9
Tooth Fractures and Traumatic Dentoalveolar Injuries
9.1 Introduction
Dental trauma is a mechanically caused tooth and/or periodontal injury.
9.2 Abuse
Physical abuse may cause oral injury.
9.2.1 Battered Child Syndrome289 (non-accidental injury)24
Every year, 0.35–0.8% children in the USA are physically abused or neglected.358 361 The frequency of abuse varies between countries, cultures and over the time.8 24 At the minimum, half of those abused suffer head and facial injuries, yet two-thirds of American paediatric and even more Dutch dentists claim to have never observed abuse.222 358 405 They profess a lack of knowledge and fear making false accusations.405
Scepticism is required when clinical findings in a child with facial or oral injuries are incompatible with explanations given by parents.232 One should have a high index of suspicion in children presenting with wounds in different healing stages, several healed root fractures, a lacerated upper lip, torn maxillary frenum, oral mucosal lacerations and discoloured teeth.159 289 360 During bouts of anger, force is often directed towards the mouth of the child in an effort to silence him or her. Unscrupulous abusers try to avoid leaving marks. Most victims are younger than 4 years, and are often babies.397 Round burns (cigarettes), burns around the wrists (binding ropes), facial bite wounds, and pulled out hair (forcing down during sexual assaults) are obvious signs of child abuse. Skull fractures and intracranial injuries will be seen in those presenting to hospitals.216 358
Dentists should be suspicious in cases of children who are unable to establish communication, including eye contact, occasionally present with enticing behaviour towards the dentist,405 and children who appear vigilant, or are in a state of frozen watchfulness or show distant or shy interaction with the parents. Long sleeves and high-necked clothes on hot days in the summer may be a cover-up for injuries.232 Abused children may be unwanted (stepchildren) or born after an extra-marital relationship, they may have disabilities, or were born prematurely and were kept in an incubator for some time, which interferes with establishing a bond. When the child with visible injuries attends the dental office, one could consider the list of features in Table 9.1.
Table 9.1 Features of oral injuries in child abuse8
| Injury | |
| Type | Bruises, stab wounds, burns, cuts? |
| Site | Is the injury at a “usual” location? |
| Characteristics | Colour, form/shape. A common injury? |
| Time | Does the appearance of the injury correspond with the reported time of injury? |
| Cause | Does the parents’ explanation correspond with the type, site and appearance of the injury? |
| Previous injuries | Signs of healed wounds and fractures? |
The dentist should consider the following questions: Were there witnesses? Have they come with the child? Have adequate steps been undertaken by the parents/caregivers? Is the perpetrator present? Most perpetrators are 20–30 years of age, emotional, impulsive and immature, and self-oriented with a tendency towards poorly controlled aggressive behaviour. Abusive parents often have a history of being abused in childhood themselves. Poverty, alcohol, drugs and matrimonial problems may play a role.216
9.2.2 Partner and Parental Abuse
Mistreatment of (fe)male partners happens frequently but is often concealed.270 Abuse of parents by adult and teenage children is beginning to draw attention.
Fighting
Alcohol and drug intoxication is linked to assaults in which the maxillofacial region is often the target. In Britain, one-quarter of injuries are due to violence.420
Torture
Orofacial blows, teeth fractured with the use of forceps, oral (and facial) electrical torture cause all kinds of facial/oral injuries.24
Brutal removal of teeth was used as torture in the days of the Roman Empire (St Apollonia, Alexandria, AD249) and was a common medieval practice to punish, for example, heretics.238
The biblical saying “an eye for an eye and a tooth for a tooth” was already practised in Babylon. The Codex Hammurabi (1750BC) decreed that physicians must treat their patients with care: he who knocked out a tooth of person of equal rank must lose a tooth.
9.2.3 Dealing with Cases of Suspected Abuse
Speak separately with the child and parent. Ask specific questions regarding the injury, but avoid angering the parent. Documented findings must be reported to appropriate agencies.
9.2.4 Brain Damage
Referral for a medical consultation has priority when there is evidence of blood or other fluid leakage from the nose or ears (brain damage). The patient may show:
- Problems with walking. Can he or she turn the head in both directions without paraesthesia (cranial nerve damage)?351
- Lethargy, confusion. Decreased consciousness may point to increased intracranial pressure (hypertension, low pulse)361
- Abnormal eye position/movements, double vision, asymmetrical pupil sizes, delayed pupil reaction to a bright light. Can the patient follows a moving finger with the eyes? Can they read?
- Low blood pressure, increased pulse (shock)52
- Nausea/vomiting, inability to swallow
- Breathing problems
- Facial paralysis (touch with cotton wool)
- Hoarse, unclear speech/diction.234 289
Facial bone discontinuities, mobility and pain on application of rotational pressure on the temporomandibular joint and haematomas around the eyes are indicative of fractures.
9.3 Spontaneous Cracks and Fractures of the Teeth
9.3.1 Spontaneous Cracks (Infractions, Craze Lines)
A spontaneous crack is an incomplete fracture that occurs under application of routine masticatory forces or due to parafunctions. The fractured tooth segments are not separated and the depth and direction of the infraction is not clearly known. Posterior teeth in particular, either healthy (one-third or even two-thirds) or not (carious, worn or restored) are prone to cracks when subjected to the lateral component of masticatory forces.53 76 195 379 436 The often encountered mesiodistal infraction propagates deeper with time.72 118 The crack is centrally located or peripherally directed and may lead to complete (cuspal) fracture of the tooth.75
Epidemiology
Persons over the age of 30 are predominantly affected,75 112 119 157 195 379 400 and there are no differences between the sexes.411 Mandibular molars in particular are prone to crack near the lingual cusps,1 43 50 75 76 112 157 195 400 413 because the mesio-palatal cusps of the maxillary molars act like a wedge, pushing the mandibular molar cusps apart.107 195 The oblique ridge protects the maxillary molars against cracks,195 but a few studies have found that these teeth experience cracks more frequently than their antagonists.322 436
A prevalence of 80–100 cases/year in general practice is reported.117 Per tooth the rate varies from 1% to 32%, with cracks extending into dentine.285 323 414 After caries and periodontal disease, spontaneous cracks may be considered the third most frequent cause of tooth loss in older persons,63 157 but this has been noted to be a “subjective impression” due to lack of sufficient evidence.257
Aetiology
Causes and contributing factors are: unexpectedly biting on hard objects (pips, stones), tooth wear, excessive erosion, caries, cavity preparation and endodontic treatment, and bruxism.2 75 119 Changes in the oral temperature can lead to cracking of the enamel of the incisors24 due to differences in the expansion coefficients of enamel and dentine.66 104 366
Little dentine remaining after cavity preparation increases the probability of a crack. Sharp internal line angles in a preparation promote stress concentration related to masticatory forces, which initiates and propagates cracks. Other iatrogenic causes are: non-passively fitting cast restorations that have been forced into place and excessive hydraulic forces during luting; placement of parapulpal pins close to the enamel; restorations with steep occlusal slopes that result in an increase in the horizontal component of masticatory forces; use of high condensation pressures when carrying out an amalgam restoration; and moisture contamination during condensation of a poor-quality amalgam.261 350
Amalgam restorations minimally restore the stiffness of a tooth. Excursive interferences make teeth twice as vulnerable to cracks, and when restored with amalgam, the odds ratio increases to 6.330 Teeth with three-surface amalgam restorations crack more frequently than teeth with two-surface fillings.322 413 Studies have found that over 90% of fractured posterior teeth are filled with amalgam, often a Class II or a broad Class I restoration;114 281 the lingual wall tends to fracture.39 As the cavity floor is deepened and as the cusp width is reduced, cuspal deflection under loading increases considerably. The cracks are more superficial in teeth with large restorations. In healthy teeth, the crack will be deeper and closer to the pulp.199
Dentinal collagen, which is present specially around the pulp, makes the tooth more resilient.231 Endodontic preparation reduces the tooth’s internal coherence and increases the probability of spontaneous cracks developing in posterior teeth, even more so when the final restoration is amalgam.158 175 413 With use of bonded amalgam, 40–60% of the tooth stiffness is recovered.323 Dias De Souza reported that cements lack this property,108 but teeth with amalgam restorations bonded with cement did not fracture.265 Non-vital teeth lack the feedback mechanism that protects against extreme loading: the masticatory force may surpass the resistance of the tooth.306 329
Endodontic treatment leads to loss of some free water188 making the tooth more brittle,306 but this is disputed, as is the claimed loss of collagen cross-linking in the dentine of non-vital teeth.202 316 317 365
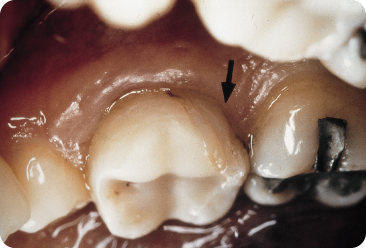
Bonded composite restorations are associated with reduced cuspal flexing. Caron et al. found that teeth with a three-surface composite restoration fractured under a lower occlusal loading and more severely than teeth with two boxed restorations separated by enamel.78 Bonded three-surface composite restorations in premolars help recover the stiffness of the teeth more than bonded amalgam435 and improve their fracture strength.369 However, the polymerisation contraction-shrinkage of the resin deforms the cusps 275 320 and may cause enamel infractions (Figure 9.1) that extend into the thin dentine.403 The volumetric shrinkage starts during the light-curing stage and a loss of 2–3% of the volume occurs by day 1.126 A bonded two-surface composite restoration bends the buccal and lingual cusps by 16 µm and a three-surface restoration by 23 µm, but the cuspal tips bend by 38 (± 44) µm.320 Comparable values have been reported by others.403 Use of a lower intensity light and a two-step curing method with first a low and then high light exposure has been found to reduce contraction stress103 127 without affecting the total volumetric shrinkage.252
Figure 9.1 Cracks in the enamel caused by the setting contraction/shrinkage of the bonded composite restoration.
Vertical Crown-Root Infraction
The probability that cracks extend beyond the epithelial attachment increases the more distally the tooth is situated. Crack progression into the root may split the tooth158 175 (the risk is increased in dentinogenesis imperfecta owing to the low dentine microhardness).24
The shape, size and material of canal posts co-determine success or failure.363 Tapering canal posts, large diameters and use of a large torsion force while inserting threaded posts increase the risk of longitudinal infractions and fractures. Tapered posts cause radicular cracks in the coronal third of the root while parallel posts cause cracks in the apical third,105 324 although use of the latter may be less risky.106 Cast metallic posts are associated with more unfavourable outcomes than glass fibre posts with diameters smaller than the root canal.437 A post must fit passively and be seated with a low-viscosity cement, without rotation, to minimise the hydraulic pressure force.350 Cracks post insertion may not clinically manifest for 1–2 years.105 387 Corrosion expansion of (silver) posts causes longitudinal cracks/fractures.4 34 96 173 253 387
Pilo et al. found that premolars with different types of post showed mainly oblique radicular fractures.324 In another study, the incisors performed equally well with different post-core systems;192 more than 80% survived for 6 years.193 Fibre-reinforced composite posts fail under relatively low loadings, but root fractures are less likely.290
Diagnosis and Appearance
Diagnosing a crack (Figure 9.2) may be difficult. Cracked vital teeth are rarely (about 15%) painful,284 413 but even then often remain undetected or are misdiagnosed as, for example, sinusitis or ear pain.72 75 168 412 A crack in the enamel cannot cause pain, but deeper cracks open minutely under pressure and when they close after cessation of the pressure, the consequent movements of the fluid in the dentinal tubules can cause pain.76 117 Pain elicited by chewing, cold (rarely hot) stimuli, sweet and acidic stimuli (micro-leakage) may represent a dentinal crack (greenstick fracture).75 375 Dentine caries may develop underneath sound enamel when plaque accumulates in deep cracks.407 Cracks extending to the pulp lead to pulpitis. Bacteria colonise subgingivally, and penetrate the cracks giving rise to small, deep periodontal defects that appear on radiographs as diffuse radiolucencies.2 105 412
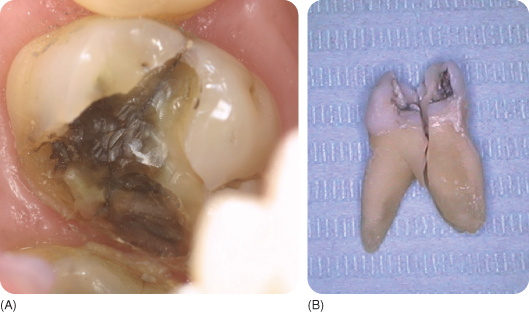
Figure 9.2 (A) Following removal of a large restoration, a dark-coloured vertical fracture line is visible (which is sometimes difficult to see, like in this figure), running from top of the figure to the bottom.
(Courtesy of M. van der Zwet.)
(B) After an endodontic access opening was made in the crown because of pulpitis, a crack was observed in the bottom of the pulp chamber. After extraction and cleaning, the tooth appeared to be totally split.
A sharp short pain when biting on a cotton roll is indicative of a crack.76 117 In spite of the presence of an avoidance pattern during chewing because of the sudden, sharp, lacerating pain, the patient may be unable to identify the involved tooth.261 284 396 Percussion in the axial direction is often inconclusive. Application of lateral pressure on the pertinent cusp may be painful, but pressure applied in another direction will not cause any problem;50 even gentle occlusal rubbing may elicit pain. The pain may become continuous,366 but then disappear when a part of the tooth breaks away.412
Tooth by tooth information may be gained with the use of occlusal biting devices (Tooth Slooth or Fracfinder) or with the application of some polymerised composite on a suspected cusp.274 Cracks are often difficult to observe, including on radiographs,2 unless they run parallel to the X-rays.50 The outline of a crack usually coincides with a groove or fissure. The adjoining teeth impede approximal examination.400 Disclosing solution is not rinsed away from a crack,218 in particular when the crack reaches into the dentine,413 but it does not mark new cracks.117 Transillumination (Figure 9.3; or with the Penlight), meticulous drying and directing light perpendicular to the long axis of the tooth, and use of methylene blue dye, may be helpful.218 256 322 330 Older cracks resemble discoloured grooves, especially in the marginal ridges.330
Figure 9.3 Cracks (the dark line in the right central incisor) may be difficult to see, even with transillumination.
Application of fluorescent oil 8 minutes after polishing shows a yellow-green line at the place of the crack with application of ultraviolet light under a surgical microscope.260
Prevention and Treatment
Cavity preparations must be kept small and shallow, and internal line angles should not be sharp. Steep occlusal cuspal slopes must be avoided during carving of the restoration. When a crack is present, grinding of the cusps is an acceptable provisional measure;3 despite this, however, the food bolus may load the tooth unfavourably.157 A temporary solution to avoid crack propagation, fracture and pulpitis256 is fitting a stainless steel band, which also helps alleviate the pain.117
Endodontic access preparations increase cuspal flexure,316 which may require partial coverage crowns rather than composite restorations.85 Older data on protection offered by composites were contradictory,112 156 263 283 385 410 but contemporary composite systems (and bonded amalgam) seem satisfactory.40 65 174 175 176 323 382 However, bonded amalgam restores the stiffness of the tooth to a lesser degree,323 may debond with time,41 and cyclic loading reduces the shear bond strength progressively.269 All this, together with thermal cycling, nullifies the bonding advantage.59
The adhesive restorative approach in non-vital premolars is promising,236 but the resistance against fractures is reduced within 3 years.175 In vitro studies show that the adhesion of composite systems to dentine decreases with time113 132 181 182 183 184 through hydrolysis and enzymatic degradation.51 52 The longer the observation period, the higher is the noted prevalence rate of fractures.67 The enamel bond may seal and protect the hybrid resin-dentine layer,102 but dentinal fluid flow and diffusion of fluid compromise the bond.
Unstable polymeric hydrogels within hybrid layers leach out, and total etching alters the collagen fibrils.183 184 Partly demineralised collagen became almost completely destroyed by proteolytic enzymes.318 Storage in saline increased nanoleakage with hydrolysis of the bond.250
Long etching times,319 and excessive drying and wetting, increase micro- and nanoleakage.131 Water degrades the bond38 and lowers the bond strength169 of two-step, but not of three-step, dentine adhesives.102
Thermocycling reduced the shear bond strength by 38–50%, depending on the pretreatment of dentine (acid-etching, self-etching, or neodymium:yttrium aluminum garnet (Nd:YAG) laser).203 The microtensile bond strength achieved with the use of a self-etching primer declined after 1 year from 39 MPa to 14 MPa and that of a wet bonding system reduced from 48 to 12 MPa.235
Treatment of an enamel crack in a healthy tooth might be delayed,257 412 but an associated amalgam restoration must be substituted with a bonded composite, a composite onlay or a cast restoration when the crack extends into the dentine.2 86 204 The prognosis may be unfavourable,86 375 but in one study only about 10% of the teeth restored with bonded composite were lost2 and in another study using bonded composite onlays, 7% were lost in 6 years.438 In cases of pulpitis, prevention of crack propagation should be prioritised over endodontic treatment.86
In the past, attempts were made to melt and fuse the cracked enamel segments with laser treatment.287 Not much is known, however, about the quality of the solidified enamel.407
A crack that is visible in the pulp chamber during endodontic treatment makes extraction unavoidable,158 particularly when a pocket is present. Attempts have been made to save such teeth with crowns,392 but bacteria still have access to the periodontium via the cracks in the enamel.
9.3.2 Spontaneous Tooth Fractures
A spontaneous fracture is the separation and loss of a tooth segment due to loading with masticatory forces or parafunctions. Tooth fractures (Figure 9.4) have the same causes as cracks, or a crack may propagate and become a fracture. Such fractures sometimes manifest when chewing soft food, because the fractured part of the tooth becomes incorporated in the food bolus. A cusp or a whole wall of the restoration may be lost after removal of a filling.117 A horizontal fracture is often restorable.86 A vertical fracture poses a serious problem and may require extraction.
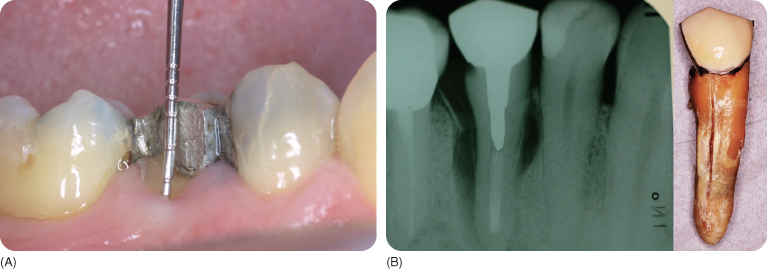
Figure 9.4 (A) Spontaneous cusp fracture; the explorer shows the depth at which the fracture line is located.
(Courtesy of M. van der Zwet.)
(B) Typical radiographic appearance of a vertical fracture (left panel) and the tooth after extraction (right panel). The spontaneous fracture of the root 35 years after treatment was caused by corrosion of the canal post.
Fractures may occur in healthy teeth,247 279 but are more common in decayed or filled teeth, especially after endodontic treatment, in mainly patients younger than 50 years.128 241 Bader et al. reported that of 39 potential risk factors, only the presence of a crack and the amount of dentine supporting the cusps were predictive of posterior tooth fracture. Parafunctions, biting on hard objects and factors such as endodontic treatment, steep cusps and sharp internal cavity line angles were poor predictors.44
Particularly affected are the posterior teeth, except the mandibular premolars.45 82 128 241 The cusps of intact maxillary premolars deflect up to 11 µm under stress; with small two-surface cavities they deflect up to 20 µm, and with extended three-surface cavities the deflection reaches 32 µm.200 The deflection may exceed the resilience of the tooth. The larger a cavity, the more likely it is that the tooth will fracture. A narrow isthmus offers better fracture resistance.114 281 The rate of fracture of functional and non-functional cusps may not be different,241 but centric stops are less prone to fracture than other cusps, especially those in the mandibular molars.82 114 A left/right difference has been noted.258
One per cent of amalgam fillings are replaced due to tooth fracture.7 The estimated fracture rate in Bader et al.’s study was 4.4/100 adults for posterior teeth and 5/100 for all teeth,42 but proportionately more fractures occur. Other authors have proposed an annual rate of some 20 fractured teeth/1000 patients,128 but a rate of 70/1000 has also been reported.43 In the mandible, twice as many lingual than buccal cusps fracture. The opposite has been found for maxillary premolars.44 45 391
In 3–4% of fractures the pulps are exposed and 25% extend subgingivally.44 45 Bader et al. reported that some 3% of fractured teeth had to be extracted.45 The majority of fractures of endodontically treated premolars are located at the base of the cusps.391 If these teeth are crowned, apical transmission of the masticatory forces increases the risk of root fracture.355 Hansen et al. found that only a small proportion of endodontically treated posterior teeth restored with a two-surface amalgam fractured within 3 years versus almost 30% with three-surface amalgam restorations, half of which were extracted within 10 years. Fractures of the lingual cusp caused the most periodontal damage and these are more common in the molars.176
In studies, the presence of an unfilled three-surface cavity halved the fracture resistance of maxillary premolars. Amalgam and composite bonded with one-step and two-step adhesives reinforced the teeth equally; without the adhesive, both materials protected minimally.87 207 391 419 439 The fracture resistance of maxillary premolars restored with bonded composite (inlays) has been found to differ from that of intact premolars; a bonded amalgam performed less well.99 160 440 A ceromer functioned the best.99
Research shows that creep and expansion of amalgam and weakening of the coronal root due to use of Gates Glidden drills in endodontically treated teeth increases the risk of fracture;178 even a composite bonded only to the enamel has a higher survival rate.177 A cast-metal onlay was superior to resin composite onlays or fibre-reinforced composite and ceramics,68 but the failure mode of the former was commonly unfavourable.425
In one study, restorations including the palatal cusp of maxillary premolars with a bonded composite, bonded amalgam or reinforced glass ionomer cement were subjected to axial loading. The teeth with reinforced glass ionomer cement exhibited lower resistance against fracture, but more tooth tissue was retained. Use of dentine pins did not improve the protection.327
9.3.3 Cervical Abfraction (Physical Stress-Induced or Non-Carious Cervical Lesion)
Cervical abfraction lesions are small V-shaped defects with sharp margins that are found mainly on the buccal enamel surface of the permanent teeth, and which may primarily be caused by occlusal forces.
The horizontal component of masticatory forces bends the crown (200–400 µm)385 on the firmly fixed root. Repeated flexures generate alternating cervical tension and compression. The tensile stresses may disrupt the chemical bonds between the hydroxyapatite crystals. Ions and small molecules penetrate the microcracks and prevent re-establishment of the bonds. The flexures cause fatigue, tearing and abfraction of the cervical enamel,164 166 243 244 276 313 and even more so because the interdigitation between the cervical enamel and dentine is relatively weak.161 307 In experimental studies, the maximum principal stresses exceeded the failure stresses for enamel.337 The more elastic dentine better withstands bending.243
The initial phase of development of abfraction lesions may comprise loss of cervical dentine, undermining the enamel. In a finite element study (which involves using a computer modelling technique), an artificially created discontinuity between the cervical enamel and root dentine increased the principal stress upon occlusal loading dramatically in excess of the failure stress rate for the cervical enamel.339
The lesions are characteristically wedge-shaped and located at sites of tensile stress concentration. Erosion, in contrast, results in more disc-shaped lesions.243 249 307 Initially, a wave-like or corrugated pattern is seen on the cervical enamel surface.64 Abfraction occurs predominantly on the buccal surfaces and may occur at an angle toward the mesial or distal,243 because each point along the occlusal plane generates slightly different forces near the fulcrum.293 Lesions also develop approximally, encircle the whole crown, resulting in breaking away of the tooth crown.164 A shift in the fulcrum apically, for instance after occlusal wear or changes in the periodontal attachment, may lead to several stacked lesions.64 239 243 249
Some studies support the abfraction theory, but others do not. Studies supporting this theory are those involving (1) models in which a tooth with piezoelectric transducers is mounted and subjected to loadings, (2) photo-elastic models, in which a tooth made of birefringent plastic after loading shows areas of stress concentration under polarised light, and (3) strain gauge and (4) finite element analysis. These techniques have been criticised.336 441
A tooth mounted in plaster behaves differently from a tooth with a periodontal ligament.308 Photo-elastic teeth have a lower elastic modulus than enamel.336 In computer models, the enamel is considered to be isotropic (all prisms oriented in the same direction), but the enamel is anisotropic. In the anisotropic enamel the load flux is directed especially towards the dentine and in the isotropic model towards the rigid enamel. A more realistic enamel model altered the stress direction and decreased the maximum tensile stresses. The finite model simplifies reality, and thus may result in false conclusions.100
The models illustrate, however, the ability of occlusal forces to cause damage.336 Use of the models indicates that lingual lesions should be present as often as buccal ones, but this is not supported by clinical findings.
During biting, chewing and swallowing, the lower and upper teeth come into contact, but such forces are not usually harmful. Larger forces, which develop during bruxism194 with large horizontal jaw movements271 or tooth clenching,96 or are seen with premature contacts and malocclusion may cause the V-shaped cervical defects.243 337 390 The magnitude, direction and patterns of strain developed on the cervical enamel depend highly on the loading patterns. Point loadings on the outer and inner inclines of cusps results in asymmetrical cervical strains315 and concordantly shaped cervical lesions.155 243 Abfraction does not occur in mobile teeth, due to the absence of a fulcrum. Kuroe et al. found that cuspal loading appeared to concentrate stresses around the cervical region below the loaded cusp, and the stresses were highest under buccal cusp loading,239 the site where the majority of the abfractions occur. Almost all teeth with abfraction in one study showed coronal wear facets, canine disclusion was common and balancing interferences were present in one-fifth of the teeth.277 Progression of occlusal and cervical tissue loss were strongly associated.325
The lesions develop chiefly in the maxillary and mandibular premolars,121 but the commonest sites seem to be: (1) labial surfaces of the maxillary incisors, (2) buccal surfaces of the maxillary premolars and (3) the labial surfaces of the maxillary canines. Rees et al. found that peak local and peak principal stresses seemed, indeed, highest in the maxillary incisors, intermediate in the maxillary first premolars and lowest in the maxillary canines.338 When one of two adjacent premolars is affected, abfraction seems likely. Erosion and tooth brushing may be the principal causes when both premolars show lesions. Acidic attacks accelerate the loss of cervical tissue.165
Bending generates a small piezoelectric charge between the dentinal regions, which may be attributed to “stress corrosion”, i.e. loss of tooth material.166 Piezoelectricity may cause enamel demineralisation or the cyclic changes can attract and repel charged erosive agents.
The lesions may be multifactorial249 307 or multicausal 277 309 and abfraction may not be the primary cause.255 Currently there is insufficient evidence to be absolutely certain of the cause.441 Occlusal forces might be major contributors, but are unlikely to be entirely responsible for the defects.262 The association of cervical abfraction lesions with occlusal forces does not necessarily support a causal relationship.25 45 Bader et al. found that, from a number of factors investigated, forceful brushing three times/day, starting on the buccal sides, bruxism, drinking fruit juice more than once/day, and a low salivary buffering capacity were separately associated with cervical lesions. Interactions between these factors were almost nil.46 Subgingival lesions exclude tooth brushing as a cause64 and wedge-shaped lesions likely develop under the influence of another factor.309
Epidemiology
In Dawid et al.’s study, some 50% of pilots had cervical abfraction lesions versus about 10% of other air force personnel. The authors concluded that tooth clenching under stress could have be responsible. The pilots were older than the controls, but age did not seem a decisive factor.96 However, in another study including mostly bruxists, older persons had more defects than younger people. Most patients were bruxists.162 In a Nigerian population, one-third of cervical defects were found to be abfraction lesions, associated with occlusal wear facets.295 Although abfraction should be more frequently present in teeth with occlusal wear than in those with occlusal erosion, this was not found to be the case in another study.226
Prevention and Treatment
Occlusal adjustment reduces cervical stress. The tensile stresses may lead to debonding and loss of cervical restorations, for which reason microfilled composites that flex with the tooth are preferred to stiffer ones.194 244 A thick layer of a flexible liner and mechanical retention are recommended. Abrasive/erosive lesions are preferably restored with composites resistant to wear.244 Dentists should consider erosion in the diagnosis and treatment of non-carious cervical lesions,226 but abfraction must be kept in mind as a primary cause.
9.4 Traumatic Tooth Fractures
An external force may fracture the enamel and/or crown dentine or the root. Precise registration and history taking of the injury is essential for evaluation and medicolegal and financial reasons. Information must be gained regarding general health and use of medicaments that may affect the treatment, such as presence of blood coagulation disorders, immune system deficiencies, diabetes mellitus, acute rheumatism, epilepsy, allergies and heart diseases.
Based on the aetiology, pathology, etc., several classifications of tooth fracture have been proposed.24 142 The classification by Andreasen and Andreasen24 has been adopted by the World Health Organization and is also followed here. The guidelines presented in this chapter for the management of traumatic dental injuries are in accordance with those of the International Association of Dental Traumatology.442 Recent guidelines can also be found at www.dentaltrauma.guide.
Pulp survival and healing after crown fractures with and without pulp exposure depend on the developmental stage of the root and damage to the apical blood supply.345 Traumatic forces transmitted to the periodontium may damage the periodontal tissues. Dental injuries are treated on an emergency basis, but limited evidence suggests that a treatment delay of 24 hours has no serious consequences for crown and root fractures27 and intrusion.443 The risk of fracture is greater in adults than in children, who are more likely to experience tooth displacement because of their more resilient alveolar bone and incomplete (thus shorter) tooth roots.24 36 60 251
Each case of dental trauma should have radiographs and sensibility tests for obtaining information regarding pulp cavity size, root development, root fractures and other injuries. However, immediately after trauma the pulp may not react due to transient pulp damage. Sensibility may return88 347 after 6–10 weeks,332 431 sometimes even after years.11 At 3 months, some 80% of pulps of traumatised teeth will react.444 It is worth bearing in mind that non-traumatised immature teeth may not react to sensibility testing.139
The pulp can become necrotic after some time.11 332 352 431 Radiographs and sensibility testing of permanent teeth are repeated after 6 weeks, 6 months, 1 year and, for fractures, 5 years,442 to check for resorption, periapical granuloma formation, pulp obliteration, absence of secondary dentine formation and cessation of root development. A yellow discolouration of the crown points to pulp obliteration, a grey-blue to black colour signifies a necrotic pulp, and a pink spot signifies internal crown or cervical resorption (Chapter 7). Immature teeth may also temporarily appear pink.10 11 Most traumatised deciduous teeth are assessed clinically after 1 week, 6–8 weeks and 1 year (clinically and with radiographs at both follow-ups), and root fractures and intrusive injuries are also assessed at 2–3 weeks and 6 months.442
After an injury, the patient should brush with a soft brush and rinse with 0.1% chlorhexidine.442
9.4.1 Crown Infraction
Traumatic crown infraction is an incomplete fracture (crack) in the enamel and/or dentine caused by an external force, without separation of the segments.24 Infraction, usually limited to the enamel,24 occurs in about 10% of teeth affected by trauma,332 and most commonly in the permanent maxillary anterior teeth. Infractions into dentine, in, for instance, maxillary premolars, are caused by a blow to the chin. The infraction may be difficult to see.
Treatment
The prognosis is usually favourable.331 An infracted anterior tooth does not need treatment, unless the tooth is heavily loaded functionally, in which case grinding is indicated. The crack may be sealed with an unfilled composite to prevent staining.24 Pulpitis develops in 0–3.5% of cases.24 332 A part of the tooth may fracture between dental follow-ups.
Deciduous Teeth
Crown infractions of deciduous teeth are rare. A grey discolouration that becomes yellow in 75% of cases60 is indicative of pulp obliteration, and a grey-blue to black discolouration is due to pulp necrosis.362 With respect to the sequelae of the injury, it does not matter whether dark discoloured deciduous teeth are endodontically treated or not.445 Where pain develops, o/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


