Chapter 9
Problem Solving in Working Length Determination
Problem-solving issues and challenges in working length determination addressed in this chapter are:
“The healing processes after removal of a pulp occur in the tissue immediately adjacent to the point where the pulp was severed. It is, therefore, of great importance to retain the vitality of these tissues in order to make healing possible.”< ?xml:namespace prefix = "mbp" />
“If the tooth is uncomfortable, however, or presents an area of rarefaction, apical access must be obtained in order to negotiate the canal throughout its entire length to reach the periapical tissues.”
“Factors that may influence a difference [in the method used for working length determination] include the quality of radiographs, superimposed anatomic structures, or anomalous positions of root canal foramen.”
For many years, the tooth apex has been the focus of many anatomic and treatment studies.
Anatomic Basis for Challenges With Working Length Determination
The apex of the mammalian tooth is a complex biological unit composed of cementum, dentin, blood vessels, nerves, and connective tissues. One of the factors determining the long-term success of root canal treatment has been shown to be the relationship between instrumentation and obturation procedures and the anatomy of the apex.
Root formation and development are determined by the Hertwig’s epithelial root sheath (HERS), which maps out the external form of the root. The HERS is a double layer of epithelial cells derived from a proliferation of the internal and external dental epithelium (

FIGURE 9-1 Remnants of the Hertwig epithelial root sheath (HERS) (arrow) in the developing root structure. This is a layer of inner and outer enamel epithelium responsible for root formation as it invaginates into the alveolar bone.

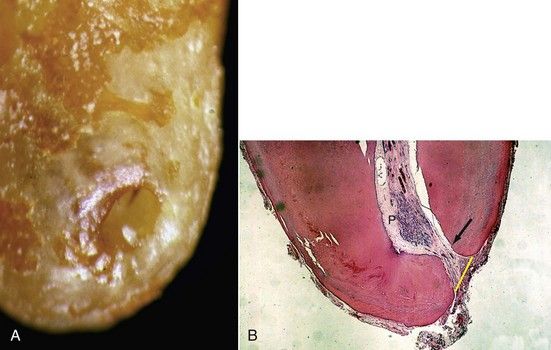
FIGURE 9-2 Palatal view of a mesial buccal root from a maxillary first molar, showing multiple foramina in the apical third of the root.
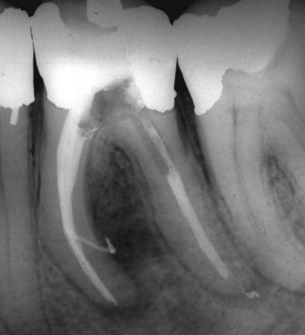
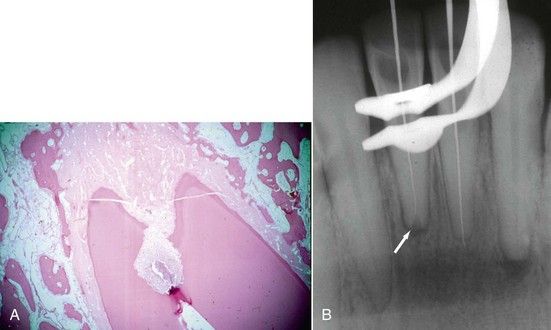
FIGURE 9-3 Large lateral canal leaving the mesial canals and exiting on the distal surface of the mesial root, as evidenced by filling during obturation. Note lateral lesion.
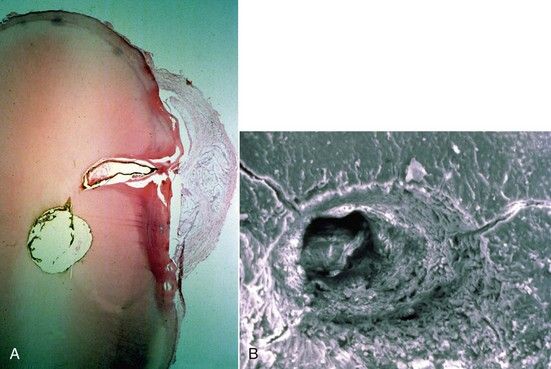
FIGURE 9-4 A, Histologic evidence of a large lateral canal in cross-section of the mandibular premolar. Note development of a cystic lesion on the lateral surface of the root. B, SEM (scanning electron microscopy) view of a lateral canal (×1800).
Extensive variability exists in the external apical root morphology of human permanent teeth with completed root apices (

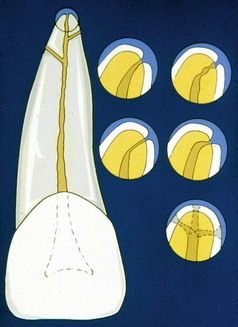
FIGURE 9-5 Multiple apical terminations pose clinical problems for working length determination, cleaning and shaping, disinfection, and obturation.

FIGURE 9-6 Overall view of an immature root that is forming shows a large dental papilla and advancing root sheath, left and right. Arrow indicates remnants of the epithelial sheath.
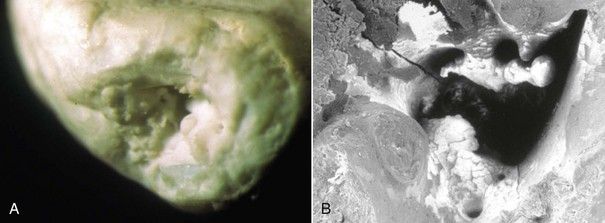
FIGURE 9-7 A, Resorbed root apex. B, SEM (scanning electron microscopy) of the same root apex shows significant irregularities. (×2000).

FIGURE 9-8 Radiograph showing apical resorption of the root apices of two teeth. Tooth on the left has an apical invaginating external resorptive defect that alters the position of the cemental-dentinal junction.
Internal morphology at the end of the root canal is determined by the odontoblasts responsible for development of the dentin. The transition from internal to external morphologic features occurs at the cementum-dentin junction (CDJ), delineated histologically by the odontoblasts. Coronal to this position, the tissue is classified as pulp tissue. However, the soft tissue contained within that portion of the canal apical to the CDJ is not dental pulp but a fibrous connective tissue that originates from the periodontal ligament and supplies the vessels and nerves leading to and from the pulp (

FIGURE 9-9 Root apex following root canal filling (RCF) short of the actual root length. Histologic evidence of hard-tissue formation (black arrows) that has formed from cells of the periodontal ligament (PDL) adjacent to root filling material. Note cementum formation (white arrows) on internal aspect of apical foramen.
The apical portion of the root canal system presents the greatest number of ramifications, with 27.4% of teeth demonstrating accessory and lateral canals or an extensive arborization, also known as an apical delta (
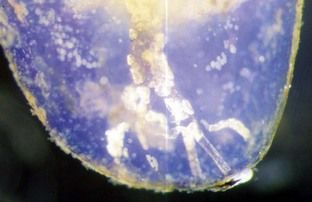
FIGURE 9-11 Apical delta formation in a demineralized and cleared tooth. Note presence of pulp stones in multiple small canals.
Studies have shown that the major foramina of most human teeth are distant from both the radiographic and anatomic apex
Apical Root Anatomy and Its Impact on Working Length
It is frequently impossible to know exactly where the apical foramen and apical constriction are located until after the canal has been obturated.
The seventh edition of the Glossary of Endodontic Terms defines the working length of a tooth as the distance from a coronal reference point to the point at which canal preparation and obturation should terminate.
The distance from the foramen to the constriction depends on a multitude of factors such as increased cemental deposition or radicular resorption (
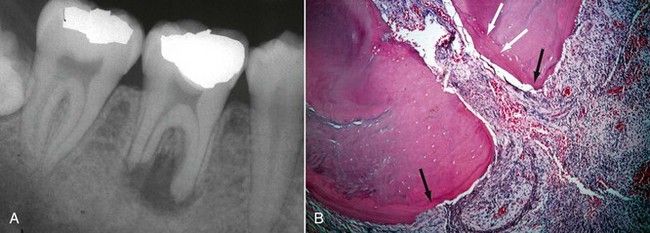
FIGURE 9-13 A, Mandibular molar with apical root resorption due to a necrotic, infected dental pulp that destroyed the natural cemental-dentinal junction. B, Histologic evidence of apical resorption on external cementum (black arrows) and layering of cementum (white arrows) into apical foramen (H&E stain ×10).
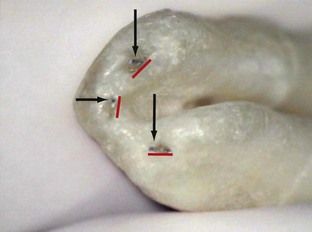
FIGURE 9-14 Apical view of tooth with a C-shaped root formation. Note root morphology around the canal exits as cementum invaginates into the foramen. K-files (arrows) are exiting from the canal long before they reach the actual root surface. Actual foramina are much larger than canal exits, as indicated by widths of the red lines. Working length determination to the root length in these cases would be destructive to periapical tissue.
Prior to establishing a definitive working length, coronal access to the pulp chamber must provide a straight-line avenue into the canal orifice, thereby facilitating subsequent canal penetration (see
Current concepts of initial canal penetration recommend preflaring techniques for a coronal-to-apical approach to working length determination rather than immediate penetration to the apex region.
In curved canals, however, after obtaining straight-line access, the working length can change, especially if debris is packed around the curvature and not removed on a regular basis. Techniques have been advocated for this purpose, and cognizant use of them is recommended.

FIGURE 9-15 When curves are present, as seen in the mesial buccal root, straight-line access is essential.
During access opening preparation, all caries, unsupported enamel, and faulty restorations are removed in an effort to secure stable reference points as aids in working length determination (see
Pathologic processes resulting in apical resorption can destroy the natural constriction of the CDJ (
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses