9
A New Clinical Protocol to Plan Craniomaxillofacial Surgery Using Computer – aided Simulation
Each year in the United States, a significant number of patients require craniomaxillofacial (CMF) surgery for the correction of congenital and acquired conditions of the head and face. The surgical correction of CMF deformities is complex and challenging. The success of these surgeries depends not only on the technical aspects of the operation, but also, to a larger extent, on the formulation of a precise surgical plan.1–10
Over the last 50 years, there have been significant improvements in the technical aspects of surgery, that is, rigid fixation, resorbable materials, distraction osteogenesis, minimally invasive approaches, and so on. However, the planning methods have mostly remained unchanged,3,4,6,10 and the question still remains: Are the traditional methods really appropriate for planning CMF surgery? Traditional planning methods will be critically reviewed and a new protocol for planning CMF surgery using computer – aided surgical simulation (CASS) will be presented.
CRITICAL REVIEW OF TRADITIONAL METHODS USED TO PLAN CRANIOMAXILLOFACIAL SURGERY
In CMF surgery, surgical planning involves a series of logical steps. These steps include data- gathering, diagnosis and quantification of the condition, establishment of a preliminary surgical plan, surgical simulation, establishment of the final surgical plan, and transfer of the plan to the patient.
Initially, data are gathered from a multitude of difference sources. These include the physical examination, medical photographs, plain radiographs (e.g., cephalogram and orthopantomogram), computed tomography (CT), and mounted plaster dental models.1,2 Each of these sources provides a portion of the whole dataset that is needed for successful planning. In practice, a surgeon evaluates each one of these studies in a sequential manner and creates a complete three- dimensional (3D) mental picture.
The next step in the planning process is the diagnosis and quantification of the deformity. In orthognathic surgery, an important part of this process is cephalometric analysis.1,11 After the surgeon has formulated the diagnosis, he or she develops a preliminary plan and, in many instances, alternative plans.
To test the feasibility of the preliminary plan(s), the surgeon then simulates the planned surgery. In orthognathic surgery, this is done by completing prediction tracings and dental model surgery.1,2 Prediction tracings are done by tracing the silhouette of the facial bones from a two- dimensional (2D) cephalogram onto a piece of acetate paper. These tracings are then cut and moved to evaluate possible outcomes. This task can also be completed in the computer.
Dental model surgery is then completed on plaster dental models that have been mounted on an articulator. This is undertaken by physically cutting the models and moving them to the desired position. In other types of surgery (e.g., trauma, pathology, and reconstruction), the extent of surgical simulation is even more limited. In clinical practice, most of these surgeries are not simulated. Sometimes, doctors obtain CT – based rapid prototyping physical models (e.g., stereolithography) to simulate skeletal surgery. After the simulation has been completed, a surgeon formulates the final surgical plan.
The last step in the planning process is to transfer the surgical plan to the patient at the time of surgery. In orthognathic surgery, the surgical plan is transferred to the patient prior to surgery by using surgical splints and selected measurements. The splints are fabricated on the same plaster dental models on which the surgery was simulated. In CMF surgeries that do not involve dentition, surgeons currently do not have a method of transferring the surgical plan to the patient. Although certain measurements taken during the planning process can be used to guide surgery, most of the time the process is more of an art than a science. There have been reports on the use of surgical navigation for this purpose,12-15 but this technique has not been universally adopted.
There are a number of problems associated with the traditional planning system. First, the coordinate systems of various datasources used for surgical planning are different. The physical examination and the medical photographs are taken with the patient’ s head oriented to the natural head position (NHP). The cephalogram is oriented to the Frankfort horizontal plane, and the articulated dental models are oriented to the axis-orbital plane.16 On average, these planes differ from each other by about 8 degrees.16 Currently, most surgeons are unaware of this problem and fail to account for the differences. This discrepancy alone can be responsible for a 15% difference in maxillary projection between the planned and the actual outcomes.16
In addition, using the traditional method, surgeons are not able to visualize the whole dataset in three dimensions.3-5,10,17,18 Instead, the surgeons have to create this picture in their minds. This creates a problem communicating with the other members of the treatment team. Clearly, it is impossible to assure that all involved have the same picture.
The analysis is 2D and only measures structures in a single plane. It may be appropriate for patients with symmetric deformities, but is inadequate for patients with asymmetric conditions.3,8 It has been reported that 34% of patients with dentofacial deformities have asymmetric conditions.19
Next, there may be inaccurate orientation of the dental models mounted on an articulator. The occlusal plane inclination of the dental models mounted on a semi- adjustable articulator is on an average 8 degrees steeper than the actual inclination of the occlusal plane.16,20 In addition, there are design flaws in the current devices used to orient the dental models on an articulator (i.e., the facebow). A patient can easily tilt the facebow during the registration process, creating an inaccurate recording of the occlusal cant (the roll of the maxilla). An inaccurate initial model position will always create an inaccurate plan.20
Dental model surgery is undertaken for two purposes. The first is to establish the occlusion, and the second is to reorient the models to ensure that the bones are placed in the ideal position at surgery. Because plaster dental models do not depict the surrounding bones, the surgeon is unable to visualize the effects of model position on the facial skeleton.5,6,21 Therefore, the ability to obtain the ideal bone position becomes a random event.4,6,7
Prediction tracings and the plaster model surgery are two separate processes, which are often inaccurate and time-consuming.3,22,23 Currently, an experienced surgeon spends 3–5 hours completing these steps, which is another drawback.24
In addition, the CT- based rapid prototyping models are costly (a single model costing, at the time of writing, about $2500), and they are unable to simulate different iterations of a given plan on a single model.17 Once the model has been cut, the cut cannot be undone. They also fail to render the teeth with the precision necessary for surgical planning.3,4,10
Finally, the fabrication of splints is time- consuming. A busy surgeon performs several of these operations per week, and many patients require two splints (intermediate and final). The fabrication of each splint may take an additional hour. 2,24 Moreover, for surgery that does not involve the dentition, surgeons do not have a way of transferring the surgical plan to the patient.3,6,8,13
CLINICAL SURGICAL PLANNING PROTOCOL
It is clear that many of the unwanted surgical outcomes are the result of deficient planning. The need to improve the traditional surgical planning methods has led our group to develop a 3D CASS system to plan CMF surgery. We have utilized this system in maxillofacial surgery,9,25-27 craniofacial surgery,28 trauma, and distraction osteogenesis.28-30 Using this system, doctors can perform “virtual surgery” and create a 3D prediction of the patient’ s surgical outcomes as if they were performing surgery in the operating room. We have documented the clinical feasibility,4,10 the accuracy,31 and the cost-effectiveness24 of this system. Our CASS system incorporates three distinctive features and innovations:
- Multiple imaging modalities are used to create an accurate model of the craniofacial skeleton.
- Special techniques are employed to orient the computerized bone model in the NHP.
- Computer-aided design (CAD)/computer-aided manufacturing techniques are used to fabricate accurate surgical splints and templates to transfer the surgical plan to the operating room. Our CASS planning protocol is presented as follows.
Step 1: Clinical e xamination and anthropometric measurements
A complete clinical examination and anthropometric measurements are essential for the clinical decision making process.1,32,33 They should be performed based on the patient’ s NHP. This information provides not only static, but also extremely valuable dynamic information (see Chapter 2 for details).
Step 2: Creation of a computerized composite skull model
A composite skull model is a computerized CT model that simultaneously displays an accurate rendition of both the bony structures and the teeth. Although 3D CT scans have been successfully used to visualize the patient’ s condition, they have not been successfully used for surgical simulation because the CT does not render the teeth with the accuracy that is necessary for surgical simulation.
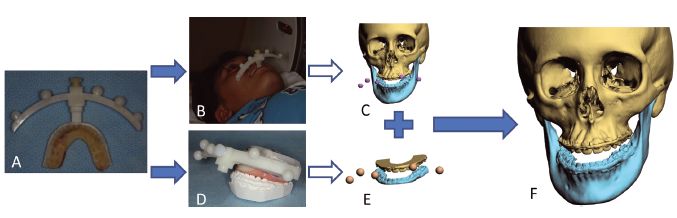
Figure 9.1 (A) Facebow with fiducial markers is attached to the bite-jig. (B) The patient bites on the bite-jig and facebow during a computed tomography scan. (C) Three separate but correlated computer models are reconstructed: a midface model, a mandibular model, and a fiducial marker model. (D) The bite-jig and facebow are placed between the upper and lower plaster dental models during the scanning process. (E) Three separate but correlated computer models are also reconstructed: an upper digital dental model, a lower digital dental model, and a fiducial marker model. (F) By aligning the fiducial markers, the digital dental models are incorporated into the 3D computed tomography skull model. The computerized composite skull model is thus created. It simultaneously displays an accurate rendition of both the bony structures and the teeth.
In order to replace the inaccurate dentition in the 3D CT model, a composite skull model is used in the surgical plan/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


