CHAPTER 9
Sandwich Osteotomy Bone Graft in the Anterior Maxilla
We constantly begin all over again.
—Michael de Montaigne
The surgical reconstructive solution for moderate to moderately severe bone loss of the anterior maxilla has undergone numerous permutations in the quest to recover esthetic orthoalveolar form, most of which have fallen short. Surgeons are constantly modifying their treatment approaches to overcome failed techniques, including guided bone regeneration and block bone grafting. The use of the interpositional bone graft, the so-called sandwich osteotomy, is the latest effort at trying to solve significant vertical maxillary defects. This use of an interpositional graft after osteotomy manipulation of residual alveolar bone is another new beginning for the dental profession. The technique, first used 30 years ago to gain denture-bearing support in the mandible, is now becoming widely used to increase bone mass to allow esthetic implant reconstruction in the maxilla.
 Surgical Treatment of Bone Loss
Surgical Treatment of Bone Loss
The field of dental implantology has expanded treatment options for partially edentulous patients. Regenerative techniques have the capability to re-create normal function and esthetics. One of the greatest challenges in restorative dentistry, however, is the restoration of maxillary anterior esthetics. Although endosseous dental implants are an option, extensive bone loss in the maxillary anterior region complicates implant placement. Exposure of screw threads is common, necessitating the use of guided tissue regeneration, but if there is extensive resorption in a vertical direction, guided bone regeneration and esthetic implant insertion are impossible. Restoration of the markedly atrophic anterior maxilla is best solved in this setting with an interpositional bone graft.
Revascularization is the key factor for successful incorporation and remodeling of a bone graft. The revascularization process depends on the host site. Surgery should preserve the local blood supply.
The choice of graft material is also important.8 Although intramembranous bone grafts may experience less resorption and show better incorporation9–11 than endochondral bone grafts,12 microarchitectural determinants of the volume maintenance of bone grafts vary. Intraorally harvested bone grafts have the advantages of a relatively short operative time, less donor site morbidity, and lower cost.13,14
Many other variables affect the success of bone grafts. Recently, better maintenance of the bone height of grafts that were placed in combination with a barrier membrane was documented.15–20 Onlay bone grafting has been advocated for vertical and/or transverse deficiency of the maxillary edentulous alveolar ridge, but the failure rate of vertical augmentation is significantly higher than that of horizontal augmentation.21 One limitation in the treatment of severe defects is insufficient soft tissue to adequately cover a block bone graft. When defects are severe, distraction osteogenesis is used to provide a scaffold for later hard tissue grafting and soft tissue histogenesis needed to cover the definitive graft.
Block grafting
The most common augmentation approach, onlay bone grafting, is a complication-prone technique that is often inadequate for correcting the presenting defect.
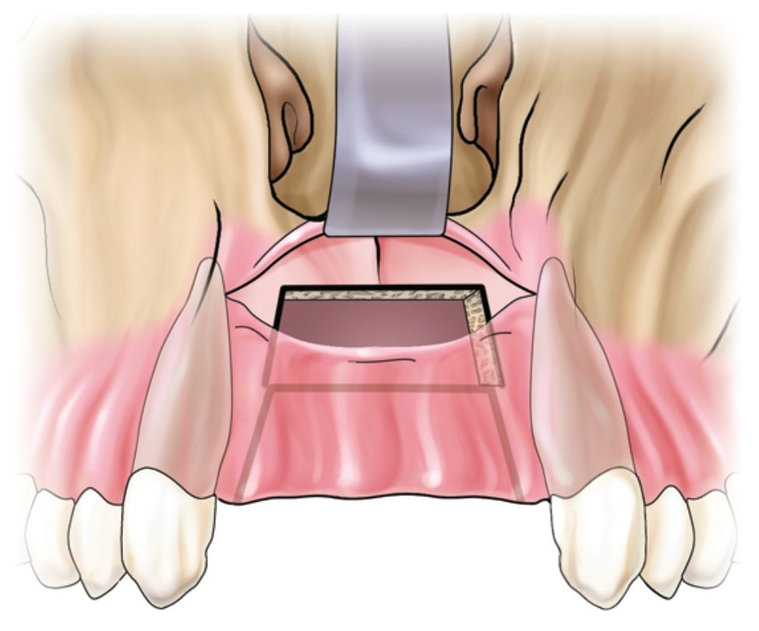
Onlay grafting in the anterior maxilla is approached by a crestal palatal incision made over the edentulous alveolar crest. The incision continues into the gingival sulcus of the teeth adjacent to the edentulous space. Vertical buccal releasing incisions are performed on each side at least 5 mm away from the area to be grafted. Full-thickness buccal and palatal flaps are required. The site is then recontoured for graft adaptation and perforated to induce revascularization.
Harvested bone is placed and fixed. The graft must be immobile for revascularization to occur. A healing period of 6 months or more is recommended before implant surgery. Any one of these steps, if not done correctly, can lead to graft failure. If healing is uneventful, the bone should be remodeled, vital, and able to adapt to functional load 7 months after onlay bone grafting.22
Self-tapping screw-shaped implants have also been used to fix block grafts.23,24 Although a one-stage surgery reduces the number of interventions, the potential for complications is magnified. Therefore, most authors recommend a two-stage approach25,26 because it takes longer than 1 year to achieve sufficient integration in graft bone when implants are placed simultaneously.26,27 With delayed placement, the graft is at least partly revascularized and regenerated at the time of implant surgery. The delayed approach also makes correct positioning of implants more likely.28
Complications, such as exposure of the onlay bone graft, are not uncommon.21 When this happens, it invariably leads to a loss of soft tissue. The treated site can become worse than the initial defect.
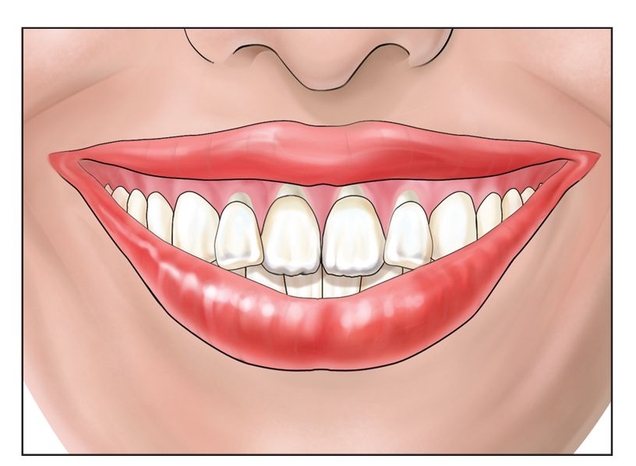
Fig 9-1a A high smile line is an indication for the use of the anterior maxillary sandwich osteotomy.





