Chapter 9
Reassessment
Time for decision making
Following completion of initial nonsurgical therapy, the importance of reviewing treatment responses and outcomes is well recognized, but its importance is often underestimated. Some of the most important decisions for the management of periodontal disease are typically required at this time in order to determine both future periodontal treatment needs and other important long-term goals, such as other restorative requirements.
The role of the reassessment appointment is to determine the response to the treatment that has been carried out, at both the tooth level and the patient level, and to decide on any further treatment that will be required. Reassessment is typically carried out at least 6 weeks after completion of initial treatment. Although it is known that healing events, and thus clinical improvements such as reducing pocket depths, may continue over a period of a few months, it is recognized that most of the healing will occur within approximately 6 weeks, and thus this period represents the shortest postoperative time suitable for carrying out the review of treatment response.
Reassessment (or review) is the comparison of clinical measurements before and after carrying out active treatment in order to measure treatment responses. Thus, the importance of accurate and thorough baseline assessment and diagnosis (discussed in < ?xml:namespace prefix = "mbp" />
Note that the Basic Periodontal Examination (BPE; and also the Community Periodontal Index) discussed in
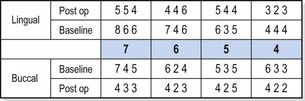
Fig 9.1 Six-point probing pocket chart of lower right sextant of a patient at baseline (prior to treatment) and at reassessment following completion of initial nonsurgical treatment. It is clear that there has been an excellent response to treatment overall. However, the BPE score for this sextant is “4” at baseline and remains “4” postoperatively because of the persisting 6-mm pocket at LR6 lingually. BPE does not provide any information about where there has been a good (or poor) response, and it completely fails to identify the generally excellent response to treatment in this sextant.
Assessing treatment outcomes
The primary objective of periodontal treatment is to eliminate existing disease and to prevent future disease progression. In clinical terms, this generally means the absence of bleeding at a site, together with a pocket that is sufficiently shallow as to be possible to maintain in the future. A site that bleeds and that continues to have a deep pocket is at increased risk of further disease progression in the future, whereas the absence of bleeding and deep pockets is a good predictor of future health of a site. In practical terms, a pocket depth of less than 5 mm is considered to be maintainable in the future by adequate oral hygiene measures alone (including an appropriate professional maintenance programme, discussed in
Therefore, at reassessment, any site may be judged to be as follows:
1. A “treated site”—one that is now less than 5 mm and not bleeding
2. A “responding” or “partially treated” site—one that shows improvement (pocket depth reduction) from baseline but that is still 5 mm or greater or still bleeds on probing
3. A “nonresponding site”—one that has shown no improvement from baseline or shows deterioration
It is common for there to be a mixture of all three of these outcomes in the same patient.
In addition, in assessing treatment outcomes, it is well described that different patients may show varying responses to treatment such that any particular patient may be judged to show a good overall response to treatment or a poor overall response to treatment.
To further complicate the matter, it is thus possible to see nonresponding sites in a patient who otherwise shows a generally good response to treatment or to see some sites that have responded well to treatment in a patient who otherwise shows a generally poor response to treatment.
Reasons for poor responses to treatment
Having diagnosed treatment responses at both the site level and the patient level, the next step in the reassessment process is to decide what further treatment is required, particularly for nonresponding sites. A logical approach to this process is first to decide the likely reasons for an inadequate treatment response, because this will help dictate the appropriate course of action for future management.
The main reasons for inadequate treatment responses are summarized in
Table 9.1 Diagnosing and managing inadequate treatment responses
| Cause | Comments | Further treatment options |
|---|---|---|
| Incorrect initial diagnosis | For example, disease too severe to be treatable; endodontic involvement or perio/endo lesion; other gingival pathology such as lichen planus; other periodontal pathology such as malignant disease causing bone loss | Implement appropriate treatment for condition |
| Inadequate plaque control | Poor compliance/motivation; inadequate dexterity; inability to access specific areas for OH; the presence of plaque-retentive factors such as calculus or overhanging restorations | Continue to reinforce OH procedures; correct any persisting local factors |
| Inadequate subgingival debridement | Difficult access for RSD—very deep sites, infrabony sites, posterior sites; the presence of difficult root anatomy such as grooves and furcations; inadequate RSD technique | Repeat RSD; periodontal surgery |
| Smoking | A major cause of poor patient treatment outcomes | Smoking cessation |
| Other | Less common causes—often difficult to diagnose except by exclusion of the above; systemic factors such as poorly controlled diabetes; possibly genetic factors; possibly associated with the presence of specific bacteria such as Aa | Adjunctive antimicrobial treatment; other adjunctive therapies (?) |
Incomplete subgingival debridement, particularly in localized areas, does not necessarily reflect on an operator’s technique. Root surface debridement (RSD) is carried out “blindly” and ultimately relies on tactile assessment to determine if all deposits have been removed successfully; thus, it is not surprising that this is not always successfully achieved (see
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


