sapphire, it has been called single-crystal sapphire. Aluminum oxide has been replaced by titanium as the material of choice for implants.
Alveolar Related to the alveolar process, the maxillary or mandibular ridge of bone that supports the roots of teeth.
Alveolar atrophy Decrease in the volume of the alveolar process occurring after tooth loss, decreased function, and/or localized overloading from an improperly fitting removable partial or complete denture.13
Alveolar bone That part of the maxilla or mandible comprising the tooth-bearing and/or supporting part of the jawbones. It consists of cortical plates, the vestibular plate being the thinnest, and trabecular bone. See also: Atrophic alveolar bone; Cancellous bone.
Quality of a. b. Of major importance to the outcome of implant placement, bone quality has been categorized in a number of classification systems, illustrating the variance in relative volume of compact cortical bone and trabecular bone. Although it is often used, the term bone quality is a misnomer; a more correct term would be bone density. A popular and often-quoted classification was originally proposed by Lekholm and Zarb (1985). Type 1 refers to homogenous compact bone of high density but low vascularity; hence not an ideal clinical situation. Types 2 and 3 describe bone that still has a dense cortical plate but also has a cancellous portion with good vascularity for ideal implant placement and stability. Type 4 describes inadequate density, and caution in its use for implant placement is warranted.14
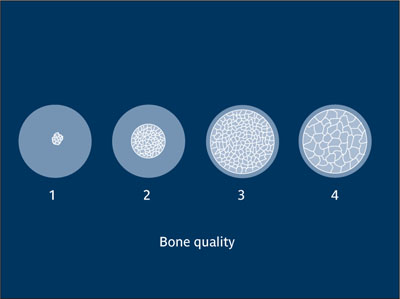
Quality of alveolar bone.
(Redrawn from Lekholm and Zarb14 with permission.)
Quantity of a. b. Of major importance to the outcome of implant placement, bone volume at a given implant site ideally should be at least 10 mm in vertical dimension and 6 mm in horizontal dimension.15
Alveolar distraction osteogenesis Augmentation procedure involving the surgical mobilization, transport, and fixation of an alveolar bone segment. A mechanical distraction device allows a gradual, controlled displacement of the mobile bone segment at an ideal rate of 0.4 mm a day. Following the desired augmentation, the device is left in place for 3 to 4 weeks for consolidation of the newly formed bone.16 See also: Distraction osteogenesis (DO).
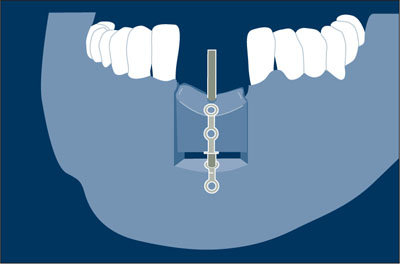
Alveolar distraction osteogenesis.
(Redrawn from Chin16 with permission.)
Alveolar mucosa Mucosa covering the basal part of the alveolar process and continuing into the vestibulum and floor of the mouth without demarcation. In contrast to attached gingiva, alveolar mucosa is nonkeratinized, mobile, and has a thin lamina propria, numerous elastic fibers, and a distinct submucosa. It is a dark red tissue, movable, and loosely attached to the periosteum. The alveolar mucosa is coronally separated from the gingiva by a line called the mucogingival junction.
Alveolar nerve Either of the superior alveolar nerve branches of the maxillary nerve of the second division of the trigeminal nerve (rami alveolares superiores posteriores, ramus alveolaris superior medius, and ramus alveolaris superior anteriores
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


