Dentin and Pulp
Learning Objectives
• Define and pronounce the key terms in this chapter.
• Discuss the dentin-pulp complex and describe the properties of dentin and pulp.
• Describe the processes of the apposition and the maturation of dentin.
• Outline the types of dentin.
• Label the anatomical components of pulp.
• Indicate and discuss the microscopic features of dentin and pulp.
• Describe the aging of dentin and pulp and discuss future concerns.
New Key Terms
Accessory canals (ay-pi-kl for-ay-men)
Apical foramen (ay-pi-kl for-ay-men)
Contour lines of Owen (serk-um-pul-pal), globular, interglobular, intertubular (in-ter-tube-u-lar), mantle, peritubular (pare-i-tube-u-lar), primary, secondary, tertiary
Dentin: circumpulpal (serk-um-pul-pal), globular, interglobular, intertubular (in-ter-tube-u-lar), mantle, peritubular (pare-i-tube-u-lar), primary, secondary, tertiary
Dentinal caries (den-tin-al), fluid, hypersensitivity (hi-per-sen-si-tiv-it-ee)
Imbrication (im-bri-kay-shun) lines of von Ebner (eeb-ner)
Pulp chamber, horns, stones (rah-dik-u-lar)
Pulp: coronal, radicular (rah-dik-u-lar)
Pulpitis (pul-pie-tis)
Tomes’ granular layer (tomes)
Dentin-Pulp Complex
Unlike enamel, both dentin and pulp cannot be viewed clinically if the teeth and associated periodontium are healthy. That is because both dentin and pulp make up the inner parts of the tooth and are not exposed to the oral environment except when certain dental pathology exists. In addition, because of their shared embryological background, close proximity, and interdependence, dentin and pulp form a dentin-pulp complex. Thus, this chapter discusses these two tissues together as one developmental and functioning unit.
Dental professionals must have a clear understanding of the histology of these two tissues. In the past, these two inner dental tissues were thought of as being analogous to a “black box” that was opened only during restorative procedures and thus hidden the rest of the time. With the advent of expanded responsibilities and increased preventive concerns for patients, all dental professionals must be able to know about these two interesting and challenging dental tissues.
Dentin
Mature dentin is a crystalline material that is less hard than enamel (see Table 6-2). Mature dentin is by weight 70% inorganic or mineralized material, 20% organic material, and 10% water. This crystalline formation of mature dentin consists of mainly calcium hydroxyapatite with the chemical formula of Ca10(PO4)6(OH)2. The calcium hydroxyapatite found in dentin is similar to that found in a higher percentage in enamel and in lower percentages in both cementum and bone tissue, such as alveolar bone. In addition, the crystals in dentin are platelike in shape and smaller in size than those in enamel.
Small amounts of other minerals, such as carbonate and fluoride, are also present. Dentin is covered by enamel in the crown and cementum in the root, as well as enclosing the innermost pulp tissue. Thus, dentin makes up the bulk of the tooth and protects the pulp.
Because of the translucency of overlying enamel, the dentin of the tooth gives the white enamel crown its underlying yellow hue, which is a deeper color in permanent teeth. If the outer coverings of either enamel or cementum are lost (discussed later), the exposed dentin on either the crown or root is various shades of yellow-white and appears rougher in surface texture than enamel. Yet, dentin is softer than enamel when instruments are used, allowing improper removal with hand instruments even in a healthy state, unlike enamel.
On a radiograph, the differences in the mineralization levels of different parts of the tooth can be noted. Dentin appears more radiolucent (or darker) than enamel because it is less dense, but is more radiopaque (or lighter) than pulp, which has the least density of the three dental tissues.
Apposition of Dentin Matrix
Dentinogenesis is the process of predentin formation that produces the initial dentin matrix during the stage of apposition of tooth development. The exact time of the stage of apposition varies according to the tooth that is undergoing development. Many factors can affect dentinogenesis when it is occurring (see Chapter 6).
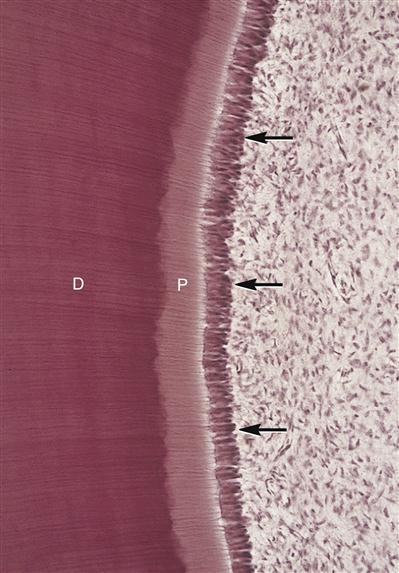
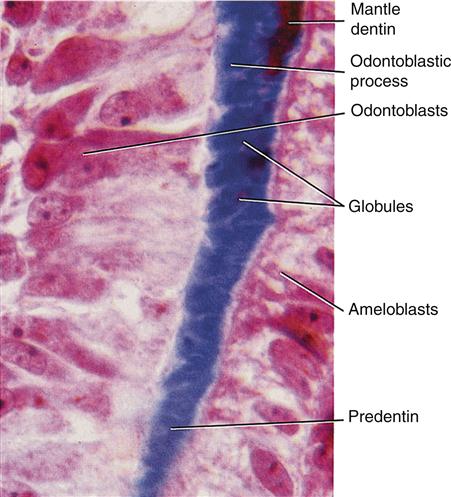
Predentin is the initial material laid down by the odontoblasts (Figure 13-2). It is a mesenchymal product consisting of nonmineralized collagen fibers. Odontoblasts were originally the outer cells of the dental papilla. Thus, dentin and pulp tissue have similar embryological backgrounds, because both are originally derived from the dental papilla of the tooth germ. These newly formed odontoblasts are induced by the equally newly formed ameloblasts to produce predentin in layers, moving away from the dentinoenamel junction (DEJ). Unlike cartilage and bone, as well as cementum, the odontoblast’s cell body does not become entrapped in the product; rather, one long, cytoplasmic attached extension remains behind in the formed dentin. Odontoblasts form approximately 4 μm of predentin daily during tooth development.
Apposition of dentin, unlike enamel, occurs throughout the life of the tooth (discussed later). Although ameloblasts are lost after the eruption of the tooth and enamel production ceases, production of dentin continues because of the retention of the odontoblasts within the tooth, along the outer pulpal wall.
Maturation of Dentin
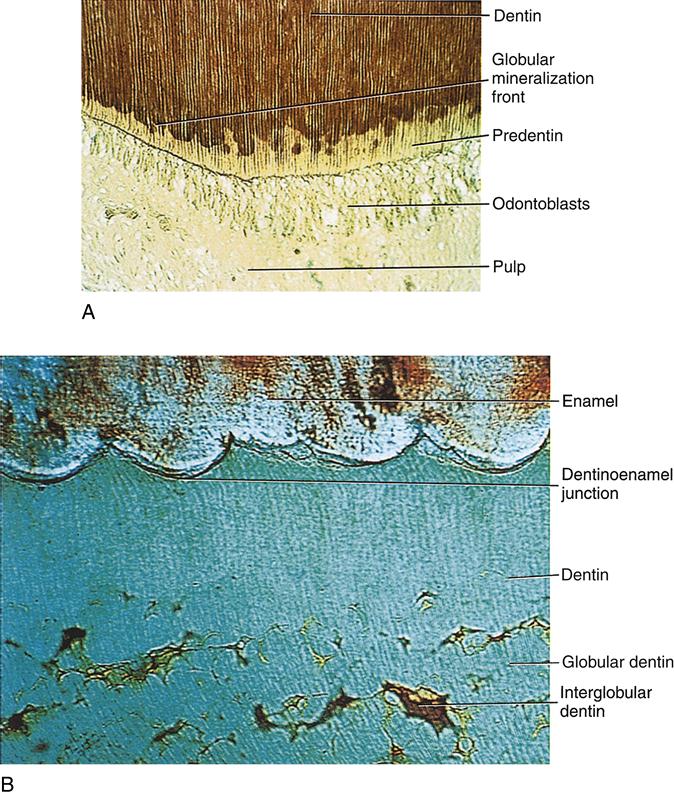
Maturation of dentin or mineralization of predentin occurs soon after its apposition. The process of dentin maturation takes place in two phases: primary and secondary (Figure 13-3). Initially, the calcium hydroxyapatite crystals form as globules, or calcospherules, in the collagen fibers of the predentin, which allows both the expansion and fusion during the primary mineralization phase. This process is analogous to the wash of watercolor paint placed on wet paper for a background, as the blobs of color run into each other—although, within dentin, it is a three-dimensional process.
Later, new areas of mineralization occur as globules form in the partially mineralized predentin during the secondary mineralization phase. These new areas of crystal formation are more or less regularly layered on the initial crystals, allowing them to expand, although they fuse incompletely. This process is analogous to additional blobs of paint placed in specific areas over a fuzzy painted background, but the colors of this additional layer do not run into each other to cover the page because the paper is no longer wet.
This incomplete fusion during the secondary mineralization phase results in differences noted in the microscopic features of the crystalline form of dentin. In areas where both primary and secondary mineralization have occurred with complete crystalline fusion, these appear as lighter rounded areas on a stained section of dentin and are considered globular dentin (Figure 13-4).
In contrast, the darker arclike areas in a stained section of dentin are considered interglobular dentin. In these areas, only primary mineralization has occurred within the predentin, and the globules of dentin do not fuse completely. Thus, interglobular dentin is slightly less mineralized than globular dentin. Interglobular dentin is especially evident in coronal dentin, near the DEJ, and in certain dental anomalies, such as in dentin dysplasia (see Figure 6-17).
Components of Mature Dentin
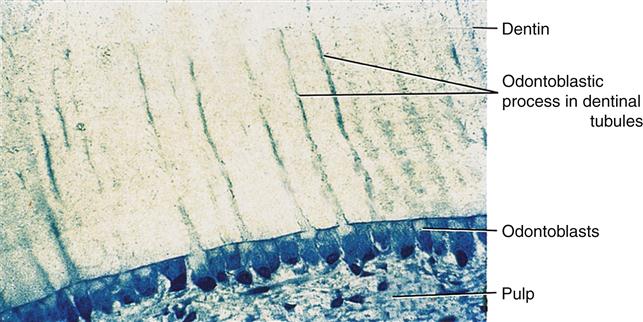
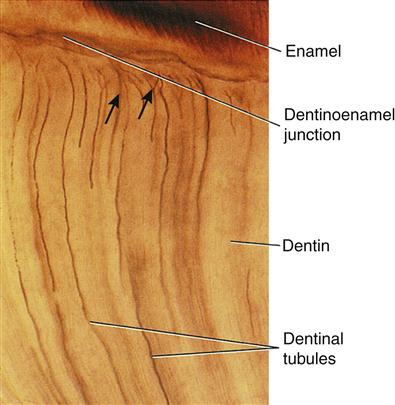
Within mature dentin, certain components, such as dentinal tubules and their contents, are noted (Figures 13-5 and 13-6). Dentinal tubules are long tubes in the dentin that extend from the DEJ in the crown area, or dentinocemental junction (DCJ) in the root area, to the outer wall of the pulp. After apposition of predentin and maturation into dentin, the cell bodies of the odontoblasts remain in the pulp inside the tooth, along its outer wall (discussed later).
Like enamel, dentin is avascular. Nutrition for odontoblasts within the dentin comes through the dentinal tubules from tissue fluid that originally traveled from the blood vessels located in the adjacent pulp tissue. Within each dentinal tubule is a space of variable size containing dentinal fluid, an odontoblastic process, and possibly an afferent axon.
The dentinal fluid in the tubule presumably also includes the tissue fluid surrounding the cell membrane of the odontoblast, which is continuous from the cell body in the pulp. The odontoblastic process is a long cellular extension located within the dentinal tubule that is still attached to the cell body of the odontoblast within the pulp. In a stained section of a tooth, odontoblastic processes within the dentinal tubule sometimes are not found at the periphery of dentin near the DEJ or DCJ. This absence may or may not be an artifact, given that live cell structures are difficult to preserve in dead mineralized tissues.
Studies suggest that the process occupies the full length of the tubule from the DEJ or DCJ to the pulp during only the early stages of odontogenesis. In mature dentin, however, the process may or may not run the full length of the dentinal tubule to extend near either the outlying DEJ or DCJ.
A sensory, or afferent axon, is associated with part of the odontoblastic process in some dentinal tubules. The myelinated axon may not extend farther than the process, and thus may not be located along either the DEJ or DCJ. Yet, the nerve cell body associated with the axon is located in the pulp along with the odontoblastic cell body. This axon is involved in registration of the sensation of pain only, and not any other sensations, even when triggered by other sensations (discussed later).
The direction of the tubule reflects the pathway of the odontoblast during apposition of predentin. There are two types of curvature established by the direction of the dentinal tubules: primary and secondary (Figure 13-7). The primary curvature of the dentinal tubules reflects the overall tubule course over time, which resembles a large S-shaped curve. The secondary curvature of the tubule consists of small, delicate curves noted in the primary curvature, reflecting the smaller daily changes in odontoblast direction during apposition. Dentinal tubules are not interrupted by the formation of the interglobular areas of dentin but pass right through them. Tubules can branch at any point along the way from the DEJ or DCJ to the pulp. Dentinal tubules are crowded n/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses