Oral Mucosa
Learning Objectives
New Key Terms
Capillary plexus (cap-ih-lary)
Hyperkeratinization (hi-per-ker-ah-tin-zay-shun)
Keratin (ker-ah-tin)
Keratohyaline granules (ker-ah-toe-hi-ah-lin)
Lamina propria (lam-i-nah pro-pree-ah)
Layer: basal (bay-sal), granular, intermediate, keratin (ker-ah-tin), prickle, superficial
Mucoperiosteum (mu-ko-per-ee-os-te-um)
Mucosa (mu-ko-sah): lining, masticatory (mass-ti-ka-tor-ee), specialized
Stratified squamous epithelium (strat-i-fide skway-mus ep-ee-thee-lee-um): nonkeratinized (non-ker-ah-tin-izd), orthokeratinized (or-tho-ker-ah-tin-izd), parakeratinized (pare-ah-ker-ah-tin-izd)
Stippling (sub-mu-ko-sah)
Submucosa (sub-mu-ko-sah)
Taste pore
Tongue: black hairy, geographic
Oral Mucosa
Dental professionals must have a clear understanding of the basic histology of the oral mucosa, the regional differences, and any clinical considerations that might be related to this information. Only then will they be able to understand the clinical considerations involved in injury to the oral mucosa, such as injury that occurs with trauma, inflammation, infection, and cancer, as well as with aging. With this information, they then can promote the health of the oral mucosa.
Classification of Oral Mucosa
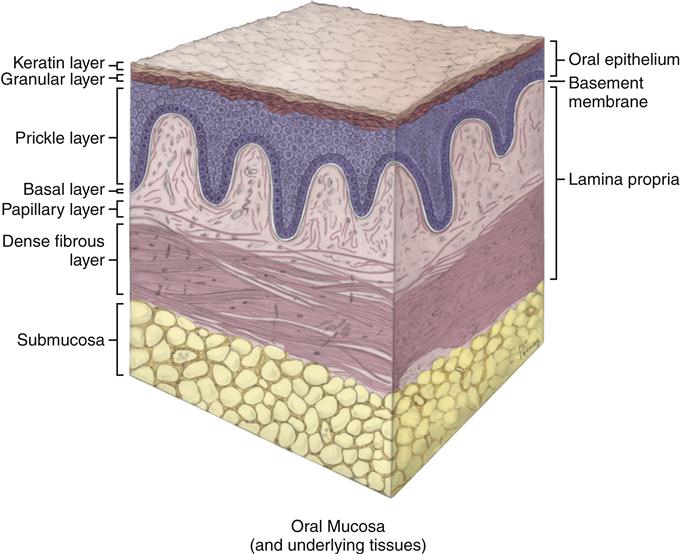
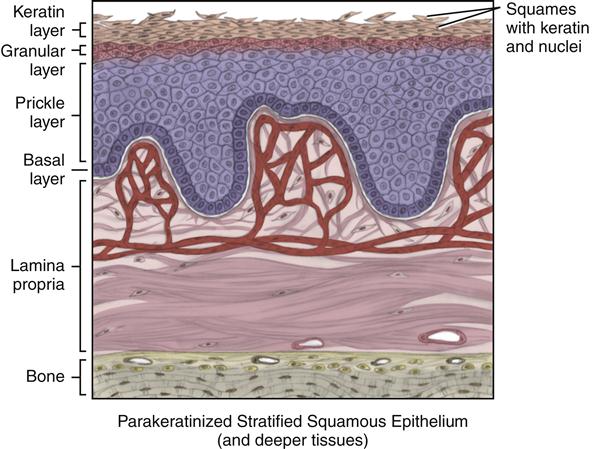
Oral mucosa almost continuously lines the oral cavity. Oral mucosa is composed of stratified squamous epithelium overlying a connective tissue proper, or lamina propria, with possibly a deeper submucosa (Figure 9-1; see Chapter 8).
Even though the entire oral cavity has an epithelial covering, and connective tissue makes up the bulk of lamina propria, regional differences are noted throughout the oral mucosa. For example, the oral mucosa is perforated in various regions by the ducts of salivary glands (see Figures 11-3 and 11-6). This chapter discusses later these regional differences, except the gingival sulcular region is discussed in more detail in Chapter 10.
A basement membrane lies between the epithelium and connective tissue in the oral mucosa (see Figures 7-6 and 8-4). It serves not as a separation between the two tissue types but as a continuous structure linking the two. Studies are focusing on trying to understand the interactions between these two tissue types, and the basement membrane may hold these answers.
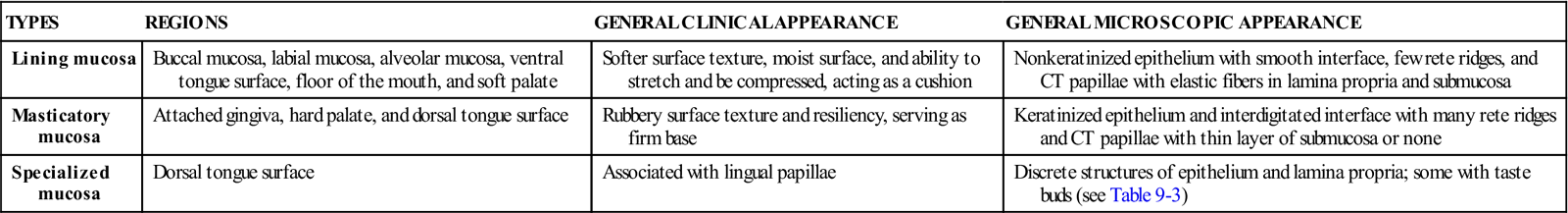
Three main types of oral mucosa are found in the oral cavity: lining, masticatory, and specialized mucosa (Table 9-1). This classification of mucosa is based on the general histological features of the tissue. The specific histological features of each oral region are discussed later. Overall, the clinical appearance of the tissue reflects the underlying histology, both in health and disease.
TABLE 9-1
| TYPES | REGIONS | GENERAL CLINICAL APPEARANCE | GENERAL MICROSCOPIC APPEARANCE |
| Lining mucosa | Buccal mucosa, labial mucosa, alveolar mucosa, ventral tongue surface, floor of the mouth, and soft palate | Softer surface texture, moist surface, and ability to stretch and be compressed, acting as a cushion | Nonkeratinized epithelium with smooth interface, few rete ridges, and CT papillae with elastic fibers in lamina propria and submucosa |
| Masticatory mucosa | Attached gingiva, hard palate, and dorsal tongue surface | Rubbery surface texture and resiliency, serving as firm base | Keratinized epithelium and interdigitated interface with many rete ridges and CT papillae with thin layer of submucosa or none |
| Specialized mucosa | Dorsal tongue surface | Associated with lingual papillae | Discrete structures of epithelium and lamina propria; some with taste buds (see Table 9-3) |
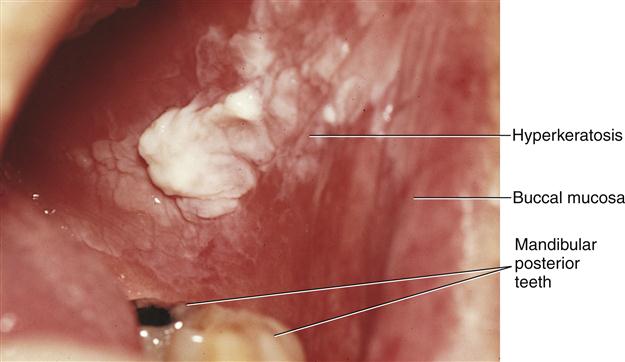
In addition, the oral cavity has sometimes been described as a mirror that reflects the health of the individual. Changes indicative of disease are seen as alterations in the oral mucosa lining the mouth, which can reveal systemic conditions, such as diabetes or vitamin deficiency, or the local effects of chronic tobacco or alcohol use.
Lining Mucosa
Lining mucosa is a type of mucosa noted for its softer surface texture, moist surface, and ability to stretch and be compressed, acting as a cushion for the underlying structures. Lining mucosa includes the buccal mucosa, labial mucosa, alveolar mucosa, as well as the mucosa lining the ventral surface of the tongue, floor of the mouth, and soft palate.
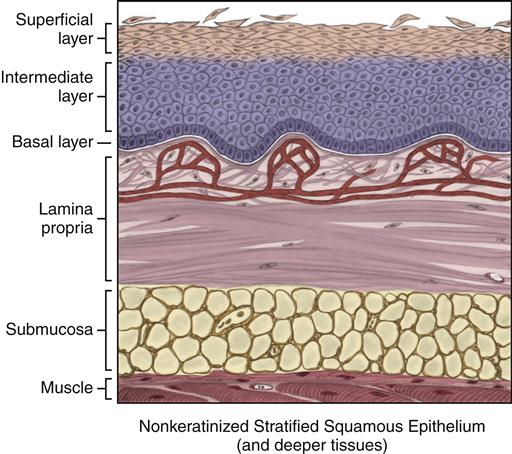
Histologically, lining mucosa is a type that is associated with nonkeratinized stratified squamous epithelium (Figure 9-2). In contrast to masticatory mucosa (discussed next), the interface between the epithelium and the lamina propria is generally smoother, with fewer and less-pronounced rete ridges and connective tissue papillae. In addition to these factors, the presence of elastic fibers in the lamina propria also provides the tissue with a movable base.
A submucosa deep to the lamina propria is usually present, overlying muscle and allowing compression of the superficial tissue. These general histological features allow this type of mucosa to serve in regions of the oral cavity where a movable base is needed, as during speech, mastication, and swallowing. Surgical incisions in this tissue frequently require sutures for closure. Local anesthetic injections into these areas are easier to accomplish than in masticatory mucosa, with less discomfort and easy dispersion of the agent, but infections also spread rapidly.
Masticatory Mucosa
Masticatory mucosa is noted for its rubbery surface texture and resiliency. Masticatory mucosa includes the hard palate, attached gingiva, and dorsal surface of the tongue.
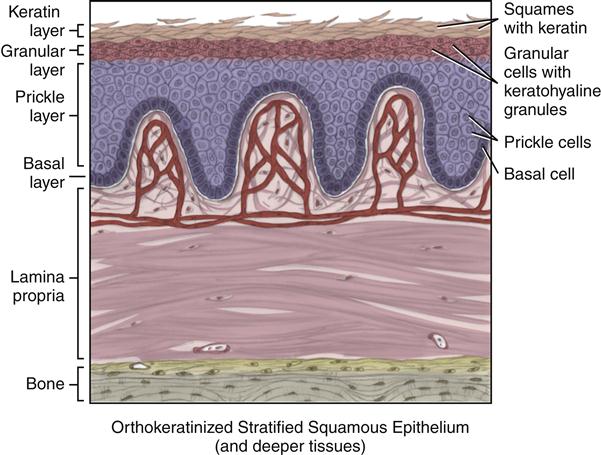
Histologically, masticatory mucosa is associated with orthokeratinized stratified squamous epithelium, as well as parakeratinized stratified squamous epithelium (Figures 9-3 to 9-5). Unlike lining mucosa discussed earlier, the interface between the epithelium and lamina propria in masticatory mucosa is highly interdigitated with numerous and more-pronounced rete ridges and connective tissue papillae, giving it a firm base. In addition, the submucosa is an extremely thin layer or is absent. When masticatory mucosa overlies bone, with or without submucosa, it increases the firmness of the tissue.
These general histological features allow this type of mucosa to function in the regions that need a firm base during mastication and speech. Sutures are rarely needed for this tissue after surgery. However, local anesthetic injections are more difficult and cause greater discomfort than those in lining mucosa, as well as when any swelling from an infectious source occurs.
Specialized Mucosa
Specialized mucosa is found on the dorsal surface of the tongue, as well as the lateral surface of the tongue, in the form of the lingual papillae (discussed later). Lingual papillae are discrete structures composed of keratinized epithelium and lamina propria (see Figure 2-14).
Epithelium of Oral Mucosa
Three types of stratified squamous epithelium are found within the oral cavity: nonkeratinized, orthokeratinized, and parakeratinized (Table 9-2). Nonkeratinized epithelium is associated with lining mucosa. Orthokeratinized and parakeratinized epithelium are both associated with masticatory mucosa. All forms of epithelium act as a barrier to pathogenic invasion and mechanical irritation and offer protection against dryness. These protective features are accentuated in epithelium with keratin.
TABLE 9-2
| TYPES OF EPITHELIUM | ASSOCIATED TYPE OF MUCOSA | BASIC HISTOLOGICAL DESCRIPTION |
| Nonkeratinized epithelium | Lining mucosa | Basal, intermediate, superficial layers |
| Orthokeratinized epithelium | Masticatory mucosa | Basal, prickle, granular, keratin layers (cells contain only keratin and no nuclei) |
| Parakeratinized epithelium | Masticatory mucosa | Basal, prickle, granular, keratin layers (cells contain keratin and nuclei) |
Histologists use the term keratinocytes for the epithelial cells in oral mucosa because they can produce keratin either naturally at normal levels if it is a keratinized tissue, or at higher levels when the tissue becomes traumatized, even in previously nonkeratinized tissue. Nonkeratinocytes, those cells that do not produce keratin, may be present in much smaller numbers in the epithelium (Table 9-3). These include melanocytes, discussed later with melanin pigmentation, as well as Langerhans and Granstein cells, both of which arise from the bone marrow and help the skin’s immune responses by acting as antigenic markers. White blood cells (WBCs) are also present, with the polymorphonuclear leukocyte (PMN) being the most commonly occurring WBC in all forms of oral mucosa (see Figure 8-17).
TABLE 9-3
| TYPES | FEATURES | FUNCTIONS |
| Epithelial cell | Rapidly renewing cell that undergoes pathway of differentiation with desmosomes; can be derived from all three embryonic cell layers | Forms cohesive sheet that resists physical forces and serves as barrier to infection |
| Melanocyte | Dendritic cell of neural crest origin, forms a continuous network near basement membrane | Synthesis of melanin pigmentation with transfer to adjacent cells by injection (melanosomes) |
| Langerhans cell | Dendritic bone marrow–derived cell noted near basement membrane | Immune response with T-cell lymphocytes |
| Granstein cell | Similar to Langerhans cell | Same as Langerhans cell |
| Merkel cell | Neural cell noted near basement membrane | Sensory information |
Nonkeratinized Stratified Squamous Epithelium
Nonkeratinized stratified squamous epithelium is in the superficial layers of lining mucosa, such as in the labial mucosa, buccal mucosa, and alveolar mucosa, as well as in the mucosa lining the floor of the mouth, the ventral surface of the tongue, and the soft palate (see Figure 9-2). Lining mucosa has similar epithelial histological traits, even though it has its own regional differences. Nonkeratinized epithelium is the most common form of epithelium in the oral cavity.
Each lining mucosa has at least three layers within the epithelium. A basal layer, or stratum basale, is the deepest of the three layers. The basal layer is a single layer of cuboidal epithelial cells overlying the basement membrane, which, in turn, is situated superior to the lamina propria. The basal layer produces the basal lamina of the basement membrane.
The basal layer is also considered germinative because mitosis of the epithelial cells occurs within this layer; however, this cell division is seen only under higher magnification of the tissue (see Table 7-2). Future studies may show the existence of an epithelial stem cell in the basal layer that produces other stem and daughter cells, similar to the situation for blood cells in the bone marrow.
The layer of epithelium superficial to the basal layer in nonkeratinized epithelium is the intermediate layer, or stratum intermedium. The intermediate layer is composed of larger, stacked, polyhedral-shaped cells. These cells appear larger or plumper than the basal layer cells, because they have larger amounts cytoplasm. The cells of the intermediate layer have lost the ability to undergo mitosis as they migrated. The intermediate layer makes up the bulk of nonkeratinized epithelium.
The most superficial level in nonkeratinized epithelium is termed the superficial layer, or stratum superficiale. It is hard to discern the exact division between the superficial layer and the intermediate layers in lining mucosa when viewing histological sections. This layer shows even larger similarly stacked polyhedral epithelial cells with the outer cells flattening into squames. The squames in these layers show shedding or loss as they age and die during the turnover of the tissue. Thus, maturation within this tissue is seen only as an increase in the size of cells as they migrate superficially.
Orthokeratinized Stratified Squamous Epithelium
Orthokeratinized stratified squamous epithelium demonstrates a keratinization of the epithelial cells throughout its most superficial layers (see Figures 9-3 and 9-4). Orthokeratinized epithelium is the least common form of epithelium found in the oral cavity. It is associated with the masticatory mucosa of the hard palate and the attached gingiva. It is also associated with the specialized mucosa of the lingual papillae on the dorsal surface of the tongue. As this tissue matures, it forms keratin within its superficial cells, showing a visible and physiological difference in the cells as they migrate superficially.
Like nonkeratinized epithelium, orthokeratinized epithelium has a single basal layer, or stratum basale, undergoing mitosis. This layer also produces the basal lamina of the adjacent basement membrane. Unlike nonkeratinized epithelium, however, orthokeratinized epithelium has more layers superficial to the basal layer: four separate layers with somewhat distinct divisions.
Superficial to the basal layer is the prickle layer, or the stratum spinosum. This layer is named for an artifact that occurs when the epithelial cells of this layer are dried for prolonged microscopic study; the cells shrink as a result of cytoplasm loss but still maintain their cellular junctions of desmosomes (see Figure 7-5). Thus, a prickly or spiky look results when the individual dehydrated epithelial cells are shrinking but still joined at their outer edges. Once they migrate to this superior a level in the tissue, cells of the prickle layer lose the ability to undergo mitosis, such as noted in the deeper basal layer. The prickle layer makes up the bulk of orthokeratinized epithelium.
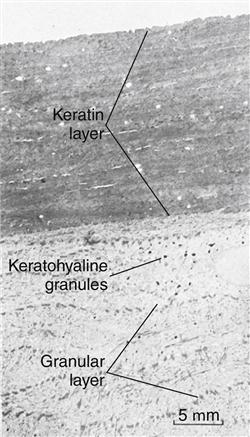
Superficial to the prickle layer is the granular layer, or stratum granulosum. The epithelial cells in this layer are flat and stacked in a layer three to five cells thick. In their cytoplasm, each of the cells has a nucleus with prominent keratohyaline granules, which stain as dark spots. The keratohyaline granules form a chemical precursor for the keratin that is found in the more superficial layers.
The most superficial layer in orthokeratinized epithelium is the keratin layer, or stratum corneum, which shows variable thickness depending on the region. The cells in the keratin layer are flat and have no nuclei, and their cytoplasm is filled with keratin. This soft, opaque, waterproof material is formed from a complex of keratohyaline granules and intermediate filaments from the cells and stains as a translucent dense material. The outer cells of the keratin layer, or squames, show increased flattening and also shedding or loss, because they are no longer viable.
In addition, parts of the keratin material are also shed as a result of the turnover of the tissue. However, these squames and their cornified cell envelope make up a major part of the epithelial barrier and are continuously being renewed. The epithelial barrier serves as protection from physical, chemical, and pathogenic attack, as well as dehydration and heat loss, that sometimes occur in the oral cavity environment.
Parakeratinized Stratified Squamous Epithelium
Parakeratinized stratified squamous epithelium is associated with the masticatory mucosa of the attached gingiva, in higher levels than with orthokeratinization, and also the tongue’s dorsal surface (see Figure 9-5). Most histologists believe that parakeratinized epithelium is an immature form of orthokeratinized epithelium. The presence of this form of keratinization on the skin is considered a disease state; therefore, parakeratinization is one of the unique histological features of the healthy oral cavity. Parakeratinized epithelium is also associated with the specialized mucosa of the lingual papillae on the dorsal surface of the tongue as well as the sulcular epithelium lining the sulcus.
Parakeratinized epithelium may have all the same layers of epithelium as orthokeratinized epithelium, such as the basal layer, prickle layer, granular layer, and keratin layer, although the granular layer may be indistinct or absent altogether.
The main difference between parakeratinized epithelium and orthokeratinized epithelium is in the cells of the keratin layer. In parakeratinized epithelium, the most superficial layer is still being shed or lost; however, these cells of the keratin layer contain not only keratin but also nuclei, unlike those of orthokeratinized epithelium. This distinction is sometimes difficult to discern under lower microscopic power in certain histological sections. Studies have shown that even though the epithelial cells have nuclei in the parakeratinized epithelium, they possibly are no longer viable, similar to the orthokeratinized epithelium.
Lamina Propria of Oral Mucosa
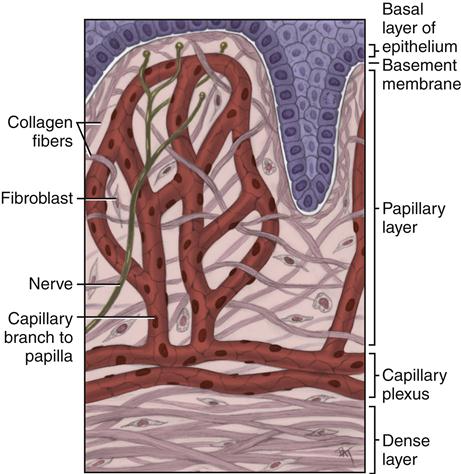
All forms of epithelium, whether associated with lining, masticatory, or specialized mucosa, have a lamina propria located deep to the basement membrane (see Figure 9-1). The main fiber group in the lamina propria is collagen fibers, but elastic fibers are present in certain regions of the oral cavity. The lamina propria, like all forms of connective tissue proper, has two layers: papillary and dense (Figure 9-7).
The papillary layer is the more superficial layer of the lamina propria. It consists of loose connective tissue within the connective tissue papillae, along with blood vessels and nerve tissue. The tissue has an equal amount of fibers, cells, and intercellular sub/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses