Implant-Related Complications and Failures
Stuart J. Froum, Perry R. Klokkevold, Sang Choon Cho and Scott H. Froum
Patients have experienced much success with endosseous dental implants.2,96 Yet, despite the long-term predictability and success of implants, complications do occur in a percentage of cases.3,27 Some complications are relatively minor and easy to correct, but others are more significant, resulting in loss of implants, failure of prostheses, and occasionally in severe loss of tissues in the area of implant failure. Complications may be surgical, biologic, mechanical, or esthetic.
Definition of Implant Survival and Implant Success
Implant success, conversely, is defined not only by the presence of the implant but also by criteria evaluating the condition and function of the implant at the time of examination. Criteria for implant success and failure have been defined over the years, but not all investigators use them. In the classic definition, Albrektsson et al6 defined implant success as an implant with no pain, no mobility, no radiolucent periimplant areas, and no more than 0.2 mm of bone loss annually following the first year of loading. Roos-Jansaker et al130 added to this definition by defining a successful implant as one that lost no more than 1 mm of bone during the first year in function. Sometimes these criteria are used as proposed, whereas at other times, they are used by investigators with modifications and new criteria. Consequently, it is inherently difficult to make comparisons between studies and often impossible to make absolute conclusions about any aspect of implant success or failure based on one or a few studies.
If one considers “success” using a strict definition as the outcome without any adverse effects or problems, then “implant success” should be defined as any implant-retained restoration in which (1) the original treatment plan is performed as intended without complications, (2) all implants that were placed remain stable and functioning without problems, (3) periimplant hard and soft tissues are healthy, and (4) both the patient and the treating clinician(s) are pleased with the results. When these strict criteria are used, implant success (i.e., absence of complications) is projected to be only about 61% after 5 years for implant-supported fixed partial dentures (FPDs) and 50% after 10 years for combined tooth/implant FPDs.94
An additional criteria of implant success that is often unreported but must be considered is the “esthetic” success or patient satisfaction with the outcome. There have been a number proposed methods to evaluate esthetic results. A restorative index was proposed by Jensen et al80 to appraise the esthetics of the final restoration. The index uses a scale from 1 to 10 with 1 being an extremely poor result and 10 being a superlative esthetic result. The index, based on both subjective and objective criteria, evaluates the size and shape of the implant restoration in comparison to the equivalent contralateral tooth, blending into the arch, as well as the presence of the papillae, gingival form, color, and other factors considered essential in determining an esthetic result. The pink esthetic score (PES) is an index proposed by Furhauser et al61 that considers seven soft-tissue parameters, including an evaluation of the color, contour, and texture of the surrounding soft tissues (papilla and facial mucosa). Each parameter is given a score of 0, 1, or 2, which allows the best score of 14 to determine the highest level of esthetics. Other indices were proposed for single-tooth implant restorations in the esthetic zone.21,102 The most recent, proposed by Belser et al,21 combines a modified PES index with a white esthetic score (WES) focusing on the visible part of the implant restoration scoring five parameters from general tooth form to hue, value, surface texture, and translucency. The maximum possible WES score is 10. These indices are aimed at quantifying the esthetic result, which could then present an objective method of judging “implant esthetic success.”
Types and Prevalence of Implant Complications
The prevalence of implant-related complications has been reported in several reviews. However, until recently, a systematic review of the incidence of biological and technical complications in studies of at least 5 years revealed that biological complications were considered in only 40% to 60% and technical complications in only 60% to 80% of the studies. One of the few conclusions of this review indicated that the incidence of technical complications related to implant components and suprastructures was higher in overdentures than in fixed restorations.22 In a systematic review of reports on the survival and complication rates of implant-supported FPDs, Pjetursson et al94 found that the most common technical complication was fracture of veneers (13.2% after 5 years), followed by loss of the screw access hole restoration (8.2% after 5 years), abutment/occlusal screw loosening (5.8% after 5 years), and abutment/occlusal screw fracture (1.5% after 5 years; 2.5% after 10 years). Fracture of implants occurred infrequently (0.4% after 5 years; 1.8% after 10 years). A retrospective evaluation of 4937 implants by Eckert et al48 found that implant fractures occur more frequently in partially edentulous restorations (1.5%) than in restorations of completely edentulous arches (0.2%), and all observed implant fractures occurred with commercially pure 3.75-mm diameter threaded implants.
In a literature review that included all types of implant-retained prostheses, Goodacre et al66 found that the most common technical complications were loosening of the overdenture retentive mechanism (33%), resin veneer fracture with FPDs (22%), overdentures needing to be relined (19%), and overdenture clip/attachment fracture (16%). Their review, with the inclusion of edentulous patients having overdentures, seemed to indicate a significantly higher percentage of complications than Pjetursson’s systematic review121 of patients with implant-supported FPDs. Goodacre et al65 found it impossible to calculate an overall prosthesis complication rate because most studies included in their review did not report on several of the complication categories.
The most common complication reported for single crowns was abutment or prosthesis screw loosening. Abutment screw loosening varied dramatically from one study to another, ranging from 2% to 45%.66 The highest rate of abutment screw loosening was associated with single crowns, followed by overdentures. The rate of prosthesis screw loosening was similar, ranging from 1% to 38% in various studies. A higher frequency was reported for single crowns in the posterior areas (premolar and molar) than in the anterior region.
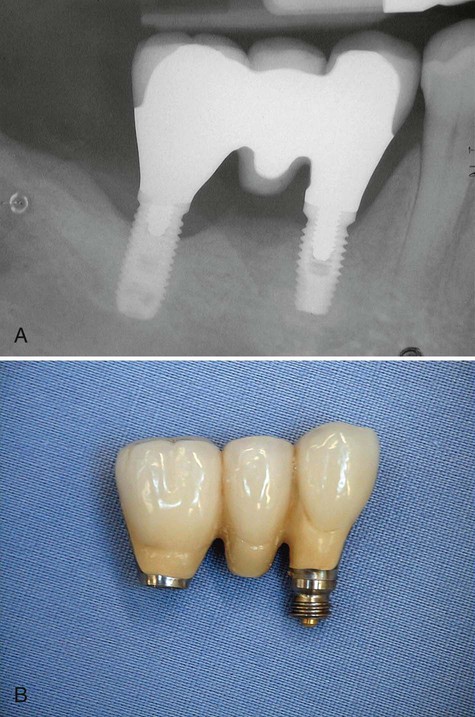
Implant fracture is an uncommon but significant complication. Goodacre et al65 reported a 1.5% incidence in their literature review. The incidence of implant fracture was higher in FPDs supported by only two implants. Consistent with this finding, Rangert et al125 reported that most fractured implants occurred in single- and double-implant–supported restorations. They also indicated that most of these fractures were in posterior partially edentulous segments, in which the generated occlusal forces can be greater, as opposed to anterior segments (Figure 82-1).
In a systematic review of prospective longitudinal studies (minimum of 5 years) reporting both biologic and technical complications associated with implant therapy (all restoration types included), Berglundh et al22 found that the incidence of technical complications was consistent with Pjetursson’s findings, with implant fracture occurring in less than 1% (0.08% to 0.74%) of cases. Interestingly, consistent with the findings in Goodacre’s review, technical complications were higher for implants used in overdenture therapy than implants supporting fixed prostheses.
In Pjetursson’s systematic review94 of survival and complication rates for implant-supported FPDs, biologic complications, such as periimplantitis and soft-tissue lesions, occurred in 8.6% of implant-supported FPDs after 5 years. However, in a more recent literature review of the prevalence of periimplant diseases, Zitzmann and Berglundh161 reported that although cross-sectional studies are rare, data from the only two studies available showed that periimplant mucositis occurred in 80% of the subjects and 50% of implant sites. Periimplantitis, conversely, was identified in 28% and 56% or more of subjects and in 12% and 43% of implant sites in the two studies that followed subjects with implants in function at least 5 years. A critical review of the literature by Esposito et al56 included 73 publications reporting early and late failures of Brånemark implants; biologically related implant failures were relatively low at 7.7%. The treatments involved all anatomic areas and all types of prosthetic design. The authors concluded that the predictability of implant treatment was especially good for partially edentulous patients compared with totally edentulous patients, with failures in the latter population being twice as high. Also, the incidence of implant failure was three times higher for the edentulous maxilla than for the edentulous mandible, whereas failure rates for the partially edentulous maxilla were similar to those for the partially edentulous mandible.
Risk factors, such as smoking, diabetes, and periodontal disease, may contribute to implant failure and complications. Several studies with numerous implants and years of follow-up have concluded that smoking is a definite risk factor for implant survival.12,44,45,50,111 A systematic review of the effect of risk factors on implant outcomes concluded that smoking has an adverse effect on implant survival and success, with the effects being more pronounced in areas of loose trabecular bone (i.e., posterior maxilla).90 The review suggested that type 2 diabetes may have an adverse effect on implant survival rates but did not have enough studies to permit a definitive conclusion.90 Finally, the same review also concluded that while patients with a history of treated periodontitis did not show any decrease in implant survival, they did experience more biologic implant complications and lower success rates.90
Different Types of Dental Implants
Many modifications have been developed to try to improve the long-term success rates of implants. More than 1300 types of dental implants are now available with different materials, shapes, sizes, lengths, and surface characteristics or coatings. There is limited evidence to show that implants with relatively smooth surfaces (i.e., machined) are less prone to bone loss from chronic infection (periimplantitis) than implants with rougher surfaces. Conversely, implants with a turned (smoother) surface might be at greater risk to fail early than implants with roughened surfaces since the bone-to-implant contact is comparatively less. To date, there is no evidence showing that any particular type of dental implant has superior long-term success.53
Different implant designs and surfaces must be studied in prospective human trials over long periods of time. At present, this data is not available, and the clinician should be aware that the data we currently have, even on rates of implant failure, may not reflect the outcome for implants being used today. Moreover, new implant surfaces and designs are continually being introduced with even less data available on potential complications.*
Surgical Complications
Hemorrhage and Hematoma
Postoperative bleeding is an equally important problem to manage (Figure 82-2). Patients should be given postoperative instructions on normal expectations for bleeding and how to prevent and manage minor bleeding. Historically, standard practice has recommended that they should be advised, with their physician’s approval, to discontinue or reduce medications that increase bleeding tendency 7 to 10 days before surgery. However, recent evidence suggests that this may not be necessary and may increase the risk of hematologic or cardiovascular problems81,82,111,132 (see Chapter 37). Dental healthcare providers should consult with medical healthcare providers regarding the best management for each individual patient. Furthermore, dental healthcare providers and patients should always include the treating medical practitioner in the management decisions if postoperative bleeding is excessive or persistent. Submucosal or subdermal hemorrhage into the connective tissues and soft-tissue spaces can result in hematoma formation. Postoperative bruising is a typical example of minor submucosal or subdermal bleeding into the connective tissues (Figure 82-3). Bruising and small hematomas typically resolve without special treatment or consequence. However, larger hematomas or those that occur in medically compromised individuals are susceptible to infection as a result of the noncirculating blood that sits in the space. Thus it is prudent to prescribe antibiotics for patients who develop a noticeably large hematoma.


Although the incidence of a life-threatening hemorrhage from implant surgery is extremely low, the seriousness of the problem warrants the attention of everyone who participates in this type of surgery. Potentially fatal complications have been reported for implant surgical procedures in the mandible (especially the anterior region).* Massive internal bleeding in the highly vascular region of the floor of the mouth can result from instrumentation or implants that perforate the lingual cortical plate and sever or injure the arteries running along the lingual surface. Depending on the severity and location of the injury, bleeding may be apparent immediately or only after some delay. In either case, the progressively increasing hematoma dissects and expands to displace the tongue and soft tissues of the floor of the mouth, ultimately leading to upper airway obstruction. Emergency treatment includes airway management (primary importance) and surgical intervention to isolate and stop the bleeding. Clinicians must be aware of this risk and must be prepared to act quickly. It is important to recognize that bleeding, although considered a complication at the time of surgery, may be a serious complication in the hours and days after surgery.41
Neurosensory Disturbances
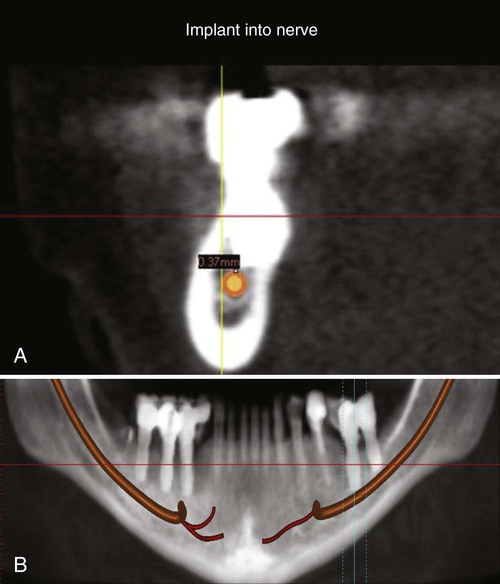
One of the more problematic surgical complications is an injury to nerves. Neurosensory alterations caused by damage to a nerve may be temporary or permanent. Neuropathy can be caused by a drilling injury (cut, tear, or puncture of the nerve) or by implant compression or damage to the nerve (Figure 82-4; also see Figure 73-18). In either case, the injury produces neuroma formation, and two patterns of clinical neuropathy may follow. Hypoesthesia is a neuropathy defined by impaired sensory function that is sometimes associated with phantom pain. Hyperesthesia is a neuropathy defined by the presence of pain phenomena with minimal or no sensory impairment.68 Some neuropathies will resolve, whereas other will persist. The type of neuropathy is not indicative of the potential for recovery.
Neurosensory disturbances reported in the literature are most prevalent and significant when they are more serious and occur more frequently, such as those associated with lateral transposition of the mandibular nerve.79,86 This relatively uncommon procedure is used to reposition the nerve and allow longer implants to be placed in the atrophic posterior mandible. Lateral nerve transposition procedures are associated with almost 100% incidence of neurosensory dysfunction immediately after surgery. More than 50% of these neurosensory changes are permanent (ranging from 30% to 80%).86 Several articles have been written on the treatment of neurosensory disturbances.7,107,126
Implant Malposition
Many of the aforementioned complications that arise during implant surgery can be attributed to the dental implant being placed in an undesired or unintended position. Malpositioning of dental implants is usually the result of poor treatment planning before the implant surgery, lack of surgical skill by the implant surgeon, and/or poor communication between implant surgeon and restorative dentist. Optimal implant esthetics and the avoidance of positional complications can be achieved by placing the implant in a prosthetically driven manner.103,116 In other words, the implant should be placed with reference to the three dimensions dictated by the position of the final restoration and not by the availability of bone. The angulation is another important determinant (fourth dimension) of implant position that will affect outcome esthetics. The ideal implant position entails an accurate preparation, insertion, and placement of the implant into the alveolus in a proper three-dimensional geometry according to apicocoronal, mesiodistal, and buccolingual parameters, as well as implant angulation relative to the final prosthetic restoration and gingival margins.91,133 (see Chapter 75).
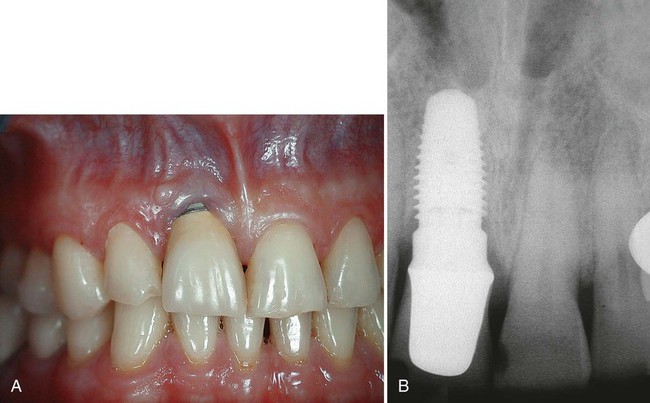
Apicocoronally, the implant should be placed so the dental implant platform is 2 to 3 mm apical to the gingival margin of the anticipated restoration.26 The actual implant position varies slightly from one implant system to another, depending on abutment design and space requirements. If the implant platform is placed too coronal, there will not be sufficient room to develop a natural-looking emergence profile and the tooth may have a squarish, unesthetic contour. If the platform is placed at or above the level of the gingival margin, a metal collar or implant exposure can occur yielding an unesthetic result (Figure 82-5). Conversely, if the implant platform is placed too apically, a long transmucosal abutment will be necessary to restore the implant. This can lead to a deep pocket and difficult hygiene access for the patient and clinician.

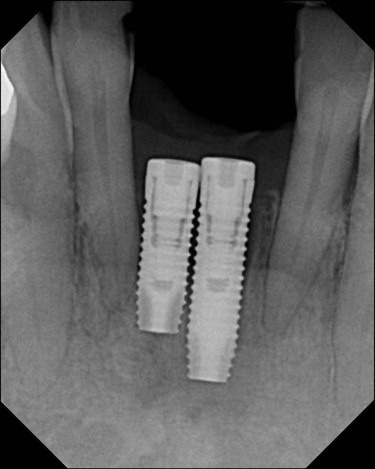
Mesiodistal implants should be placed at a distance of 1.5 to 2 mm from a natural tooth and 2 to 3 mm from an adjacent implant to maintain an adequate biologic dimension.70 Similar to natural teeth, violation of biologic width around an implant can lead to bone loss.75 Implants that are placed too close to each other (Figure 82-6) or natural teeth can be difficult to restore. Impression copings and impression-taking techniques must be modified. Improperly spaced implants invariably lead to chronic inflammation and peri-implantitis.51,153 Conversely, implants placed with excessive distance from an adjacent tooth or implant may require prosthetic compensation in the form of mesial or distal cantilevers, which may predispose the implant to biologic (e.g., bone loss) and mechanical (e.g., screw loosening,66 screw fracture,150 or implant fracture125) complications, as well as difficulties with hygiene.153
Ideally, implants should be placed, buccolingually so there is at least 2 mm of bone circumferentially around the implant.144 Implant exposure through the lingual or buccal cortex can predispose an individual to abscess and/or suppuration.35 Implants that are placed too far palatally/lingually require prosthetic compensation in the form of a buccal ridge lap, which may be difficult for the patient to clean and could lead to tissue inflammation.20
To obtain ideal esthetics, to avoid potential esthetic complications, and to correct bodily placement of the dental implant, the implant must be correctly angulated on insertion. In most anterior cases, it is desirable to have the implant long axis directed so it is emerging toward the cingulum. In the posterior region, the implant axis should be directed toward the central fossa or the stamp cusp of the opposing tooth. Implants that are placed with mild-to-moderate misangulations can often be corrected prosthetically with implant abutments. Minor misangulations (up to 15 or 20 degrees) can be corrected by with prefabricated stock-angled abutments; moderate misangulations (20 to 35 degrees) can usually be managed with customized UCLA-type abutments; extreme errors in implant angulations (more than 35 degrees) may deem an implant unrestorable and require it to be left submerged (i.e., sleeper) or to be removed (Figure 82-7).

The ultimate complication of malposed implant(s) is implant or instrument invasion into vital structures. The most common violation of neighboring anatomy is the placement of the dental implant into the adjacent tooth root. Surgical procedures used to prepare osteotomy sites and place implants adjacent to teeth can injure the teeth either by directly cutting into the tooth structure or by damaging nearby supporting tissues and nerves. Instrumentation (e.g., drills) directed at or near the adjacent tooth may cause injury to the periodontal ligament, tooth structure, and nerve of the tooth. Depending on the extent of the injury, the tooth may require endodontic therapy or extraction. On insertion, dental implants will follow the trajectory of the osteotomy prepared by the surgical drills. Care must be taken when preparing the osteotomy to stay true to the planned path of insertion. Guidepin location radiographs taken during implant surgery can greatly reduce the potential for damaging adjacent teeth (see Figure 73-15). Radiographic analysis before implant surgery should include detection of curved, convergent, and/or dilacerated root structures of adjacent teeth that can limit implant placement.
Particular care must be taken when placing implants in the mandible so as to not encroach on the inferior alveolar canal or the mental foramen (see Chapter 54) for a description of this anatomy. Encroachment on the mandibular canal or mental foramen during osteotomy or implant placement via direct contact or mechanical compression of bone can result in injury to nerves and blood vessels. Paresthesia, hypoesthesia, hyperesthesia, dysesthesia, or anesthesia of the lower lip, skin, mucosa, and teeth may result, as well as arterial or venous bleeding.67 The incidence of sensory disturbances after mandibular implant placement has been reported to range from 0% to 17.5%.16
The risks of surgery are always present, but the complications can be minimized with an understanding of the etiologies and with proper diagnosis and treatment planning. Three-dimensional imaging (e.g., computed tomography [CT] and cone-beam CT [CBCT] scans) provides the surgeon with useful presurgical information for proper diagnosis and treatment planning (see Chapter 73). Careful surgical exposure for direct visualization and identification of the mental nerve may be indicated as well. Once identified, it is recommended to establish a “zone of safety” and to keep instrumentation and implants a safe margin away from the nerve (e.g., ≥2 mm).67
Biologic Complications
Inflammation and Proliferation
Inflammation in the periimplant soft tissues has been found to be similar to the inflammatory response in gingival and other periodontal tissues. Not surprisingly, the clinical appearance is similar as well. Inflamed periimplant tissues demonstrate the same erythema, edema, and swelling seen around teeth. Occasionally, however, the reaction of periimplant soft tissues to bacterial accumulation is profound, almost unusual, with a dramatic inflammatory proliferation (Figure 82-8). This type of lesion is somewhat characteristic around implants and is indicative of either a loose-fitting implant to abutment connection or trapped excess cement that remains buried within the soft-tissue space or “pocket.” The precipitating local factor ultimately becomes infected with bacterial pathogens, leading to mucosal hypertrophy or proliferation and possible abscess formation (Figure 82-9). Correction of the precipitating factors (e.g., loose connection, retained cement) may effectively resolve the lesion. Another type of lesion resulting from a loose abutment connection is the fistula (Figure 82-10). Again, correcting the etiologic factor can quickly resolve the fistula.

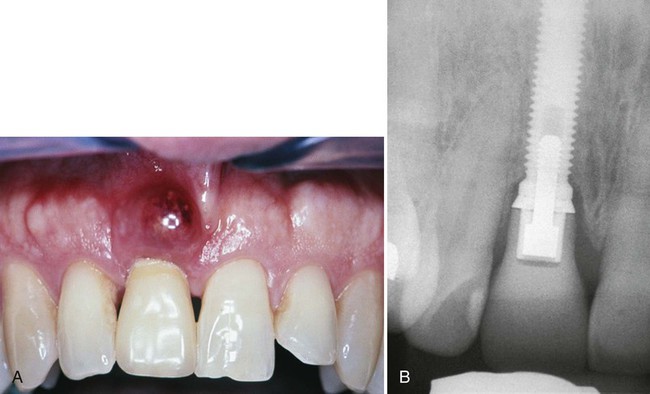
Dehiscence and Recession
Dehiscence or recession of the periimplant soft tissues occurs when support for those tissues is lacking or has been lost. Recession is a common finding after implant restoration and should be anticipated especially when soft tissues are thin and not well supported (Figure 82-11). Improper implant positioning also predisposes periimplant tissues to recession. As noted earlier, placement or angulation of the implant too far to the buccal causes the buccal plate to resorb and has been shown to result in greater recession.143 Another factor to consider is the thickness of the buccal plate of bone. Spray et al144 recommended this thickness to be 2 mm or greater to support the buccal soft tissue. If this thickness is not present, presurgical or simultaneous site development using guided bone regeneration is indicated. Recession is a problem that is particularly disconcerting in anterior esthetic areas. Patients with a high smile line or high esthetic demands consider such recession a failure (Figure 82-12).

Periimplantitis and Bone Loss
Periimplantitis is defined as an inflammatory process affecting the tissues around an osseointegrated implant in function, resulting in loss of supporting bone.108 The prevalence of periimplantitis has been reported to be controversial depending on the criteria used to define the amount of marginal bone loss necessary to be present, together with evidence of soft-tissue inflammation to determine the existence of the disease.89 Reports of prevalence of periimplantitis have varied from approximately 7% to 37% of implants in various studies.92,131 Recently, a proposed classification for early, moderate, and advanced periimplantitis based on degree of bone loss was presented in an attempt to improve communication when describing prevalence and treatment.60 To diagnose a compromised implant site, soft-tissue measurements using manual or automated probes have been suggested. Although some reports state that probing is contraindicated, careful monitoring of probing depth over time seems useful in detecting changes of the periimplant tissue.38,124,146,147
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



