Chapter 9
Treatment of an Edentulous Patient with an Accelerated Treatment Protocol and Immediate Occlusal Loading Protocol (All-on-4™)
LITERATURE REVIEW
The concept of osseointegration was originally designed for edentulous patients, specifically those patients with edentulous mandibles who were experiencing difficulties managing mandibular complete dentures (Lindquist et al. 1996). The initial protocol originally yielded high implant cumulative survival rates (CSRs) with two-stage surgical protocols where implants were placed and soft tissues were closed over the implants; implants were not exposed to the oral cavity during initial healing (Brånemark et al. 1977). Four to six months of unloaded healing was initially mandated for osseointegration prior to a second surgical procedure scheduled to uncover the implants, place transmucosal abutments, and begin prosthetic procedures. Unfortunately, these patients generally had to continue wearing ill-fitting dentures during this entire time. The apparent contradiction with this scenario was that patients generally scheduled this type of treatment because of difficulties managing their mandibular dentures, yet they did not receive the fixed implant prostheses until 9–12 months after implant placement.
There are a significant number of literature citations that have demonstrated high survival rates for implants placed with high primary stability into the parasymphysis regions of edentulous mandibles, splinted together with rigid interim prostheses, and placed into immediate functional occlusion (Schnitman et al. 1997; Tarnow et al. 1997; Jaffin et al. 2000; Grunder 2001; Strietzel et al. 2011). This modality may also be considered for partially edentulous patients with severe periodontal disease (Cooper et al. 2002). Cooper and others demonstrated a 6- to 18-month postimplant placement CSR of 100% for mandibular implants placed with high primary stability, immediately post extraction of periodontally compromised teeth; rigidly splinted together with acrylic resin prostheses; and placed into fully functional occlusion.
Buser et al. (1997) and Cochran et al. (2002) considered implants to be successful if they satisfied the following criteria:
- Absence of pain or any negative subjective sensation
- Absence of clinical detectable implant mobility
- Absence of any recurrent peri-implant mucositis and/or peri-implantitis accompanied by swelling, redness, or pain of the peri-implant mucosa
- Absence of continuous peri-implant radiolucency
- Absence of mesial and/or distal vertical bone loss of more than 30% of the endosseous part of the implants
- No need to repair or replace the implant-supported prosthesis
- Subjective evaluation of the treatment outcomes
Traditional implant treatment plans typically called for a significant number of implants to be placed vertically throughout an edentulous jaw (Block and Winder 1991). However, posterior maxillae and mandibles have several anatomic limitations with this approach: the mandibular inferior alveolar canal and associated structures may limit the amount of bone available for vertical implant placement. Vertical and buccal/lingual resorption of posterior edentulous mandibular ridges may also prevent placement of dental implants distal to the mental foramina. In posterior maxillae, it is not uncommon to see vertical resorption of alveolar bone and/or enlargement of the maxillary sinuses that preclude vertical implant placement (Krekmanov et al. 2000).
Multiple authors have reported on the average number of implants required for implant prostheses (Del Fabbro et al. 2006; Strietzel et al. 2011). Strietzel et al. (2011) reported that the median number of implants in their retrospective chart review for maxillary fixed implant prostheses was 9 (SD 1.6, range 6–12). Mandibular fixed prostheses averaged 8 implants per patient (SD 1.4, range 6–10). Del Fabbro et al. (2006) reported similar findings. Capelli et al. (2007) reported the results of immediate occlusal loading (IOL) in maxillary and mandibular jaws: implant CSR was 97.6% for up to 40 months post loading; prosthesis CSR was 100%. They concluded that their preliminary results suggested that immediate rehabilitation of edentulous maxillae and mandibles with hybrid prostheses supported by six or four implants, respectively, may represent a viable treatment alternative with respect to more demanding surgical procedures, such as grafting. Their clinical results indicated that immediately loaded tilted implants achieved the same outcome as upright implants in both jaws.
Agliardi et al. (2010) reported on the results of a clinical study that included 173 edentulous patients, followed for up to 59 months. Four implants, two tilted and two vertical, were placed according to a specific protocol (All-on-4™ (AO4), Nobel Biocare, Yorba Linda, CA, USA). Provisional, all-acrylic resin prostheses were inserted on the same day as implant placement. Definitive prostheses were inserted 4–6 months later. A total of 154 immediately loaded prostheses (61 maxillary, 93 mandibular) were in function for at least 1 year and were included in the analysis. Four vertical maxillary and one tilted mandibular implant failed within 6 months of occlusal loading. No further implant failures were noted. The 1-year maxillary implant CSR was 98.4% and 99.7% for mandibular implants. Agliardi et al. (2010) concluded that their preliminary results from this relatively large number of implants and patients suggested that the AO4 protocol can be considered to be a viable treatment option for immediate rehabilitation of maxillae and mandibles.
The preceding reports consistently reported clinical results associated with interim, acrylic resin, and immediate prostheses. Definitive prostheses were generally fabricated 3–6 months post occlusal loading. This treatment approach necessitated fabrication of two prostheses: interim, acrylic resin prostheses fabricated and inserted within 1–2 days of implant placement and definitive prostheses fabricated with metal frameworks approximately 3–6 months post implant placement and occlusal loading. There are also protocols that have been developed that provide patients with definitive cast metal frameworks/hybrid prostheses (Tames et al. 2004; Tealdo et al. 2011). These protocols involve slightly more coordination among the surgical, prosthetic, and laboratory teams but have proved to be a viable alternative to previous protocols that include interim and definitive prostheses.
Tealdo et al. (2011) compared implant survival rates and radiographic outcomes of immediate and delayed implant loading in edentulous maxillae. They reported on the results of a clinical study where 49 patients in need of maxillary full-arch treatment were randomized into two groups: test group (n = 34) treated following the Columbus Bridge Protocol with four to six implants loaded within 24 hours and a control group (n = 15) treated following the ad modum Brånemark protocol with six to nine implants loaded a mean 8.75 months after surgery. Two hundred sixty implants (test: n = 163, control: n = 97) were placed; subjects were treated with immediate screw-retained full-arch prostheses within 1 day of implant placement. Bone levels were measured at baseline and at 1, 2, and 3 years; bone levels were analyzed using repeated-measures analysis of variance. Tealdo and others reported that all patients appeared for all of the scheduled recall visits. No differences in CSRs were found between groups at 36 months. Ten implants (6.1%) failed in the test group; four implants (4.1%) failed in the control group. At 36 months, no prosthetic failures were detected. Significantly less bone loss was found, at all-time intervals, in the test group (P < 0.001). Average bone levels from the implant/abutment connections was 1.3 mm in the test group and 1.9 mm in the control group at 12 months, 1.5 and 2.2 mm at 24 months, and 1.6 and 2.3 mm at 36 months, respectively. Tealdo et al. (2011) concluded that the Columbus Bridge Protocol involving immediate loading of maxillary implants placed into both healed and fresh extraction sites exhibited equivalent implant survival and less marginal bone loss at 3 years when compared to the conventional two-stage delayed loading protocol.
The AO4 concept was designed to use posterior tilted implants and anterior vertical implants to create full-arch, screw-retained prostheses (Figures 9.1). This protocol may be less clinically invasive for patients as it precludes the need for grafting in the posterior segments of either jaw (Figures 9.2). The concept was initially proposed in a publication as treatment for patients with mandibular dental disease because IOL had proven to be successful in patients with edentulous mandibles (Schnitman et al. 1997; Tarnow et al. 1997; Cooper et al. 2002). The protocol included placement of four implants (two posterior tilted, two anterior straight) placed with high insertion torque and splinted together with fixed, screw-retained prostheses (Malo et al. 2003). All implant apices were placed such that they engaged cortical bone anterior to the mental foramina. The tilted implant design generally resulted in an increased anterior/posterior (A/P) spread for the implants and restorations and typically provided first molar occlusion for patients with short cantilevered segments (Figures 9.3). Positive results for long-term implant survival with the AO4 protocol have been reported by numerous authors (Capelli et al. 2007; Crespi et al. 2012; Weinstein et al. 2012).
Figure 9.1 Panoramic radiograph of a patient treated with the AO4 protocol. Note the tilted distal implants inboth jaws and the relatively vertical anterior implants in both jaws.
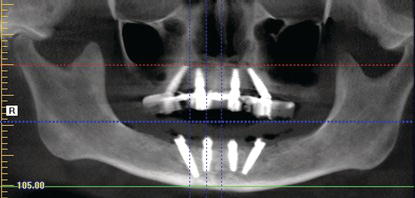
Figure 9.2 Panoramic radiograph of a patient with significant maxillary posterior resorption and large, pneumatized maxillary sinuses.
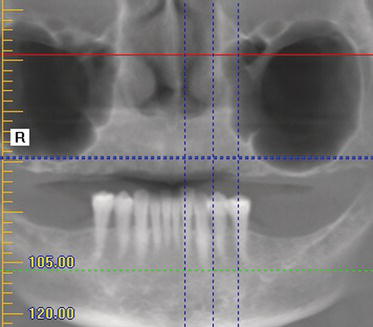
Figure 9.3 Occlusal image of a maxillary prosthesis fabricated per the AO4 protocol. Note the size of the A/P spread and the inclusion of first molars bilaterally within the prosthesis.

CLINICAL CASE PRESENTATION
This patient was 55 years old when she presented to the author.
Appointments 1 and 2: Initial Examination, Articulator Mounting, and Wax Try-In
Chief Complaint
“I have a bunch of loose teeth. I can’t eat and won’t smile.”
History of the Present Illness
This patient had been losing multiple teeth over the past several years – some of which actually simply fell out of her mouth. At one time, she did have removable partial dentures (RPDs) fabricated, but she could no longer wear them due to dental discomfort. She also did not want to wear any type of dentures. At the time of her first clinical visit, she was in no acute distress. She was a registered nurse in a cardiac care unit in a local teaching hospital.
Radiographs (CT Scan)
At the author’s practice, all patients receive a complimentary computed tomography (CT) scan. The benefits and limitations of CT scans have already been covered in Chapter 3; they will not be repeated here. Selected images from the patient’s preoperative CT scan can be seen in Figures 9.4–9.14.
Figure 9.4 Panoramic view from the preoperative CT scan. Note the significant amount of periodontal bone loss around the remaining teeth, the pneumatization of both maxillary sinuses, and the relatively high location of the inferior alveolar canals.

Figure 9.5 Panoramic view from the preoperative CT scan with the maxillae in focus. The diagnostic slices will be taken from this maxillary image.
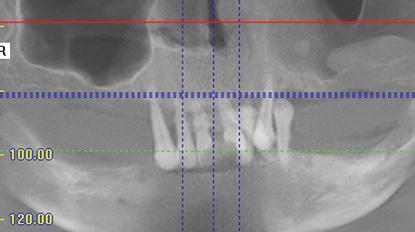
Figure 9.6 Panoramic view from the preoperative CT scan with the mandible in focus. The diagnostic slices will be taken from this mandibular image.
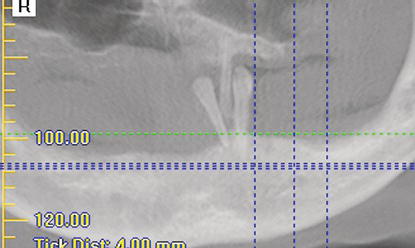
Figure 9.7 This slice identified the location of the anterior portion of the right maxillary sinus. There was adequate bone volume for implant placement.
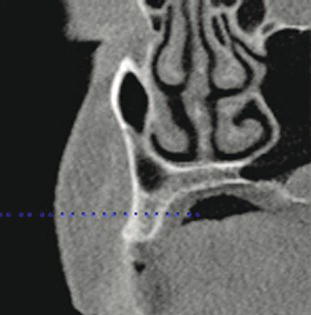
Figure 9.8 This slice identified the amount of bone available in the right anterior maxilla. There was adequate bone volume for implant placement.

Figure 9.9 This slice identified the amount of bone available in the left anterior maxilla. There was adequate bone volume for implant placement.

Physical Examination
This patient presented with partially edentulous maxillae and a partially edentulous mandible. The maxillary teeth were lost prior to treatment (Figures 9.15–9.19). The posterior edentulous maxillary ridge was broad and U shaped. Buccal vestibules were within normal limits. No soft tissue pathology was noted. She also had adequate saliva.
Figure 9.10 This slice identified the location of the anterior location of the left maxillary sinus. There was adequate bone volume for implant placement.

Figure 9.11 This slice identified the location of the right mental foramen. The tilted implant was to be placed such that the osteotomy was approximately 4 mm superior to the occlusal aspect of the foramen.
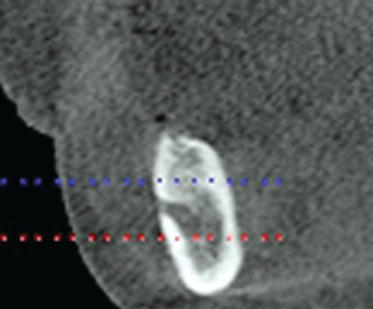
Figure 9.12 This slice identified the potential location of the right vertical implant. There was adequate bone volume for implant placement.
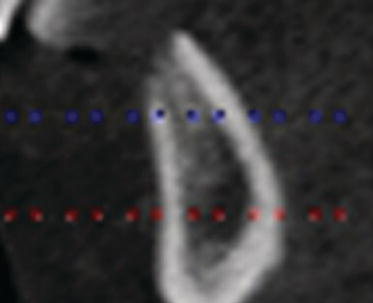
Figure 9.13 This slice identified the potential location of the left vertical implant. There was adequate bone volume for implant placement.
Diagnostic Casts, Articulator Mounting, and Diagnostic Wax Try-In
Due to the fact that the patient had not been wearing her maxillary complete denture and that she had specific aesthetic concerns relative to maxillary tooth location and arrangements, it was decided to proceed with preliminary impressions, diagnostic casts, and an articulator mounting (Figures 9.20 and 9.21). A maxillary record base with occlusion rim was fabricated on the maxillary diagnostic cast, and the articulator mounting would be made at a tentative vertical dimension of occlusion (VDO). The patient would then be able to evaluate the planned aesthetic results, and the author could evaluate the interocclusal space at the tentative VDO and the location of the teeth. Knowledge of accurate tooth locations is essential when treatment planning cases with implant surgeons. Teeth shade and molds were also selected at the initial jaw relation records visit. An initial determination of the VDO, incisal edge position, location of the incisal/occlusal plane, and lip support was made; the casts were mounted on an average value articulator (Stratos 100, Ivoclar Vivadent AG, Liechtenstein) (Figures 9.22). Denture teeth were set in a Class I relationship with the mandibular teeth, and the wax denture was tried in (Figures 9.23). The centric jaw relationships were verified as accurate; the patient had a thorough chance to evaluate the aesthetic arrangement of the maxillary teeth, lip support, and incisal display during speaking, smiling, and at rest. The patient approved the arrangement of the teeth in the wax denture.
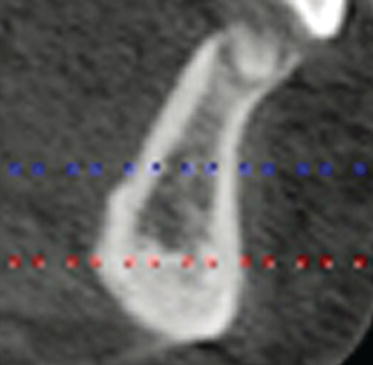
Figure 9.14 This slice identified the location of the left mental foramen. The tilted implant was to be placed such that the osteotomy was approximately 4 mm superior to the occlusal aspect of the foramen.
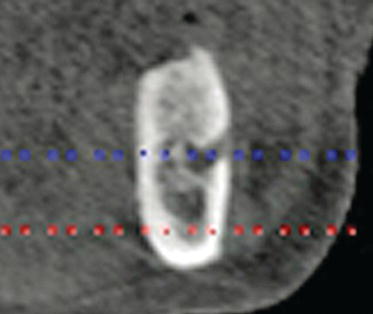
Figure 9.15 Clinical, preoperative full-face image with the patient at the vertical dimension of rest position. Note the lack of lip support, as the patient was not wearing her maxillary complete denture.

Figure 9.16 Clinical, preoperative lower midface image. The patient was asked to open her mouth and close until her lips met. This was considered to be the vertical dimension of rest position.

Figure 9.17 Clinical, preoperative, intraoral image. There was minimal A/P resorption of the edentulous maxillae; the maxillae were in a Class I skeletal relationship with the mandible and mandibular teeth.

Figure 9.18 Clinical, preoperative, intraoral image of the edentulous maxillae. The posterior edentulous ridges appeared to be quite broad; the alveolar ridges were actually quite resorbed buccally/lingually. She did not have enough bone volume for vertical, posterior implant placement.

Figure 9.19 Clinical, preoperative, intraoral preoperative image of the partially edentulous mandible and mandibular teeth. Note the heavy accumulations of supragingival calculus.

Figure 9.20 Laboratory occlusal image of the edentulous maxillary diagnostic cast.
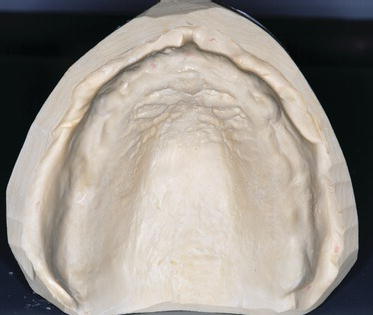
Figure 9.21 Laboratory facial image of the mandibular partially edentulous diagnostic cast.

Figure 9.22 Laboratory facial image of the mounted diagnostic casts with the maxillary occlusion rim and record base in place. This articulator mounting represented the tentative VDO.

Figure 9.23 Clinical image of the patient smiling, with the maxillary wax denture in place. The patient liked the aesthetic arrangement of the maxillary denture teeth, lip support, and incisal display during speaking, smiling, and at rest. This wax denture would be processed into the interim maxillary implant-retained prosthesis.

Diagnosis
After a careful evaluation of the CT scan, physical findings, articulator mounting, and wax denture, the following diagnoses were made:
Assessment
The patient desired fixed, nonremovable prostheses in both jaws. She did not want to undergo periodontal surgery as she had done that in the past and had no long-term success along with, significant surgical morbidity. Shanbhaq et al. (2012) reported on the results of a study that evaluated the impact of periodontal therapy on oral health-related quality of life in adults. They concluded that routine, nonsurgical therapy moderately improved the oral health-related quality of life in adults with periodontal disease. Genco and Borgnakke (2013) identified numerous risk factors associated with periodontal disease that included lifestyle factors, such as smoking and alcohol consumption. They also included diseases and unhealthy conditions such as diabetes mellitus, obesity, metabolic syndrome, osteoporosis, and low dietary calcium and vitamin D. Genco and Borgnakke (2013) noted that these risk factors could be modified by patients, and the management of risk factors was a major component of contemporary periodontal care of many periodontal patients. They also noted that genetic factors also had a role in periodontal disease and allowed dental professionals to target individuals for prevention and early detection. They also stated that the role of genetic factors in aggressive periodontitis was also clear. However, they also advised that although genetic factors (i.e., specific genes) have been strongly suspected to have an association with chronic adult periodontitis, there was yet no clear evidence for this in the general population. Genco and Borgnakke also stated that it was important to pursue efforts that identified genetic factors associated with chronic periodontitis because such factors have the potential to identify patients susceptible for development of this disease. Many of the systemic risk factors for periodontal disease, such as smoking, diabetes and obesity, and osteoporosis in postmenopausal women, are relatively common and can be expected to affect a significant number of patients with periodontal disease. Hence, risk factor identification and management has become a key component of care for periodontal patients. This patient admitted to smoking but also told the author that she wished to quit. She possessed several of the risk factors previously identified.
The patient had adequate bone volume for two distal tilted and two vertical maxillary implants. If a vertical implant placement protocol was to be implemented, the patient would have required bone grafting into both maxillary sinuses in order to develop adequate bone volume for posterior, vertical implant placement. The tilted posterior implant protocol eliminates maxillary sinus bone grafting and has proved to be efficacious. In a systemic review, Menini et al. (2012) reported on the results of a literature review that evaluated outcomes of vertical and tilted implants supporting full-arch fixed implant prostheses used in immediate occlusal loaded, maxillary prostheses. Eleven articles were analyzed; a total of 1623 maxillary implants (778 tilted, 845 upright) were placed into 324 patients. Seventeen tilted (2.19%) and 16 vertical implants (1.89%) failed during the first year. No significant differences in failure rates were reported between tilted and vertical implants (P value = 0.52). Marginal bone level results were reported in six studies. A nonsignificant mean difference between tilted and vertical implants was found with regard to bone loss. Tilted implants demonstrated a favorable short-term prognosis in full-arch immediate loading rehabilitations of maxillae. Menini and others noted that randomized long-term trials were needed to better elucidate long-term success of tilted and vertical implants.
The mandibular teeth presented with a poor long-term prognosis secondary to the advanced horizontal bone loss. Periodontal surgical treatment was a potential option, but the risk/benefit ratio would have been disproportionate to the benefits of maintaining the teeth as the patient did not have enough bone volume in the posterior mandible for vertical implant placement. Substantial bone grafting would have been required with increased costs and morbidity.
Extraction, alveolectomy, implant placement, and IOL for a full-arch prosthesis were the treatment plan that, in the author’s opinion, represented the treatment that would have the best, long-term prognosis. Grandi et al. (2012) reported on the outcomes of immediately loaded mandibular full-arch prostheses according to the AO4 concept supported by implants placed in fresh extraction sockets up to 18 months after loading. Their study included 47 patients, 47 mandibular prostheses, each supported by four implants (n = 188). Patients received fixed implant-retained prostheses with metal frameworks within 48 hours of surgery; definitive prostheses were placed approximately 6 months later. At the 18-month follow-up appointments, Grandi and others noted no implant failures and all prostheses were stable and successful. They concluded that within the limits of the study, it can be suggested that immediately loaded mandibular cross-arch fixed dental prostheses can be supported by four postextractive implants successfully; however, they also noted that larger and longer follow-ups were needed. Galindo and Butura (2012) reported similar results after one year of function with definitive prostheses.
Treatment Options
Two treatment options were developed for this patient.
Treatment option 1 included:
- Implant placement per the AO4 protocol that included extraction of the mandibular teeth
- Maxillary and mandibular alveolectomies to provide adequate restorative volumes for prosthetic treatment
- Placement of two posterior tilted implants and two anterior vertical maxillary and mandibular implants with high insertion torques
- Fabrication and insertion of full-arch maxillary and mandibular fixed prostheses on the day of surgery
Treatment option 2 included:
- Extraction of the mandibular teeth
- Alveolectomy to provide adequate restorative volume for a mandibular implant-supported overdenture
- Placement of two mandibular anterior implants for use as overdenture abutments, unloaded healing, and single-stage surgical protocol
- Fabrication and insertion of a maxillary complete denture
- After osseointegration, placement of resilient overdenture abutments into the osseointegrated implants
- Fabrication and insertion of a mandibular implant-supported overdenture
Prognosis
Prognosis has been defined as literally foreknowing, foreseeing; it is a medical term for predicting the likely outcome of one’s current standing or disease process. When applied to large statistical populations, prognostic estimates can be quite accurate. However, it is much harder to translate this into a prognosis for a specific patient. A complete prognosis includes the expected duration, function, and a description of the course of the disease and success of treatment.
Based on the available literature on IOL using the AO4 protocol, the author rated the prognosis for treatment option 1 as excellent. The patient’s chief complaints would be satisfied in that she would have fixed, nonremovable prostheses; have no palatal coverage; enjoy relatively normal function with relatively little likelihood of prosthetic complications; and experience minimal bone loss; and excellent implant survival had been reported in the literature.
Based on the available literature on single-stage surgical protocols and implant survival with the mandibular overdenture treatment concept, the author rated the prognosis for treatment option 2 as good. Mandibular implants that supported overdentures were known to have high survival rates and significantly improved patients’ quality of life. Lee et al. (2012) reported in a systematic review regarding treatment outcomes of mandibular implant overdentures that implant survival rates of mandibular overdentures was high regardless of the number of implants used in specific cases. Denture maintenance was not likely influenced substantially by the number of implants; patient satisfaction was typically high, again regardless of the number of implants used in a given case. This patient was likely to enjoy reasonable function with the mandibular implant-supported overdenture, but both prostheses would be removable by the patient. The patient had previously reported difficulty with wearing/managing a maxillary complete denture. However, the author never had a chance to evaluate the preexisting denture relative to fit, occlusion, or aesthetics.
Appointment 3: Consultation Restorative Dentist/Patient
A separate consultation was scheduled with the patient and her husband. The diagnoses of her existing disease were thoroughly discussed and explained. The two distinctly different treatment options were also discussed and explained with models, verbal descriptions, and power point slides of patients with similar physical presentations and treatments. Her own mounted casts and maxillary wax denture were also used. All of their questions were answered; they indicated that they understood the disease processes and treatment options, including no treatment. No treatment was immediately ruled out due to her lack of maxillary teeth/prosthesis. They selected treatment option 1 that included immediate, full-arch prostheses supported by four implants in both jaws.
Since the wax denture was already made and the articulator mounting was correct, arrangements were made to fabricate the immediate prostheses. A consultation was scheduled between the author and the treating surgeon.
Appointment 4: Consultation Prosthodontist/Surgeon
This particular surgeon was most familiar with NobelActive™ implants, manufactured by Nobel Biocare, Yorba Linda, CA, USA. Multiple studies have demonstrated that immediate implant placement into fresh extraction sites, where implants require high primary stability, can be impacted by implant surface texture and macroscopic design elements (Vanden Bogaerde et al. 2005; Crespi et al. 2010). NobelActive implants were designed to optimize the osseointegration phenomenon with a variable thread design and an oxidized, highly crystalline, phosphate-enriched titanium dioxide surface that has demonstrated high primary stability and reduced risk of nonintegration when compared to machined surface implants with immediate loading protocols (Glauser et al. 2001; Rocci et al. 2003). NobelActive implants were designed with macroscopic grooves on the threads of the implants. Hall et al. (2005) demonstrated increased rates of bone growth within the grooves and faster osseointegration when compared to implants without the grooves (Figures 9.24).
Figure 9.24 Illustration of a NobelActive™ implant.

The threads of this implant system were designed to provide high insertion torque and, consequently, high primary stability. The implant was designed to function as an osteotome that condenses the surrounding bone as the implant goes to place. The thread spacing increases from the apical end to the coronal portions of the implant; this supposedly results in increased axial and radial bone compression during implant placement. Clinicians have found this useful in areas of soft bone. NobelActive implants also have been machined with platform switching at the implant restorative platforms (Figures 9.25). The manufacturer has stated that this design feature allows for increased soft tissue preservation by providing a secure internal prosthetic interface along with a narrow emergence profile. Using narrow implant restorative components on slightly wider implant restorative platforms has been shown to have positive effects on bone and soft tissue remodeling around dental implants (Lazzara and Porter 2006; Vandeweghe and De Bruyn 2012).
Number/Size of Implants
Based on the patient’s anatomy and desires for maxillary and mandibular fixed prostheses, it was decided to use the AO4 treatment protocol. The surgical plan called for placement of four maxillary NobelActive implants (two posterior implants tilted; two anterior implants vertical) and four mandibular NobelActive implants (two posterior implants tilted; two anterior implants vertical). The diameters of the implants were planned to be 4.3 mm, the posterior implant lengths were planned to be at least 15 mm, and the anterior lengths were planned to be at least 11.5 mm (Figures 9.26).
Figure 9.25 Illustration of the conical connection and platform-switched implant restorative platform of a NobelActive implant.

Figure 9.26 Schematic illustration of the tentative locations of four maxillary and four mandibular NobelActive implants per the AO4 protocol.
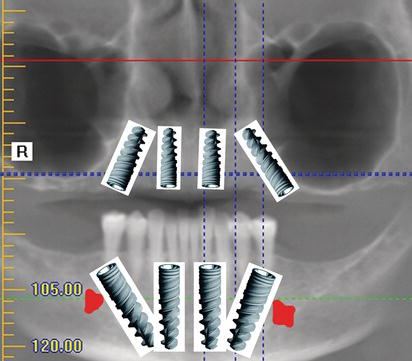
Figure 9.27 Right posterior laboratory image of the maxillary diagnostic cast and record base mounted against the mandibular diagnostic cast at the selected VDO.

Figure 9.28 Left posterior laboratory image of the maxillary diagnostic cast and record base mounted against the mandibular diagnostic cast at the selected VDO.

Prosthesis Design
Both prostheses were planned to include screw-retentive elements, which would preclude leaving any remnants of cement behind after insertion of the interim prostheses. The prostheses were to be fabricated as conventional, acrylic resin, removable-type prostheses (Figures 9.27–9.36). Conventional prosthodontic protocols were followed in order to establish the appropriate VDO, jaw and tooth relationships, lip support, and incisal display during speaking, smiling, and at rest. This was accomplished with alginate impressions, fabrication of diagnostic casts and maxillary record base with an occlusion rim, articulated casts, and denture wax set up with a clinical try-in appointment.
Figure 9.29 Anterior laboratory image of the maxillary diagnostic cast and record base mounted against the mandibular diagnostic cast at the selected VDO. The mandibular left anterior and posterior teeth were removed in anticipation of extractions and alveolectomy required for the AO4 clinical procedures.

Figure 9.30 Right posterior laboratory image of the maxillary diagnostic cast and record base mounted against the mandibular diagnostic cast at the selected VDO. The denture teeth were set per the occlusal plane established at the clinical jaw relation records appointment.

Figure 9.31 Right posterior laboratory image of the maxillary diagnostic cast and record base mounted against the mandibular diagnostic cast at the selected VDO. The mandibular right anterior and posterior teeth were removed in anticipation of extractions and alveolectomy required for the AO4 clinical procedures.

Figure 9.32 Left posterior laboratory image of the maxillary diagnostic cast and record base mounted against the mandibular diagnostic cast at the selected VDO. The denture teeth were set per the occlusal plane established at the clinical jaw relation records appointment.

Implant/Abutment Connection
The NobelActive internal connection per the manufacturer was machined with a hexagonal interlocking, built-in platform shifting, and external platform for fixed restorations at the implant restorative platform level (Figures 9.37). The connection was machined with 60° rotational increments, uniform load distribution with accurate implant/abutment fit, and an implant/abutment interface that allows for individual emergence profile designs for improved soft tissue maintenance. This concept was validated with an 18-month clinical study that involved the use of narrow-diameter abutments over larger-diameter implant restorative platforms. Cocchetto et al. (2010) placed 15 Certain PREVAIL implants (Biomet 3i, Palm Beach Gardens, FL, USA) into ten patients. PREVAIL implants also have been machined with built-in platform switching. The 5 mm diameter implants were connected to 4.1 mm healing abutments in a single-stage surgical protocol. Periapical radiographs were taken before and immediately after surgery, 8 weeks after implant placement, immediately after definitive prosthesis insertion, and at 12 and 18 months after loading. The serial radiographs taken during this study revealed an average peri-implant bone loss of 0.30 mm. The authors concluded that increasing the discrepancy between the diameters of implant platforms and restorative abutments may lead to a decrease in the amount of subsequent crestal bone loss (Figures 9.38).
Figure 9.33 Anterior laboratory image of the maxillary diagnostic cast and record base mounted against the mandibular diagnostic cast at the selected VDO. The denture teeth were set per the occlusal plane established at the clinical jaw relation records appointment.

Figure 9.34 Anterior laboratory image with the denture teeth set per the findings established at the clinical jaw relation records appointment.

Figure 9.35 Right laboratory image with the denture teeth set per the findings established at the clinical jaw relation records appointment.

Figure 9.36 Left laboratory image with the denture teeth set per the findings established at the clinical jaw relation records appointment.

Figure 9.37 Laboratory image of the cross section of theinternal conical connection, with hexagonal interlocking between the implant and abutment connection. Thisconnection results in a tight seal between implants andabutments, as well as provides high mechanical strength.
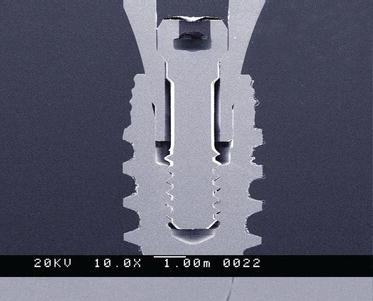
Figure 9.38 Schematic illustration of the built-in platform shifting (circle) for maximum soft tissue volume and minimal crestal bone loss for NobelActive implant restorative platforms.

Surgical Work-Up and Protocol
The author and the surgeon decided to use the IOL concept that has been termed AO4. Per Malo, the indications for these procedures include edentulous maxillae and mandibles or dentitions with hopeless periodontal/caries prognoses (Malo 2012). The principles involved with this treatment protocol include four implants – two vertical in the anterior jaw segments and two angled implants in the posterior segments. The implants are placed in specific positions in order to support fixed, provisional, immediate, full-arch prosthe/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


