Chapter 6
Retreatment of a Patient with a Fractured Implant-Retained Fixed Partial Denture in the Posterior Maxilla-CADCAM Abutments and a New Fixed Partial Denture (Cement Retained)
LITERATURE REVIEW
Dental implant restorations placed in the 1980s had challenges associated with the biology of osseointegration, as well as biomechanics of prosthesis survival (Adell et al. 1981; Kallus & Bessing 1994). Implant prostheses were initially designed with screw retention to facilitate removal and repair; in some cases, aesthetics and occlusion principles were sacrificed (Zarb & Schmitt 1990).
As implant treatment modalities changed from edentulous patients to include partially edentulous patients, there were reports of prosthetic complications that had a negative impact on overall success rates in implant restorative treatment. Zarb and Schmitt (1990) reported on 274 implants placed in 46 consecutive patients followed for up to 9 years. The success rate for the implants was 89.05%; the success rate for the prosthetic treatment was 100%. The 100% prosthetic survival rate (SR) indicated that none of the implant restorations had to be remade. Zarb and Schmitt recorded complications and problems during the surgical, restorative, and follow-up phases of treatment. Zarb and Schmitt concluded that safe retrievable techniques would result in negligible morbidity.
Hemmings et al. (1994) studied and compared maintenance requirements for fixed prostheses and overdentures in mandibular edentulous patients. They reported that postinsertion adjustments were more common in the first year in the overdenture population, but thereafter, fixed prostheses had more complications and required more maintenance. The average number of recalls for the first year was 2.27 and 1.57, respectively.
Attard and Zarb (2002) reported on the long-term success of implant-supported posterior prostheses in the first 35 consecutive, partially edentulous patients treated at the University of Toronto. They reported that the overall survival of the posterior implants was 94%. They concluded that Brånemark dental implants were highly effective in the rehabilitation of partially edentulous patients missing multiple posterior teeth.
Pjetursson et al. (2012) reported the results of a systematic review associated with implant-supported fixed dental prostheses (FDPs) in use for at least 5 years. Meta-analysis of the included studies indicated an estimated survival of implants supporting FDPs of 95.6% after 5 years and 93.1% after 10 years. The SR of implant-supported FDPs was 95.4% after 5 years and 80.1% after 10 years of function. When the analysis was done exclusively for metal-ceramic FDPs and gold-acrylic resin FDPs were excluded, the SR increased to 96.4% after 5 years and 93.9% after 10 years. Only 66.4% of patients were free of any complications after 5 years. The most frequent complications over the 5-year observation period were fractures of the veneering material (13.5%), peri-implantitis and soft tissue complications (8.5%), loss of access opening restoration (5.4%), abutment or screw loosening (5.3%), and loss of retention of cemented FDPs (4.7%). Pjetursson and others concluded that implant-supported FDPs were safe and predictable treatments with high SRs. They also concluded that complications may be minimized by using reliable components and materials, and that patients should be placed into a well-structured maintenance/recall program after treatment has been completed.
The hexagonal extension on the coronal aspect of external hex implants was originally designed as a rotational torque transfer mechanism used during surgical placement of implants. With the initiation of single-unit implant restorations, the external hex was used as an antirotation component (Beaty 1994) (Figures 6.1 and 6.2). The precision fit between implants and abutments is one of the key elements in long-term prosthetic success of implant restorations (Jemt 1986; Asavant et al. 1988). Binon (1995) contended that if the rotation between implants and abutments can be minimized, more stable and predictable screw joints will result; rotation of less than 5° is desirable for implant joint stability.
Figure 6.1 Occlusal view of 4.1 and 5.0 mm implant restorative platforms (left, right, respectively); the flat-to-flat surface dimensions were 2.7 mm.

Figure 6.2 Profile view of 4.1 and 5.0 mm diameter implants; the hexagonal heights were 0.7 mm for both implants.

The implant/abutment interface determines joint strength, stability, and lateral/rotational stability. As implant design evolved, so did implant/abutment connections. One of the first internally hexed implant/abutment designs incorporated a 1.7 mm deep hex below a 0.5 mm wide, 45° bevel (Niznick 1983). Internal connection implants were intended to distribute masticatory forces deeper within implants, which would protect the abutment screw from excessive loading forces. For increased strength, internal connection implants were made from titanium alloy instead of commercially pure (cp) titanium, which provided superior strength to the implant/abutment connection (Mollersten et al. 1997; Norton 2000).
There have been further design changes in attempts to improve stability and predictability of the implant/abutment interface. Design changes have included variations in joint designs or the numbers of hexes present within the connection system (Sutter et al. 1993; Perriard et al. 2002).
Kano et al. (2007) reported on a classification system to measure the microgaps associated with implant/abutment connections. They noted that a large microgap at the implant/abutment interface was associated with certain adverse effects that included screw loosening, abutment rotation, and abutment fracture. They proposed a classification system based on horizontal and vertical microgaps in implant/abutment interfaces. Forty-eight randomly selected external hexagonal implants were paired with (1) machined titanium abutments, (2) premachined palladium abutments cast with palladium alloy, (3) plastic burnout abutments cast with nickel chromium alloy, and (4) plastic burnout abutments cast with cobalt chromium alloy. A comparison of the horizontal and vertical microgaps at implant/abutment interfaces was completed at eight locations on each specimen to the nearest micrometer using an optical microscope with 150× magnification. P < 0.05 was the threshold for statistical significance. Kano and others reported no significant difference between groups with respect to vertical misfit. Relative to horizontal implant/abutment accuracy, machined titanium abutments presented significantly higher horizontal misfit compared to other groups (P < 0.001). Premachined cast-on abutments had significantly higher horizontal misfit than cast NiCr abutments (P < 0.001). In the proposed classification system, 23% of all sites measured at the implant/abutment interface had an ideal relationship, 34% had a horizontal discrepancy only, 4% had a vertical discrepancy only, and 39% had both vertical and horizontal discrepancies. They concluded that the proposed implant/abutment classification system demonstrated a way to characterize and compare microgap at implant/abutment interfaces.
Biomet 3i (Palm Beach Gardens, FL, USA) introduced an internal connection implant (OSSEOTITE® Certain®) in 2003 (Figures 6.3 and 6.4). This internal connection was designed with 4 mm of internal engagement that provides lateral stability for off-axis masticatory forces (Niznick 1991; Mollersten et al. 1997; Norton 2000). Mollersten et al. (1997) performed a laboratory study where they studied the depths of the joints in implant/abutment connections and found that the strength and failure modes varied significantly between the implant systems and deep joints, in contrast to shallow joints. They concluded that joint depth should be one of the considerations that should be taken into account in selecting predictable dental implant systems.
In a more recent literature review, Gracis et al. (2012) concluded that the incidence of fracture of metal-based and zirconia-based abutments and that of abutment screws was not influenced by the type of implant/abutment connection. Abutment screw loosening was the most frequently occurring technical complication. They did report that the type of connection seemed to have an influence on the incidence of the screw loosening: more loose screws were reported for externally connected implant systems for both types of materials. However, Gracis and others also reported that proper preload may decrease the incidence of this type of complication.
Figure 6.3 Cross-sectional view of Biomet 3i’s internal connection implant/abutment connection. There are three distinct zones within the implant/abutment connection: the occlusal portion is specific for a 6-point hex; the middle portion for a 12-point hex; the lower portion for the audible click with complete insertion of the restorative component.
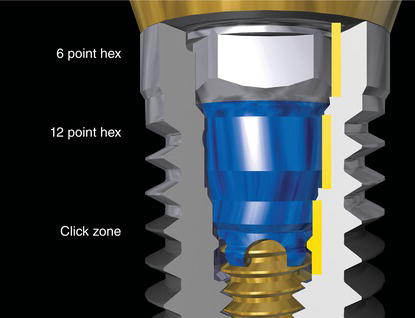
Figure 6.4 Occlusal view of the 6/12-point connection of Biomet’s internal connection implant.

Saidin et al. (2012) tested the effects of different implant/abutment connections on micromotion and stress distribution relative to microgap formation. They tested four types of implant/abutment connections: internal hexagon, internal octagon, internal conical, and trilobe. They reported that internal hexagonal and octagonal implant/abutment connections produced similar patterns of micromotion and stress distribution. They attributed this to the regular polygonal design. Internal conical implant/abutment connections produced the highest magnitude of micromotion; the trilobe implant/abutment connection demonstrated the lowest magnitude of micromotion due to its polygonal profile. Saidin et al. (2012) concluded that noncylindrical implant/abutment connections provided stable locking mechanisms that reduced micromotion and therefore reduced the occurrence of microgaps. However, they also noted that stress tended to concentrate at the vertices of all abutments, which could lead to microfractures and subsequent microgap formation.
Figure 6.5 Stock titanium alloy abutment in place on a master cast, as received from the manufacturer [GingiHue Post (IAPP454G)].
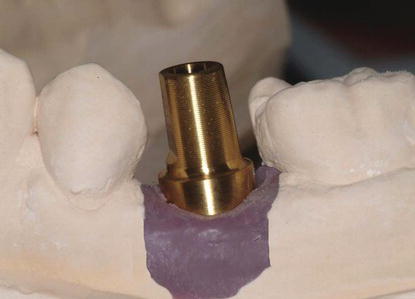
Figure 6.6 The GingiHue Post (provided in Figure 6.5) after it was prepared by a dental laboratory technician for use as an abutment for a cement-retained crown.
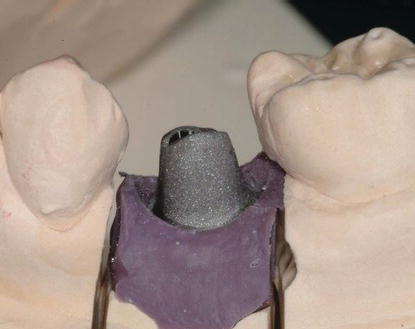
The height of the abutment screw in Biomet 3i’s internal connection system is 1.95 mm from the top of the screw to the seating surface. This reduced vertical height allows greater flexibility in the amount of abutment preparation without risk of damaging the head of the screw (Figures 6.5 and 6.6).
Figure 6.7 Profile view of a Gold-Tite® hexed abutment screw for Biomet 3i’s internal connection implant.

This internal connection system incorporates a 6-point hex design for use with straight abutments and a 12-point, double-hex design for use with preangled abutments. Stock abutments may be less expensive than custom abutments for clinicians and therefore may result in decreased costs for restorative dentists.
Abutment screws with Biomet 3i’s internal connection system are torqued to 20 N cm. Rodkey (1977) discussed that the type of finish present on abutment screws can have a considerable effect on the tension induced by a given torque. Sakaguchi and Borgersen (1995) reported that the actual preload developed within a screw joint system is dependent upon the finish of the interfaces, friction between the components, geometry, and properties of the materials in the system. Martin et al. (2001) performed an extensive laboratory study where they tested four commercially available abutment screws and their ability to generate preloads in dental implant (external hex)/abutment connections. The greatest preload values were calculated for Gold-Tite® abutment screws at 20 and 32 N cm levels. Enhanced screw surfaces have been shown to generate less friction between screws and implants than nonenhanced screws (Figure 6.7).
Computer-aided design and computer-aided manufacturing (CADCAM) technology is an exciting new method for producing implant restorations for single, multiple, and full-arch restorations. Biomet 3i’s protocol (BellaTek ® Encode ® Impression System) involves recording clinical information with digital intraoral scans or impressions and generating digital information relative to implant analogs, adjacent and opposing teeth, and the contours of the planned restoration in a computer (Drago 2006). The BellaTek ® Encode ® Impression System provides solutions to clinicians by potentially eliminating the need for implant-level impressions. This particular protocol may streamline the treatment process for surgeons, restorative clinicians, and dental laboratory technicians. This system was designed so that, in some cases, healing abutments do not have to be removed from the implants to record the spatial orientation of the implant hex. This nonremoval may have an impact on soft tissue and crestal bone preservation. Special healing abutments (BellaTek Encode Healing Abutments) (Figure 6.8), are placed at the time of implant placement with a single-stage surgical protocol or at the time implants are exposed to the oral cavity with a two-stage surgical protocol may be scanned intraorally. Clinicians, who do not possess an intraoral scanning (IOS) system, may elect to make a clinical impression of the healing abutments and scan the casts in the laboratory. The digitized information then can be manipulated by a designer to design a patient-specific abutment (Figure 6.9). Dental laboratory technicians and/or clinicians can accept or modify the design. Once the design is accepted, abutments may be milled from titanium alloy or zirconia (Figure 6.10).
Figure 6.8 Occlusal view of a BellaTek® Encode® Healing Abutment with a 5 mm emergence profile.

Figure 6.9 CADCAM of two abutments for a 3-unit, implant-retained FPD.
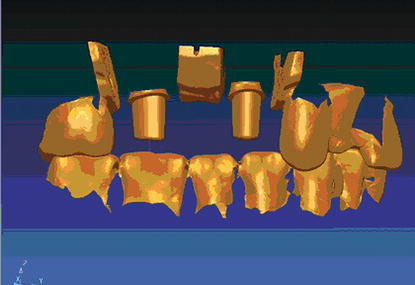
Figure 6.10 Facial laboratory view of two CADCAM titanium alloy abutments on a master cast.

Milled titanium abutments fabricated with CADCAM technology provide clinicians and dental laboratory technicians’ significant advantages over custom cast abutments made with conventional casting technology. Waxing, casting, and finishing procedures associated with conventional cast abutments have been eliminated. Generally speaking, there are significant time savings with this process since the commercial dental laboratory will only have to provide the definitive porcelain-fused-to-metal (PFM) crown restorations for the implant restorations. This system may decrease the overall costs of implant treatment for laboratories, restorative dentists, and patients.
Eliasson and Ortorp (2012) reported on the results of a laboratory study that compared the accuracy of implant analog placement in working casts using the robotic technique of this particular CADCAM system and analog placement using a conventional, pickup impression technique. One acrylic resin master model was fabricated, provided with two groups of three implant analogs. Encode Healing Abutments were mounted on the test side; conventional pickup impression copings were inserted on the control side. Fifteen impressions were made with a vinyl polysiloxane material. Using the digital technology explained earlier, implant analogs were placed by a robot on the test side. Implant analogs were placed on the control side conventionally. The center point of each implant analog fitting surface was measured with a laser measuring machine in the x-, y-, and z-axis, as were also the angular direction of the center axis and the positions of the antirotational hexes. Eliasson and Ortorp concluded that both conventional and robot techniques presented low levels of displacement of the implant analogs in all casts. The test technique was less precise, but the difference in accuracy was small. Both techniques were precise enough for single crowns and short-span, implant-supported fixed partial prostheses.
Howell et al. (2013) also reported on the accuracy of the BellaTek Encode robocast technology as compared to the accuracy of conventional pickup and transfer impression techniques. This study differed from the previous study (Eliasson and Ortorp) in that the implants were placed in a master model nonvertical and nonparallel to each other. Howell and others noted that the CADCAM-generated master casts were less accurate than the casts developed from open-tray impressions in the nonparallel sites. The CADCAM casts were less accurate than the open-tray and closed-tray casts in the parallel sites. Howell and others noted that within the limitations of the study design, the BellaTek Encode technique resulted in master casts that were less accurate than master casts made from traditional open- and closed-tray impression techniques. It should be noted that the manufacturer (Biomet 3i) has long recommended that, for complex cases involving multiple units, master casts should be verified prior to proceeding with fabrication of the restorations or a clinical try-in prior to completion of the restoration is needed to make sure that the restoration fits the implant restorative components accurately and passively.
Baldassarri et al. (2012) reported on the results of a laboratory study that tested the marginal accuracy of three different implant/zirconia abutment connections and one implant/titanium abutment connection. Three combinations of implants with custom-made zirconia abutments were analyzed (n = 5/group): NobelProcera abutment/titanium inserts on Replace Select Tapered TiUnite implants (Nobel Biocare) (NP); BellaTek Encode abutments/NanoTite Tapered Certain implants (Biomet 3i) (B3i); Astra Tech Dental Atlantis abutments/Biomet 3i NanoTite Tapered Certain implants (At). Five custom-made BellaTek Encode titanium abutments/NanoTite Tapered Certain implants (Ti) were used as a control group. All abutments were fabricated with CADCAM. One-hundred and twenty vertical gap measurements were made per sample using scanning electron microscopy (15 scans × 4 aspects of each specimen (buccal, mesial, palatal, distal) × 2 measurements). Analysis of variance was used to compare the marginal fit values among the four groups, the specimens within each group, and the four aspects of each specimen. Baldassarri and others concluded that the implant/titanium abutment connections demonstrated significantly better fits than all implant/zirconia abutment configurations. The mean microgaps were approximately three to seven times larger than those in the titanium abutment system.
The following clinical case presentation illustrates the use of CADCAM custom abutments and a 3-unit fixed partial denture (FPD) to replace a screw-retained 3-unit FPD that failed after 10 years of function.
CLINICAL CASE PRESENTATION
Appointment 1: Initial Examination (3/4 Hour)
A 62-year-old man presented to the author with a chief com plaint, “I have a broken bridge” (Figure 6.11). His history included placement of two 4.1 mm diameter implants (external hex) approximately 10 years previous to this visit. The implants had been placed by an oral surgeon and restored by a general dentist. The patient had retired and moved to the author’s city (LaCrosse, WI, USA). The aesthetic veneer material had fractured. The patient was not sure which implant components had been placed (Figure 6.12).
Figure 6.11 Preoperative clinical appearance of the fractured implant-retained 3-unit FPD.

Figure 6.12 Preoperative radiograph demonstrated approximately 1–2 mm of bone loss around the osseointegrated implants in the right posterior maxilla.

The physical examination revealed an end-to-end occlusion, Type I gingivitis, a normal range of motion, and a dentition in good repair. The implant-retained FPD was screw-retained and appeared to be consistent with the original Brånemark implant system.
Diagnostic Casts
Diagnostic casts were made from alginate impressions (Figure 6.13). They were mounted in centric occlusion, and the occlusal relationships were evaluated in preparation for a new FPD.
Diagnosis
The following diagnoses were established:
This patient’s condition was classified as patient type Class II per the American College of Prosthodontists’ Prosthodontic Diagnostic Index (PDI): moderately compromised based on the skeletal and dental malocclusion, missing three or less teeth in a given quadrant, and minimal periodontal involvement (McGarry et al. 2002).
Figure 6.13 Diagnostic casts mounted in centric occlusion demonstrated an end-to-end occlusion. This occlusal relationship was probably implicated in the fracture of the aesthetic veneer material.

Appointment 2: Consultation Restorative Dentist/Patient (1/2 Hour)
A definitive consulta/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


