Chapter 7
Accelerated Treatment Protocol of a Patient with Edentulous Jaws and CADCAM Titanium Framework/Fixed Hybrid Prostheses
LITERATURE REVIEW
Multiple prosthetic options exist for rehabilitation of patients with edentulous mandibles: conventional complete dentures, implant-retained/supported overdentures, and fixed implant-retained full-arch prostheses. These treatments all have benefits and limitations associated with them: cost, complexity, length of treatment, prognosis, function, and aesthetics (Adell et al. 1981; Morin et al. 1998; Allen et al. 1999; Wright et al. 2002).
Patients treated with complete dentures often express dissatisfaction with function, aesthetics, and phonetics (Carlsson et al. 1967; Awad & Feine 1998). In a clinical trial, Bilhan et al. (2013) assessed satisfaction, as well as the frequency and type of prosthetic complications in terms of several variables, in patients with complete dentures. They studied 64 patients with a mean age of 63.48 years who presented to a private clinic wearing complete dentures and who requested new dentures. The degree of patient satisfaction with their dentures was assessed, as well as complications and parameters related to the dentures such as the accuracy of vertical dimensions and centric relation, arrangement and possible malposition of the artificial teeth, and the border length of the denture bases. They reported that the most common complication was loss of retention (85.9%), followed by ulceration (44.2%). Mandibular dentures with long vestibular borders showed a significantly higher incidence of epulis fissuratum (P = 0.017); denture-related sore spots influenced patients’ speaking ability (P = 0.023). Bilhan and others concluded that routine recall examinations seem to be important for wearers of complete dentures, as insidious complications may develop and cause damage to the dentures as well as the patients’ oral tissues. In edentulous situations, dental implants may provide significant improvements in terms of increased retention, stability, comfort, and decreased bone resorption (Lindquist et al. 1988; Melas et al. 2001; Awad et al. 2003; Thomason 2012).
Prosthetic/implant treatment options should be carefully evaluated early in the planning process because treatment options have different requirements relative to anatomical constraints, surgical morbidity, patient expectations, patient function, and costs (DeBoer 1993; Feine et al. 1998; Zitzmann & Marinello 2002). The fixed mandibular implant-retained prosthesis supported by commercially pure or titanium alloy implants represents one of the earliest, most predictable treatments on a long-term basis, for edentulous patients (Adell et al. 1981). This implant treatment protocol took advantage of large amounts of residual bone in edentulous mandibles (anterior, between the mental foraminae) and avoided areas that exhibited more resorption (posterior) (Figures 7.1 and 7.2). Some of the posterior teeth were replaced on cantilevered segments. Romanos et al. (2012) conducted a systematic literature review of all published articles identified through a search of MEDLINE from January 1980 through June 2011 using the terms crestal bone loss, dental implants, distal cantilevers, marginal bone loss, and periodontal disease. The identified articles that met the inclusion criteria described fixed complete dental prostheses utilizing distal cantilevers. In vivo studies were included for data extraction while in vitro and animal studies were used for descriptions of clinical or mechanical performance. Romanos and others concluded that, based on the 19 cited articles (including 14 human studies), it was difficult to derive data-based conclusions regarding the use of cantilever prostheses other than an approximate 95% prosthetic survival rate. Subjective and objective information from these studies demonstrated a distinct preference for the use of distal cantilever prostheses, as few risks were associated with this type of prostheses. They also concluded that a careful evaluation of the studies demonstrated that cantilevered prostheses provided a treatment option without a high risk of complications (Figure 7.3).
Figure 7.1 Radiograph of an edentulous mandible with five implants between the mental foraminae. Some of the posterior teeth have been replaced on the cantilevered segments of the prosthesis.
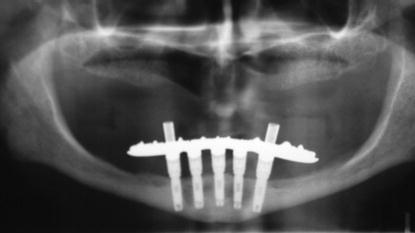
Figure 7.2 Close-up view of the right posterior segment in Figure 7.1. Note the amount of bone resorption in the posterior mandibular segment. The proximity of the inferior alveolar canal to the crest of the alveolar ridge precluded placement of implants posterior to the mental foramen.

Numerous studies have demonstrated excellent long-term results for edentulous patients treated with dental implants per the Brånemark protocol (Zarb & Albrektsson 1985; Albrektsson 1986; Lindquist et al. 1996; Testori et al. 2002; Mertens & Steveling 2011). Age does not seem to be an absolute contraindication for dental implants. In a retrospective study, Engfors et al. (2004) studied 133 edentulous patients who were 80 or more years of age and who were consecutively treated with fixed implant-retained prostheses. Seven hundred sixty-one Brånemark-type implants were placed into 139 edentulous jaws. The 5-year cumulative survival rate (CSR) for the earlier group for both jaws was 93%. A control group of patients younger than 80 years of age was 92.6%. The corresponding CSRs for the mandibular implants were 99.5% and 99.7%, respectively. The most common complications in the earlier 80-year-old group were soft-tissue inflammation (mucositis) and cheek/lip biting. Veneer fractures of the denture teeth from the prostheses were the most common complaint of the younger than 80-year group. Engfors and others concluded that results of implant treatment in patients over 80 years of age were not significantly different than treating younger patients. However, there were more postinsertion complications and adjustment visits in the 80 + -year-old group of patients.
Figure 7.3 Laboratory occlusal view of mandibular fixed hybrid implant prosthesis. This prosthesis was supported by four implants per the AO4® protocol. The anterior/posterior (A/P) spread enabled the metal framework to support the cantilevered first molars.

With the development of osseointegration and the limited amount of motion inherent between an osseointegrated implant and the surrounding bone, accurate, passively fitting implant frameworks have been one of the goals in implant treatment (Branemark et al. 1977). An osseointegrated implant has micromotion within the bone of approximately 10 µm; a natural tooth may move up to 100 µm (Assif et al. 1996). This lack of flexibility or intimate fit at the bone/implant interface means that any forces induced into the system via ill-fitting frameworks will almost certainly remain in the system and may result in biomechanical issues such as screw loosening and/or screw fracture.
Multiple authors have examined impressions and master cast accuracy in implant treatment (Carr 1991; Hsu et al. 1993; Herbst et al. 2000). Kari et al. (2004) performed a laboratory study to determine the degree of passive fit in cement- and screw-retained frameworks. They concluded that an absolute passive fit of implant superstructures is not possible using conventional clinical and laboratory procedures. They proposed that reference strain values from implant-retained prostheses that have functioned without apparent complications could help define a biologically acceptable fit.
Titanium frameworks have been used as alternatives to gold castings for implant frameworks for over 15 years (Ortorp & Jemt 2004). Titanium is less expensive than noble alloys, is well tolerated in biologic environments, and has been shown to develop mucosal attachments whereas gold alloys do not (Abrahamsson et al. 1998). Computer numeric controlled (CNC) milling procedures with titanium alloys allow better control of distortions inherent within the waxing/casting/finishing processes associated with conventional casting technology. Ortorp and Jemt (2004) reported on the results of a prospective clinical study with 129 edentulous patients who were treated with 67 CNC frameworks and 62 frameworks made with gold alloys and conventional casting techniques. Clinical and radiographic data were obtained over a 5-year period.
Ortorp and Jemt (2004) reported that problems were low in both groups (34% of the CNC group and 26% of the control group reported no problems during the study). The CSRs were 94.9% and 98.3% for implants and titanium prostheses, respectively. The respective corresponding CSRs for the control group were 97.9% and 98.2% for implants and titanium prostheses, respectively. Metal fractures were only seen in the control group (casting). Mean marginal bone loss was 0.5 mm in both groups. They concluded that CNC titanium frameworks were a viable alternative to gold alloy castings in edentulous jaws. However, the degree of fit between implant abutments and frameworks was not quantitatively measured.
Zirconium dioxide (ZrO) frameworks have also been used in fixed, full-arch implant prostheses. Katsoulis et al. (2012) analyzed the precision of fit of implant-supported, screw-retained computer-aided design and computer-aided manufacturing (CADCAM) ZrO frameworks. Katsoulis and others designed a study whereby CADCAM ZrO frameworks (NobelProcera®) for screw-retained 10-unit implant-supported reconstructions on six implants (FDI positions 15, 13, 11, 21, 23, 25) were fabricated. The data were digitized by using an optical scanner (laser (ZrO-L, n = 6)) and a mechanical scanner (ZrO-M, n = 5) to record the implant platforms and the framework resin patterns (copy mill technique). Laser-scanned CADCAM titanium (TIT-L, n = 6) and cast CoCrW-alloy frameworks (Cast, n = 5) were fabricated on the same patient master model and designed similar to the ZrO frameworks; the Ti and CoCrW alloy frameworks were the controls. The one-screw test (implant site #25, screw-retained) was applied to assess the vertical microgaps between implant and framework platforms with a scanning electron microscope. The mean microgaps were calculated from proximal and buccal values. Statistical comparisons were performed with nonparametric tests. Katsoulis and others reported that no statistically significant pairwise differences were observed between the relative effects of vertical microgap between ZrO-L (median 14 µm; 95% CI = 10–26 µm), ZrO-M (18 µm; 12–27 µm), and TIT-L (15 µm; 6–18 µm). However, the values of the cast CoCrW frameworks (236 µm; 181–301 µm) were significantly higher (P < 0.001) than the three CADCAM groups. Katsoulis and others concluded that optical and tactile scanners with CADCAM technology resulted in highly accurate long-span screw-retained ZrO implant reconstructions. Titanium frameworks showed the most consistent precision fits. Fit of the cast alloy frameworks was clinically unacceptable.
The original case report for this chapter illustrated a conventional approach for the prosthetic reconstruction of a patient after implants were placed in a single-stage surgical protocol. The prosthetic appointments for this treatment included the following.
ORIGINAL TREATMENT PROTOCOL
The new chapter features a clinical protocol that the author has termed Accelerated Treatment whereby the eight clinical appointments provided earlier were decreased to a total of three clinical appointments. This new protocol has been extremely well received by patients; it is more efficient in terms of clinic time required, as well as patients require less time off from work (Drago 2012).
The following clinical case report demonstrates the treatment of an edentulous patient with implants and fixed implant-retained prostheses in both jaws. The patient originally presented with Type III and Type IV periodontal disease in the mandible; she was edentulous in the maxillae (Figures 7.4–7.8). The patient had a maxillary denture constructed approximately 10 years previous to this first visit; it was not comfortable, and the patient was so irritated by it that she never used it. The mandibular teeth were seriously infected with periodontal disease; the patient no longer wished to spend any time, money, or effort in retaining them. She was interested in fixed, implant-retained prostheses.
Figure 7.4 Preoperative clinical image of the patient at her original presentation to the author for treatment. She chose not to wear her existing maxillary denture as it was not comfortable, and she did not like the aesthetics associated with it.
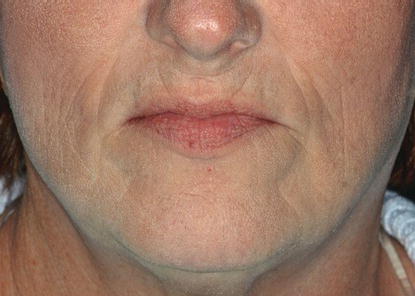
Figure 7.5 Preoperative, intraoral clinical image of the patient’s existing dentition as she presented to the author for treatment.

After thorough physical and radiographic examinations, the patient was classified as Class III per the Prosthodontic Diagnostic Index (McGarry et al. 2002):
- Residual ridge morphology with minimum influence to resist horizontal or vertical movement of the denture base; Type C maxilla
- Location of muscle attachments
- Class I, II, or III maxilla/mandibular relationship
- Conditions requiring preprosthetic surgery
- Simple implant placement; no augmentation required
- Multiple extractions leading to complete edentulism for immediate denture placement
Figure 7.6 Preoperative, intraoral clinical image of the patient’s edentulous maxillae. Note the broad posterior edentulous ridges, as well as the amount of keratinized tissues present. The posterior ridges were all soft tissue; there was no bone available for posterior implant placement.

Figure 7.7 Preoperative, intraoral clinical image of the patient’s mandibular dentition as she presented to the author for treatment. Note the significant accumulations of supragingival calculus and stains attached to the lingual surfaces of the mandibular anterior teeth.

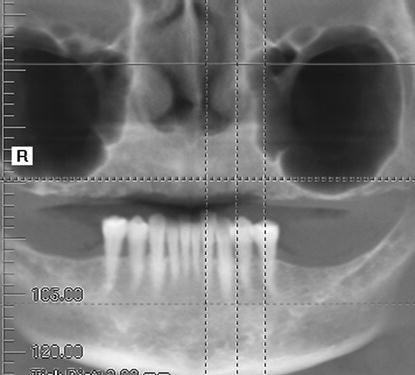
Figure 7.8 Preoperative panoramic radiograph at the patient’s initial presentation to the author for treatment. Note the significant amount of bone present in the anterior maxillae; the significant pneumatization of both maxillary sinuses precluded the use of posterior, vertical implants without significant bone grafting.
The patient elected to proceed with extraction of the remaining mandibular teeth and placement of implants in both jaws per the All-on-4® (AO4) protocol. The AO4 protocol will be illustrated in a different chapter. This chapter’s treatment will commence approximately 4 months after the date for the earlier surgeries; the author typically allows 4 months to elapse between the surgical appointment and initiation of the definitive prosthetic phase of treatment.
The treatment plan was originally agreed upon prior to the initial treatment that included extractions, implant placement, and immediate occlusal loading with full-arch restorations. The treatment plan for the definitive prostheses is in Table 7.1.
ACCELERATED TREATMENT PROTOCOL
CLINICAL CASE PRESENTATION 4 MONTHS POST EXTRACTIONS, IMPLANT PLACEMENT, AND IMMEDIATE OCCLUSAL LOADING
Appointment 1: Evaluate Aesthetics, Jaw Relation Records, Abutment-Level Impressions (3 Hours)
The patient was now approximately 4 months post extractions, implant placement, and immediate occlusal loading with full-arch prostheses per the AO4® protocol. She was very pleased with the aesthetic, phonetic, and functional results of the treatment; she did not request any changes to be made from the interim prostheses to the definitive prostheses.
Radiographic Examination (CBCT)
A postoperative cone beam computed tomography (CBCT) was taken after the maxillary interim prosthesis was inserted to identify the locations of the implants and for a macroscopic evaluation of crestal bone levels and bone implant contact (Figure 7.9).
Extraoral Physical Evaluation
The patient’s overall aesthetic appearance was pleasing (Figure 7.10). She presented with excellent lip support and incisal displays during speaking, smiling, and at rest. The vertical dimension of occlusion also appeared to be quite satisfactory – both subjectively and objectively by the author.
Intraoral Physical Examination
The patient presented with even occlusal contacts throughout the prostheses and bilateral Class I occlusal relationships (Figure 7.11). Both prostheses were stable and relatively plaque-free. The peri-implant soft tissues were also within normal limits.
Clinical Assessment
Since the patient was pleased with the aesthetic, phonetic, and functional results, and the author considered the interim prostheses to be aesthetic and satisfied the basic prosthodontic requirements, it was decided to maintain the existing occlusal relationships and translate them to the definitive prostheses. The implants appeared to be osseointegrated. The definitive clinical determination would be established after the interim prostheses were removed, and each individual implant/abutment could be evaluated for mobility.
Table 7.1 Treatment plan (maxillary/mandibular fixed, hybrid, screw-retained implant prostheses).
| Diagnoses | ||
| 1. Edentulous maxillae with mild resorption anteriorly and moderate/significant resorption posteriorly | ||
| 2. Edentulous mandible with mild resorption | ||
| 3. Eight osseointegrated implants | ||
| 4. Fixed, full-arch interim maxillary and mandibular prostheses | ||
| Prosthetic services | Insurance code | Fee |
| Comprehensive oral evaluation | ______ | ______ |
| Diagnostic casts | ______ | ______ |
| Cone beam – three-dimensional image reconstruction using existing data, includes multiple image | ______ | ______ |
| Surgical guides | ______ | ______ |
| Maxillary screw-retained hybrid prosthesis with CADCAM framework | ||
| CADCAM framework | ______ | ______ |
| Mandibular screw-retained hybrid prosthesis with CADCAM framework | ||
| CADCAM framework | ______ | ______ |
| Yearly recall appointment | ______ | ______ |
| Periapical radiographs | ______ | ______ |
| Benefits | ||
| Both prostheses will be fixed and not removable by the patient. The patient should enjoy improved function. The occlusion (bite) will be made optimal; facial aesthetics should be maintained, consistent with the patient’s desires. The patient should enjoy an excellent, long-term prognosis. Long-term bone loss will be minimized in both jaws. | ||
| Limitations | ||
| Cost, complexity, and length of treatment (2–3 months). Implants are generally successful in the edentulous jaws approximately 96–99% of the time. The implants have to be placed optimally for the earlier treatments to be accomplished. If the implants cannot be placed optimally, changes in the treatments (surgical and prosthetic), fees, and designs will be likely. Neither prosthesis will be removable by the patient. In certain situations, one or both prostheses may need to be removed at any of the follow-up visits. The patient needs to return to this office at least once per year for follow–up, which will include radiographs (x-rays) to assess osseointegration of the implants, fit and occlusion of the prostheses, health of the soft tissues, and the integrity of the implant/abutment connections. This treatment plan itemizes only the prosthetic phase of treatment. | ||
| Patient signature________________________________________________________ | ||
| Date________________________________________________________ | ||
| Witness________________________________________________________ | ||
| Date ________________________________________________________ | ||
Figure 7.9 CBCT panoramic image of the patient immediately after insertion of the interim maxillary prosthesis, prior to insertion of the mandibular interim prosthesis using the AO4 protocol.
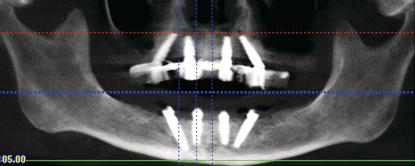
Figure 7.10 Clinical image of the patient smiling approximately 4 months post tooth extractions, implant placement, and immediate occlusal loading of maxillary and mandibular full-arch prostheses. The patient was thrilled with the aesthetic, phonetic, and functional results of the interim prostheses and was ready to proceed with construction of the definitive prostheses with CADCAM frameworks.

Figure 7.11 Clinical, intraoral image of the patient in centric occlusion, 4 months postoperative. The interim prostheses had been fabricated at a tentative vertical dimension of occlusion, in a Class I occlusal relationship.

Figure 7.12 Clinical image of the face bow record. The face bow was aligned parallel to the interpupillary line as the horizontal reference point.

Figure 7.13 Clinical image of the centric jaw relation record. Bimanual manipulation of the mandible was used to properly orient the mandible into the appropriate jaw relationship, at the existing vertical dimension of occlusion.

Figure 7.14 Clinical occlusal image of the maxillary interim prosthesis screw access restorations – left segment.

Jaw Relation Records
Face bow and centric jaw relation records were made using conventional prosthodontic principles and techniques (Figure 7.12) (Pound 1970). The jaw relation records were made with poly vinylsiloxane interocclusal impression material, at the existing vertical dimension of occlusion (Figure 7.13).
Removal of Interim Prostheses/Alginate Impressions for Diagnostic Casts
The interim prostheses were removed by removing the screw access restorations and unscrewing the retaining screws (Figures 7.14–7.17). After the interim prostheses were removed, alginate impressions were made, and diagnostic casts were poured in dental stone (Figures 7.18 and 7.19).
Assess Implant/Abutment Stability and Clinical Osseointegration
Clinical osseointegration is actually a histologic diagnosis (Branemark et al. 1977). There are a significant number of literature citations that demonstrated high survival rates for implants placed with high primary stability, into the parasymphysis regions of edentulous mandibles, splinted together with some type of rigid interim prostheses and placed into immediate functional occlusion (Schnitman et al. 1997; Tarnow et al. 1997; Jaffin et al. 2000; Grunder 2001; Strietzel et al. 2011). This modality may also be considered for partially edentulous patients with severe periodontal disease (Cooper et al. 2002). Cooper et al. (2002) demonstrated a 6- to 18-month postimplant placement CSR of 100% for mandibular implants placed with high primary stability, immediate post extraction of periodontally compromised teeth, rigidly splinted together with acrylic resin prostheses, and placed into fully functional occlusion.
Figure 7.15 Clinical occlusal image of the maxillary interim prosthesis screw access restorations – right segment.

Figure 7.16 Laboratory image of the intaglio surface of the maxillary interim prosthesis. Immature plaque had accumulated on this surface.

Figure 7.17 Laboratory image of the intaglio surface of the mandibular interim prosthesis. Immature plaque and calculus had accumulated on this surface.

Figure 7.18 Laboratory occlusal image of the diagnostic cast of the maxillary interim prosthesis. This was poured from the alginate impression that was made immediately after the maxillary interim prosthesis was removed from the maxillary implants.

Figure 7.19 Laboratory facial image of the diagnostic cast of the mandibular interim prosthesis. This was poured from the alginate impression that was made immediately after the mandibular interim prosthesis was removed from the mandibular implants.

Buser et al. (1997) and Cochran et al. (2002) considered implants to be successful if they satisfied the following criteria:
- Absence of pain or any negative subjective sensation
- Absence of clinical detectable implant mobility
- Absence of any recurrent peri-implant mucositis and/or peri-implantitis accompanied by swelling, redness, or pain of the peri-implant mucosa
- Absence of continuous peri-implant radiolucency
- Absence of mesial and/or distal vertical bone loss of more than 30% of the endosseous part of the implants
- No need to repair or replace the implant-supported prosthesis
- Subjective evaluation of the treatment outcomes
Figure 7.20 Clinical image of torque driver in place on a posterior maxillary implant. This was a 30° angled abutment; the abutment screw was torqued to 15 N cm, per the manufacturer’s instructions.

Figure 7.21 Clinical image of torque driver in place on an anterior maxillary implant. This was a straight abutment; the abutment screw was torqued to 35 N cm, per the manufacturer’s instructions.

Figure 7.22 Clinical image of the maxillary abutments in place after the abutment screws were torqued to the appropriate levels.

Figure 7.23 Clinical image of the mandibular abutments in place after the abutment screws were torqued to the appropriate levels.

Clinically, the abutment screws were torqued to 15 N cm for the posterior angled abutments and 35 N cm for the anterior straight abutments (Figures 7.20 and 7.21). The patient reported no pain or tenderness during these clinical procedures; no mobility was detected. The implants were considered to be osseointegrated (Figures 7.22 and 7.23).
Abutment-Level Impressions
Impressions for implant restorations may be made at the implant restorative platform level (Figure 7.24) or at the abutment level (Figure 7.25). Implant impressions also may be splinted together prior to the impression or remain as individual units. Accuracy of splinted versus unsplinted implant impressions has been studied by numerous authors. Papaspyridakos et al. (2011) reported on the results of an in vivo study where they investigated the effect of implant impression techniques (splinted vs. unsplinted) on the accuracy of fit of fixed implant prostheses in edentulous patients. This clinical study included 12 edentulous patients (13 edentulous jaws). All patients had undergone computer-guided, prosthetically driven implant surgery. Splinted (with acrylic resin) and unsplinted pickup implant impression protocols were used to generate two different casts. Intraoral verification indexes were made to fabricate a third index cast (prosthesis fabrication cast); these made up a control group. All patients were definitively rehabilitated with one-piece zirconia prostheses. The accuracy of each prosthesis was evaluated indirectly by examining them clinically and radiographically, with the prostheses in place on the generated casts. Of the 13 casts made with splinted impression copings, 12 were reported to have accurate prostheses. Six of the thirteen frameworks made from unsplinted impression copings demonstrated accurate clinical fits. The authors concluded that there was clinical evidence that splinted impression copings generated more accurate implant impressions and master casts than the unsplinted impression coping technique for complete-arch, one-piece fixed prostheses.
Figure 7.24 Clinical image of implant restorative platforms of NobelActive™ implants. This implant/abutment connection has been called the NobelActive Conical Connection (inset).
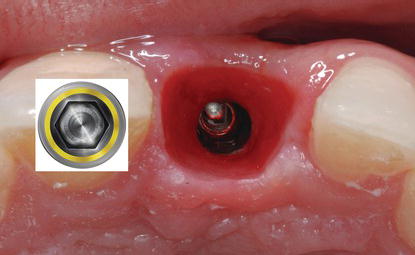
Figure 7.25 Close-up view of a 17° angled, multiunit abutment with the NobelActive Conical connection. This connection has a six-sided hex that enables the abutment to be placed such that the screw access opening exits lingual to the facial surface of an anterior implant.

Figure 7.26 Clinical image of the maxillary interim prosthesis in place, retained by long abutment impression coping screws. Note that the screws are occlusal/incisal to the occlusal/incisal surfaces of the posterior and anterior segments of the prosthesis, respectively.

Instead of using splinted abutment impression copings, the author used the interim prosthesis as the verification index. Long abutment impression coping screws were placed into the screw access openings of the interim prosthesis such that they extended past the occlusal surfaces of the teeth (Figure 7.26). Due to shrinkage of the soft tissues secondary to healing, a small amount of space existed between the intaglio surface of the maxillary int/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


