4
Deviations in Timing and Site of Eruption
4.1 Eruption
4.1.1 The Eruption Process
Eruption is defined as the act of emergence of any part of a tooth into the oral cavity. However, in practical terms, eruption includes the entire axial movement of a tooth, from the movements during odontogenesis267 in its crypt to when it makes contact with its antagonist(s), and the axial movement thereafter to compensate for tooth wear. The eruptive process is influenced by several factors including the growth of the face, jaws and alveolar height.
Pre-eruptive movements start after initiation of root formation, even prior to calcification. Previously, root growth was incorrectly43 63 220 considered to deliver the eruptive force. However, teeth without roots or those with extremely short roots due to radiotherapy,197 481 congenital kidney disease63 or due to surgical root removal also erupt. The developing root even penetrates 2–4 mm further into the surrounding bone, without any eruptive movement.271
It has been suggested that the eruptive force could be delivered by the periodontal ligament itself.284 The ligament fibres are rapidly renewed and remodelled by the local fibroblasts267 and might be responsible for eruption. However, in humans, this might hold true after emergence,271 but before that time the tooth–alveolus connection is incomplete and there are too few fibres,240 and thus the mechanism of eruption may be different from that of rodent incisors which erupt continually throughout life.72 Microtubules in the periodontal ligament may be involved in eruption,33 but evidence is lacking and results of experiments are confliciting.72
Cells in the dental follicle and possibly in the periodontal membrane are targeted by the epidermal growth factor and other hormones (such as growth hormone), which initiate several cellular processes including cell differentiation and DNA synthesis in the ligament fibroblasts.385 416 A pushing force, instead of traction, is generated in the periodontal ligament, due to a hydrostatic pressure gradient in the periodontal ligament and the interstitial fluid. Blood vessel permeability is altered under the influence of growth hormone, which controls the secretion of insulin-like growth factors.
The pre-eruption path of the tooth lies within the gubernaculum dentis, a narrow sheath of soft tissue within the bone.72 Resorption of bone and eventually the roots of the deciduous teeth broadens the path. Increased secretion of enzymes such as hyaluronidase and gelatinase,352 cytokines such as interleukin-1430 and other regulatory molecules for osteoclastogenesis501 are required for the breakdown of the tissues ahead of the erupting tooth.72 220 271 Calcitonin inhibits osteoclastogenesis and may have anti-eruption properties.502 The dental follicle contains monocytes and chemotactic molecules necessary for the formation of osteoclasts, the bone resorbing cells.486
The number of monocytes in the coronal part of the dental follicle increases proportionally to the number of the osteoclasts.487 Tooth germs transplanted to elsewhere in the jaw erupted when the dental follicle was left intact in experimental studies but if there was follicular damage the teeth did not erupt.224 Thus the dental follicle may be essential for eruption,71 but signalling molecules in the stellate reticulum may act as factors controlling the timing of eruption through their interaction with the dental follicle, and may also possibly initiate the eruption.486
After emergence into the oral cavity, the eruptive movement continues until the tooth makes contact with its antagonistic(s). The tooth moves at night in the direction of the antagonist(s), about 4 mm within 14 weeks. During the daytime, in particular during breakfast and the mid-day meal, a small apical movement takes place.240 Risinger et al. found that from 20:00 to 24:00 hours, premolars moved 65 µmm orally, in cyclic eruptive rhythms of 20–50 seconds, and between midnight and morning they intruded 33 µmm.385
Shifts in the position of the teeth and their sockets occur to compensate for the growth of the face. For example, between the ages of 9 and 25 years the permanent maxillary incisors move some 6 mm downwards and 2.5 mm labially.195 After the age of 16, vertical movement diminishes and the displacement occurs mainly in the horizontal plane.196 An active spurt of movement occurs during puberty.425 As mentioned above, minimal eruptive movements continue to occur after establishment of occlusal contact to compensate for tooth wear.482 In the absence of involvement of a tooth in mastication, eruption continues, whereby the epithelial attachment of the tooth comes to lie on exposed cementum.302
4.1.2 Timing of Eruption
Most teeth emerge when half to three-quarters of the final root length is achieved.29 155 There is marked variation in the timing of eruption of individual teeth with respect to chronological age. Mean eruption times can be determined retrospectively or prospectively. With the case–control method, large groups of children of different age cohorts are examined to record which teeth are erupted, although a cohort effect or a period (calendar year) effect may introduce bias.328 The physiologic eruption timespan of a tooth may be arbitrarily defined, for instance as the mean ± 3 × SD (standard deviation). An eruption time outside this is by definition delayed380 or accelerated. The standard deviations for the emergence times of individual teeth differ.189 In practice, the time periods and eruption sequence shown in Table 4.1 may be used, although these will differ considerably by country and population.
Table 4.1 The sequence of eruption and time periods within which the deciduous and permanent teeth erupt
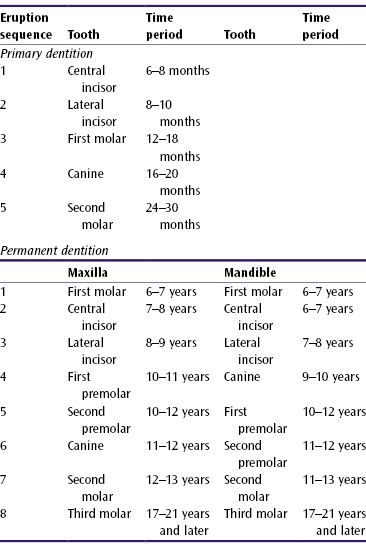
Deciduous Dentition
A sex difference is absent in the maturation and the eruption times of the deciduous teeth.215 297 Earlier eruption both in boys111 323 441 and girls104 has been recorded, but may apply only to the maxillary lateral incisors and mandibular canines.160 One has to take into account that eruption patterns vary between individuals as they are (weakly) correlated with factors such as birthweight, increase in weight after birth (in boys), birth order, mother’s age at time of conception and body length (in girls). Maternal smoking in particular has been shown to retard dental maturity and eruption.194 210 215 323 440 A weak association between head circumference and number of emerged teeth increased greatly when comparing children below the 25th percentile with those above the 75th percentile (Yule’s coefficient of association (Q) = 0.6 for boys and 0.4 for girls).194 Hypodontia is clearly accompanied by delayed development of the dentition,34 147 179 356 as are congenital clefts of the lip, jaws and palate.355 376
“Teething”, i.e. the eruption of especially the deciduous mandibular and, to a lesser degree, the maxillary central incisors (23%), and occasionally other teeth,91 is accompanied by several symptoms. Parents reported gingival itching (85%), agitation (74%), dribbling (70%), fever (46%), disturbed sleep (39%), diarrhoea (35%) and runny nose (26%). Proteins of the degrading enamel matrix act as antigens and cause an auto-immune response.343 However, systemic symptoms such as fever and diarrhoea are absent.
Permanent Dentition
The eruption times of the deciduous and permanent teeth correlate moderately (in the order of r = 0.40), but more so between first permanent molars and the second deciduous molars (in the order of r = 0.70).260 At observations made at three different ages, a sample of Finnish girls had more erupted teeth than boys;327 the tooth-dependent difference ranged from 0.1 to 1.0 year.475 In a longitudinal study, the difference in eruption times of the individual teeth was 2.5–14 months.160
The interval between two check-ups in a longitudinal investigation may, for instance, be 1 year. 475 If a tooth erupts between check-ups, one only knows that the tooth emerged within that year, which is not very accurate. One may then assume that the tooth erupted at the midpoint of the yearly interval, but such an assumption may give rise to bias. This disadvantage may be overcome by use of appropriate statistical methods.328
Variations in the mean eruption times in different studies are due to sex, sample, age and country differences at the time of observation.358 A variation of 15 months related to sex has been found for all permanent teeth.170 It has been shown that at 5–6 years of age sexual dimorphism is absent.245 Per tooth, girls aged 6–12 years are a few months in advance of boys, more so for the (mandibular) canines.151 152 245 260 264 327 At 8 years, tooth mineralisation in girls is ahead, reaching its peak at 13 years,186 but the third molars erupt earlier in boys.245 According to some researchers, there are no sex differences in the eruption times of the individual teeth.67 251
As mentioned above, eruption times also vary between individuals,67 169 ethnically and geographically. A 1.5-year advance in eruption noted in sub-Saharan Africa may have been due to errors in the data,352 but more recently the mean eruption times of third molars in Nigerian females was noted to be 13 years and in Nigerian males it was 15 years.322
The eruption of the permanent dentition is also influenced by presence of caries in the deciduous teeth,1 449 but this effect is now seen less often due to the general decline in the prevalence of caries. In the 1980s, permanent teeth erupted 4–5 months earlier than in 1934,185 256 and in 1965 (in Denmark) earlier than in 1913,178 a secular trend comparable to an increased body length and earlier onset of the menarche (which, however, weakly correlates with eruption times).207 In France, a trend has been noted for later eruption of the maxillary premolars and earlier emergence of permanent second molars.391 Today, many children mature at a younger age than 50 or 100 years ago, they are growing faster and have increased stature, all of which seem to be associated with accelerated eruption.186 328
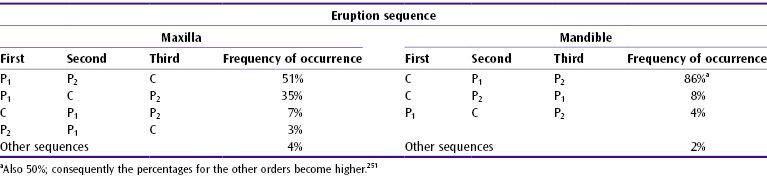
Sequence of Eruption
Several sequences of eruption have been reported (Table 4.2), deviating from that presented in Table 4.1.170 251 The eruption sequence of the maxillary second premolar and canine is changing (Denmark, USA, France).328 391 478 In a sample of boys in New York, the mandibular second premolar was found to erupt after the second molar.478 In Finland, the mandibular central incisors presently emerge before the first molars in 68%.311
Table 4.2 Sequence of eruption of some permanent teeth170
Chronological Age, Dental and Skeletal Maturity
The intellectual and physical burden in, for instance, orphans will be too heavy if their age is estimated to be older than they actually are and they will lack exposure to appropriate challenges if estimated to be too young. Age when not known is estimated on the basis of the degree of ossification of the bones such as the hand and wrist. Another possibility is to use the level of dental maturation. One scoring method (Demirjan, 1973) is based upon eight stages of calcification seen on radiographs of the seven left mandibular permanent teeth (the third molar is excluded).110 The eight stages are related to skeletal development. For example, in stage eight the mandibular canine root apex is closed and the epiphyses of the long bones are fused with the diaphyses.90 With the seven tooth scores, the dental age is determined, using conversion tables for sex, 109 110 because a French-Canadian study noted that after the age of 7 years, girls were more dentally mature than boys.111 The reference group data appeared invalid for other populations. A modified method has resulted in a better fit.445
Correlation between the skeletal age and dental maturation in different age categories is reported to be low (r = 0.2–0.4).108 177 358 Even in one study which showed high correlation (r = 0.59), this was not high enough to substitute the age determined by skeletal maturity with that determined via dental estimation.396 The calcification of the mandibular canines probably correlates better (and that of other teeth less) with specific ossification areas in the hand bones.90 418 In a few towns or countries, some children of known age were estimated to be older based on dental estimates and others younger, 121 249 269 308 310 446 whereas use of skeletal maturity led to more correct estimates.269 A large impact of environmental factors on dental maturity may explain differences between children with the same ethnic background. Genetic factors may explain racial differences. 338 The remains of eighteenth and nineteenth-century British children of known age were used for dental estimation. Several of the younger children were dentally delayed, their dental age being below the lowest limit of the scale (2.5 years).250
Other dental-based methods have been developed,288 requiring the assessment of fewer teeth.57 257 290 A study of one of these methods288 in monozygotic and dizygotic twins revealed that variation in dental age was best explained by additive genetic influences (43%), environmental factors common to both twins (50%) and specific environmental factors that were not shared by both.338
Age estimation via different dental-based methods by different observers using identical radiographs had very diverging/differing results.382 One method led to age estimations that were too high and two others to age estimations that were too low. The 95% confidence interval (for Demirjian’s method) for individual age estimation exceeded 15 months,100 2 years,290 308 421 and 3 years.121
Compared with Caucasians, the eruption is accelerated in the Bantu and delayed in autochthonous Australians.345 Dental maturity110 and eruption times136 show varying degrees of correlation.358 Methods to assess dental maturity are not interchangeable.311 The independent physiological determinants177 “dental age” and “skeletal maturity” are used to find as precise as possible the age of war orphans and adoptive children.137 Some researchers prefer solely the use of skeleton maturity for age estimation177 while others prefer dental maturity. Marked differences between individuals and populations make the estimation of the chronological age based on the dental development precarious.
4.2 Abnormal Eruption Times
Beyond the physiological variations, the eruption of the deciduous and permanent dentition may be accelerated or retarded and teeth may not erupt or only partially erupt. Eruption delays are more common than acceleration.430
4.2.1 Pathologically Accelerated Eruption
Pathologically accelerated eruption occurs when one or more deciduous or permanent teeth emerge at a younger age than expected on the basis of eruption times or the stage of root development.
Deciduous Dentition
Local Factors
- Natal and neonatal teeth. Teeth erupted at or around birth are described in Chapter 1. A superficially located tooth germ seems the likely cause.
- Early teething (dentitio praecox). Many or all deciduous teeth erupt prematurely, probably again due to superficially located germs. The precocious dentition may be familial.345
General Factors
- Fever. Infectious diseases with fever may be associated with early eruption of some teeth, but some teeth may erupt later than normal.345
- Syndromes. Premature eruption is linked to a number of syndromes (Chapter 11), including oral clefts (Figure 4.1).
Figure 4.1 Neonatal tooth in a child with cleft lip and palate.

All deciduous teeth had erupted (except second molars) in a child aged 11 months with three copies of chromosome 8,342 and in a 4-month-old child with Letterer–Siwe disease (involves proliferation of the macrophages that is fatal).9
Permanent Dentition
Local Factors
Early Loss of Deciduous Teeth
When a deciduous tooth is lost earlier than its normal exfoliation time, for example due to caries requiring extraction of the tooth,185 accelerated root resorption345 or trauma, the successor tooth’s eruption is accelerated. There are reports of premolars having emerged prematurely when the predecessors were extracted less than 2 years before their exfoliation time.93 351 Others have found both delayed and accelerated premolar eruption,73 except in the mandibular premolar-canine region.207 Early eruption requires that the space available for the successor is of normal proportion. Delayed eruption of usually the mandibular second premolar and the maxillary canine occurs when the space is too small,207 due to drifting and tilting of the adjacent teeth into the space.306
Rural Maasai (Africa) traditionally removed the tooth buds of the deciduous canines, because febrile illnesses in childhood are believed to be caused by the swelling over the canine region, which was thought to contain “worms”. The removal did not affect the eruption time of the successors, which may, however, be damaged.171
Emergence of the premolars was reported to be accelerated by 4–8 months and 2–4 months in boys and girls respectively, when their predecessors were decayed and restored.244 Pulpotomy of a deciduous molar may accelerate the emergence of the successor,239 320 but delayed exfoliation is reported too. Caries, pulp necrosis and pulpotomy hasten the resorption of the deciduous roots, but not the rate of root growth of the succedaneous teeth.164 However, in a 6-year-old with erupted mandibular canines, root development was similar to in a 13–14-year-old,303 while erupted premolars in other 6-year-olds were reported to be mobile because of insufficient root development.73
Extraction of deciduous molars with abscesses and resorbed alveolar bone accelerate the emergence of the succedaneous tooth regardless of its developmental stage,73 in a buccal or lingual direction, with the tooth taking the path of least resistance.189
Prepubertal Periodontitis
Deciduous teeth exfoliate prematurely due to aggressive (formerly called early-onset pubertal)503 periodontitis,325 463 which is not necessarily followed by an accelerated eruption of permanent teeth.22 Extraction of the very mobile teeth and scaling with subgingival chlorhexidine irrigation of other teeth in a 5-year-old girl was followed, until the age of 13, by mobility and root resorption that led to extraction of all permanent teeth.463
Juvenile periodontitis may be present in otherwise healthy patients. Curettage and antibiotics have been advised if the process starts at the age of 4 years around a few teeth. Symptoms are local gingival recession and bone resorption, but without root resorption and gingival inflammation. A generalised, rapidly progressive process starts early in the mixed dentition with acutely inflamed gingiva. Abnormal leucocytes are also reported. Afterwards, the permanent dentition may show severe periodontitis.325 326 The pulp cavities of the teeth may be large, with abnormal cementum and root resorption.326
The roots of deciduous teeth in “prepubertal” periodontitis show bacteria within the dentinal tubules or in the cementum. The cementum is either normal, wider than normal or hypoplastic, and both resorption and repair are evidenced. Suprabony root surfaces exhibit resorption lacunae, calculus and colonies of heterogeneous bacterial populations.45 Permanent teeth of subjects with prepubertal periodontitis had thicker cementum and were infiltrated by microorganisms compared with the teeth of 50-year-old healthy controls. A cuticle may cover the cementum in prepubertal periodontitis, which is not seen in adults with periodontitis.255
General Factors
- (Facial) hemihypertrophy. Eruption is advanced by 4–5 years on the side of the face showing ovegrowth.34
- Mercury poisoning. Early exfoliation of deciduous teeth and breakdown of periodontal tissues was described in a 15-month-old child exposed to mercury in the house of a former gold miner. The miner routinely used mercury to extract gold from ore and boiled away the mercury condensed on the walls and floor.272 Mercury is still used to extract gold from sand obtained from rivers. In the past, mercury caused early loss of permanent teeth in mercury miners, mirror makers and workers in the felt-making industry (“mad as a hatter”).
- Precocious puberty (pubertas praecox). When puberty starts prematurely due to central or peripheral disturbances, all permanent teeth erupt early. Central disturbances may have several causes including idiopathic ones and premature activation by tumours of the hypothalamus. An example of a peripheral cause is a gonadal tumour. Medroxyprogesterone medication for idiopathic precocity is associated with accelerated root development and eruption.77 Slightly advanced tooth development148 and definitely advanced root formation has been confirmed in cases of precocious puberty not on medication.205 Odontogenesis is retarded in idiopathic precocity and but proceeds normally when other causes underlie premature puberty.388
- Syndromes. Eruption is accelerated in cases with syndromes (Ellis–Van Creveld, Hallerman–Streiff, pachyonychia congenita, Sturge–Weber, etc.). In the Klippel-Trénaunay syndrome (which includes unilateral bony and soft tissue hypertrophy) the permanent teeth erupt prematurely on the affected side of the jaw.293 Although dental maturity seemed to be delayed by more than 12 months in about 20% of patients with osteogenesis imperfecta type III and accelerated in as many of those with osteogenesis imperfecta type IV, the eruption times of the deciduous and permanent teeth were normal, but in some subjects the permanent second molars emerged late.314
- Systemic diseases. Hyperthyroidism leads to thyrotoxicosis, which is accompanied by tachycardia, hypertension and accelerated tooth eruption.346 In advanced cases the deciduous teeth are lost from atrophied alveolar bone and the permanent teeth erupt early.408 Well-controlled diabetes does not influence eruption. In uncontrolled diabetes, there is accelerated exfoliation of the deciduous teeth and eruption of the permanent teeth, but long-standing diabetes delays the eruption of permanent teeth.2 56 The effect in the mixed dentition period is probably mediated by the pituitary gland, which is stimulated in the initial stages of the disease but in then becomes exhausted in juvenile diabetes of longer duration, the reasons for which remain unclear.56
- Systemic diseases and syndromes with juvenile periodontitis. Premature loss of a few or all deciduous teeth, possibly followed by accelerated eruption (and loss) of permanent teeth, may occur in many diseases168 281 285 that compromise the host response and cause periodontitis. Examples are acute lymphocytic leukaemia (leucocyte proliferation and hyperplasia of lymphoid tissue), cyclic neutropenia (decreased number of neutrophilic leucocytes), histiocytosis X (abnormal macrophages), acatalasia (absence of the enzyme catalase), haemangioma and lymphangioma.
Several syndromes are associated with prepubertal periodontitis and early tooth loss. Chediak–Higashi syndrome is characterised by oculocutaneous albinism, abnormal neutrophils, respiratory system and skin infections, and severe gingivitis.168 285 Antibiotic treatment proves ineffective.504
Papillon–Lefèvre syndrome is characterized by hyperkeratosis of palms and soles and early, rapid, destructive periodontitis. The prematurely lost deciduous teeth are replaced by the earlier erupting permanent teeth.174 Antibiotics and extraction of the deciduous dentition followed by a period of edentulism seem effective in preserving the permanent dentition.138 Extraction of teeth with poor prognosis and conventional periodontal treatment improve the condition,359 although edentulism in a 12-year-old affected child has been reported.174 The crevicular fluid may not show clear-cut pathognomonic expression of cytokines and matrix metalloproteinases.459
- Tumours, inflammation. Accelerated loss of the deciduous teeth, even starting at the age of 1 year, may be caused by malignant and benign neoplasms and osteomyelitis.22
4.2.2 Pathologically Delayed Eruption
Pathologically delayed eruption is the emergence in the mouth of one or more teeth of the deciduous or permanent dentition at a later age than expected on the basis of published mean eruption times. Delayed eruption is more common than early eruption and has many more causes. Alternative terms are late, retarded, depressed, impaired, (primary) retention, primary/idiopathic failure of eruption, impaction, embedded teeth, and pseudoanodontia;430 some terms have a specific meaning and will be defined later.
Deciduous Dentition
Dentitio tarda occurs when a deciduous tooth erupts 6 months later than it does on average.166 171
Local Factors
- Gingival fibromatosis and hyperplasia. After dental trauma/surgery, the follicle of an erupting deciduous tooth may not merge with the overlying mucosa, which also does not break down (or this is delayed). Gingival hyperplasia with dense connective tissue may act as a barrier: hormonal and hereditary causes, vitamin C deficiency and use of drugs such as phenytoin are underlying causes. In general, mucosal barrier will be more likely to cause delayed eruption of permanent rather than the deciduous teeth.430
- Hyperdontia. In hyperdontia, the eruption of the regular teeth may be delayed (Chapter 1). Odontomes,163 tumours and morphological aberrations such as double teeth occasionally delay the eruption of deciduous teeth, and this may be the first sign of the underlying abnormality.430
- Prematurely born children. Low birthweight is related to eruption delay of the deciduous teeth,404 405 and the permanent dentition lags 3 months behind. However, the differences between these children and children born at term are negated when age adjustments are made for prematurity: that is, 6-month-old children born 2 months too early must be compared with children aged 4 months.406 Subsequently, there are no differences in between the groups in “teething” or maturation of the permanent teeth.24 Eruption seems delayed until 18 months after birth. Thereafter, during infancy, catch-up is observed. By age 9 the delay has been compensated.405 406 Significantly accelerated eruption of permanent incisors and first molars is possible in the prematurely born due to the influence of catch-up growth and related factors.165
General Factors
- Dietary deficiencies, inclusive hypovitaminoses. Nutritional influences on eruption are minor compared with other factors, but extreme nutritional deprivation and intra-uterine growth retardation markedly delay the general development of teeth and eruption.3 64 127 381 399 430 Vitamin C deficiency causes scurvy, a “gingivitis” that results in premature shedding of the deciduous teeth. Insufficient vitamin D causes retardation;379 dietary intake of minerals or vitamin D in very young children does not affect the maturation of the deciduous dentition.24
- Endocrine disorders. Growth retardation in familial hypoparathyroidism,146 347 cretinism (hypothyroidism in infancy) and hypopituitarism is associated with retarded dental development, and that of the skeleton lags even further behind; (over)treatment also has an impact.148 296 Due to absence of functional “type 1 parathyroid hormone related protein” and its receptor during tooth development, the whole tooth becomes enclosed within a bony crypt because of lack of bone resorption around the tooth crowns, and non-eruption.489
- Heredity. The deciduous and permanent dentition emerged late in siblings in one family despite normally developed teeth. The family reported the condition in previous generations.379 Ethnicity also has an impact on the eruption times.345
- HIV. Paediatric human immunodeficiency virus (HIV) infection is accompanied with eruption delay. The mean number of erupted deciduous teeth is normal up to the age of 2, but it then plateaus and thereafter decreases in both dentitions depending on the clinical symptoms of the disease.374 In one study, the severity of clinical symptoms but not that of T-lymphocyte depletion appeared strongly associated with a retarded eruption in children aged 5 months to 13 years.175
- Hypophosphataemia. Eruption is possibly delayed, but deciduous teeth also exfoliate early, at the age of 18–28 months,168 because of rapidly destructive periodontitis.503 At what age the permanent teeth erupt in these cases has not been reported.
- Hypophosphatasia. In this condition, the paediatric skeleton fails to mineralise properly and the eruption of the deciduous teeth is delayed.262 It is a rare (1 : 1 000 000, an underestimation), autosomal recessive and dominant metabolic disorder with alkaline phosphatase deficiency, reduced phosphatase activity in the cells and increased urinary excretion of phospho-ethanolamine. Deposition of bone following resorption is defective. Phosphate ions precipitate on the tooth roots due to supersaturation.32 Alkaline phosphatase protein may be abnormal.187 The (anterior) deciduous teeth shed very prematurely, with or without root resorption following resorption of the alveolar bone and gingival recession. The permanent teeth may also be lost early. In neonatal hypophosphatasia, the cementum is hypoplastic or aplastic in young children, if they survive to this age.52 58 66 168 187 243 257 319 In one family, children with exfoliation of the deciduous incisors and canines as early as at 1.5 years of age had symptoms of hypophosphatasia, but localised prepubertal periodontitis could not be ruled out.22 Some children reported to have prematurely lost part of the deciduous dentition had normal dentitions 15 years later,243 with large pulp cavities and possibly hypocalcified enamel;58 262 in one report the enamel was reported to be black.262 When the disorder manifests after infancy, the first symptom is loss of the teeth, followed later by bone fractures.52 The roots of the lost teeth are resorbed.126 In patients requiring extractions in the deciduous dentition, a more conventional approach could be attempted.285 Adults with the disorder may be either asymptomatic or have osteomalacia, like in vitamin D deficiency, with soft bones due to impaired mineralisation. Collagen fibres may not attach to the defective cementum,66
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


