7
Use of MTA as Root Perforation Repair
Mahmoud Torabinejad1 and Ron Lemon2
1 Department of Endodontics, Loma Linda University School of Dentistry, USA
2 UNLV, School of Dental Medicine, USA
INTRODUCTION
The decision of the clinician and patient with respect to the attempt to repair perforation by any cause requires the consideration of many factors. Iatrogenic perforation should be a rare event. If not, the clinician should review his/her case selection, technical skills, and availability of aids, such as the dental operating microscope (DOM), in order to reduce the incidence of perforation. Prevention is always preferable to repair and the clinician should select cases within his/her skill and experience level and refer challenging cases to an endodontist. Even successfully treated perforations may lower the long-term prognosis for the tooth due to loss of tooth structure and consequential increase in susceptibility to root fracture or periodontal breakdown.
The clinician must understand the important variables affecting the prognosis of perforation repair: time, location, and size of defect (Petersson et al. 1985; Fuss & Trope 1996). Many types of perforation can offer a good prognosis for repair if these variables are evaluated. Tooth loss is not inevitable after perforation and the clinician should offer treatment options to the patient prior to a recommendation for extraction. An “Endodontic Informed Consent” document must contain a statement concerning the possibility of perforation and the clinician should not be reluctant to discuss this outcome with the patient.
Important factors concerning the decision for repair or extraction of a perforated tooth include the interest of the patient to retain the tooth, the prognosis for repair, and the general condition of the patient’s mouth, restoratively and periodontally. Poor periodontal health related to inadequate oral hygiene compromises the prognosis for perforation repair. Additional treatment costs associated with perforation repair may not be advisable if the patient has extensive restorative needs.
Compared to historical treatment approaches, the prognosis for perforation repair has improved. A better understanding of the etiologic factors associated with successful outcomes and recent, biologically active materials, such as mineral trioxide aggregate (MTA; Dentsply Tulsa Dental, Tulsa, OK), have greatly improved repair prognosis. Prior to the era of biologically active materials, restorative materials were used in an attempt to seal the perforation defect. Amalgam, Cavit, Intermediate Restorative Material (IRM), glass ionomer, and composite were used with marginal results (Fig. 7.1). Wet conditions associated with perforation repair negatively affected the sealing properties of many of the materials (Seltzer et al. 1970; Alhadainy 1994; Fuss & Trope 1996; Regan et al. 2005; Tsesis & Fuss 2006). Controlling the placement of the materials was problematic and often the defect was not sealed adequately or the periodontal support tissues were chronically irritated from uncontrollable overfill of repair material (Fig. 7.2).
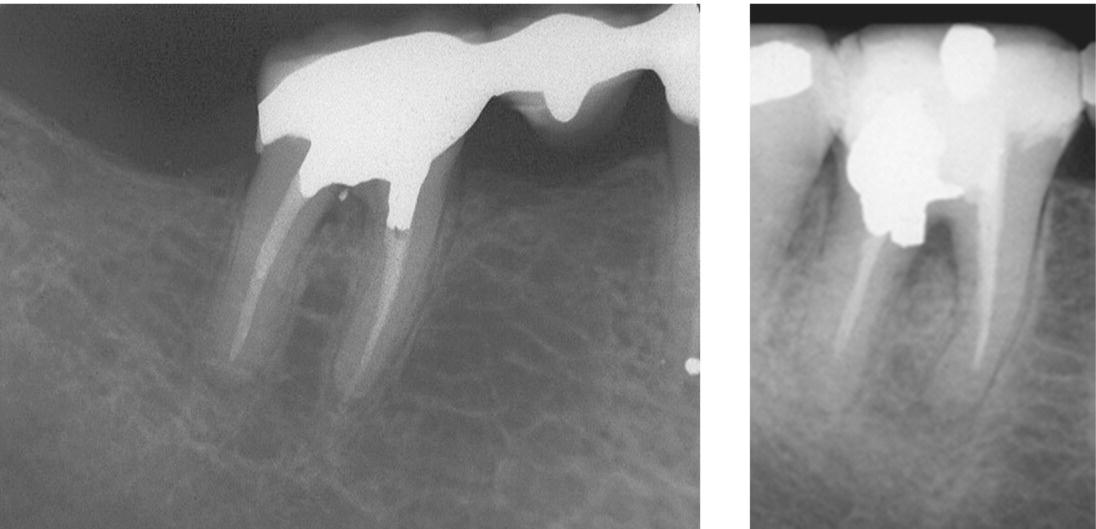
Fig. 7.1 Prior to the introduction of MTA, restorative material such as amalgam was used to seal perforation defects. Failure rate was high due to the presence of moisture and inability to control the placement of the materials. Both of these perforation repairs are failing due to periodontal breakdown.

Fig. 7.2 Controlling the placement of amalgam and its lack of seal in experiment has led to the development of a periodontal defect and formation of chronic inflammation in the furcation. In contrast the adjacent tooth repaired with MTA has not led into the same results.
To control moisture and to minimize extrusion of the repair material, an “internal matrix” method was developed. A biologically tolerant graft material, such as hydroxyapatite or calcium sulfate, was packed through the perforation to fill the osseous defect. Then, the repair material could be placed so that moisture contamination was reduced and placement of the repair material was more controllable, which reduced the incidence of extrusion of repair material (Lemon 1990, 1992).
When MTA was introduced into the market in 1998, the age of biologic repair began. The unique and desirable properties of MTA have been described earlier in this book. MTA has been shown to induce a biologic repair of the perforation defect. When MTA is hydrated in the presence of a balanced salt solution containing phosphate ions, hydroxyapatite crystals are formed on the surface of the MTA (Sarkar et al. 2005). Hydroxyapatite is essential for mineralization. A biologic repair implies that cementum or bone will cover the surface of the set MTA. Most importantly, chronic inflammation is minimal (Fig. 7.3) compared with other repair materials (Pitt Ford et al. 1995; Torabinejad et al. 1995; Koh et al. 1997; Keiser et al. 2000; Holland et al. 2001; Rafter et al. 2002; Camilleri & Pitt Ford 2006; Ribeiro et al. 2006; Souza et al. 2006; Camilleri 2008; Komabayashi & Spångberg 2008; Wang et al. 2009; Brito-Júnior et al. 2010; Samiee et al. 2010; Silva Neto et al. 2010; Fayazi et al. 2011). Pitt Ford et al. (1995) created furcation perforations in premolars of dogs and repaired them immediately or after a week of contamination with either amalgam or MTA. Their histological findings showed cementum formation underneath MTA in most treated specimens, in contrast to the samples whose furcation perforations had been repaired with amalgam. They also reported that when perforations are treated immediately and without contamination, the healing rate after their repair with MTA was significantly better than those contaminated with delayed repair. Yildirim et al. (2005) compared the healing of furcation perforations repaired with either MTA or Super EBA in dogs’ teeth. Their histological findings showed cementum formation underneath all MTA specimens at the 6-month interval. In contrast their Super EBA specimens showed no cementum formation and they had mild to severe inflammation at the same time interval. Noetzel et al. (2006), in another dog study, showed significantly more inflammation in furcation perforation sites repaired with tricalcium phosphate cement compared with those repaired with MTA after 12 weeks. Al-Daafas and Al-Nazhan (2007) compared gray MTA and amalgam as furcation perforation repair materials in dogs’ teeth that had been contaminated with bacteria. They also investigated the effect of calcium sulfate as a barrier beneath MTA. As in the previous investigation, the MTA samples showed significantly less inflammation and greater bone formation compared with their amalgam specimens. Their results showed when calcium sulfate was used to prevent MTA extrusion, it caused formation of mild to moderate chronic inflammation and stratified squamous epithelium around the repaired perforation sites. Vladimirov et al. (2007) repaired furcation perforations in dogs’ teeth with either ProRoot MTA or Titan cement. Their findings after 30 days showed presence of thinner capsules and fewer inflammatory cells in MTA specimens compared with those repaired with Titan cement. Based on available information, it appears that MTA produces better histological results compared with other currently used perforation repair materials. In addition, placement of a barrier beneath MTA has no significant effect on treatment success. Furthermore, repairing the perforation site immediately and avoiding bacterial contamination produces better results than their counterparts.
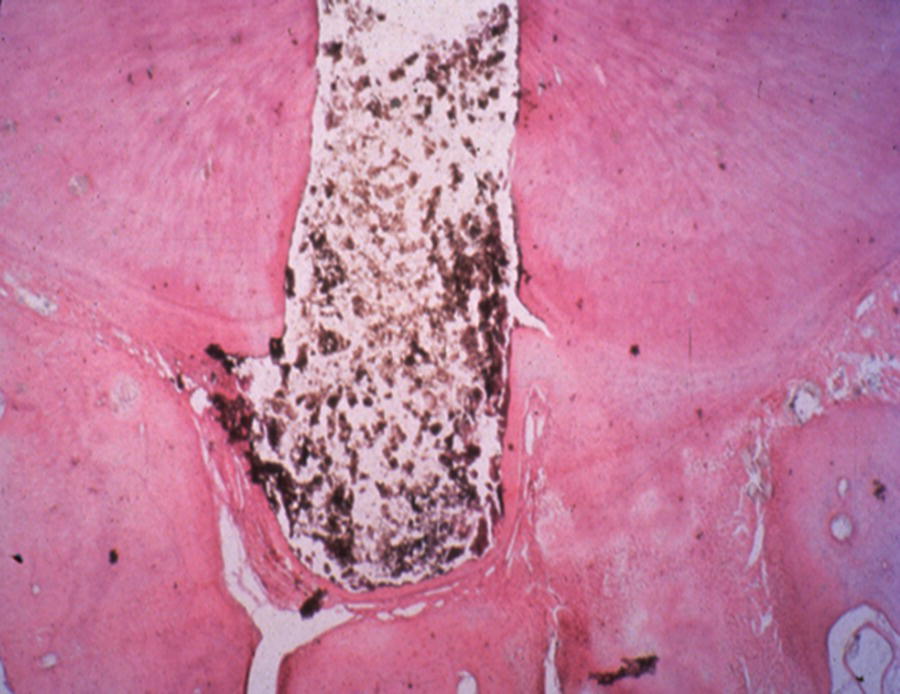
Fig. 7.3 Repair of a furcation perforation in a dog premolar with MTA results in formation of cementum adjacent to the repair material and lack of inflammation in the periodontal ligament.
The formation of hydroxyapatite crystals between the MTA and the tooth interface has been implicated in the excellent sealing properties reported for MTA (Koh et al. 1997; Holland et al. 1999; Regan et al. 2002; Main et al. 2004; Juárez Broon et al. 2006; Pace et al. 2008; Roberts et al. 2008; Miranda et al. 2009; Mente et al. 2010). The treatment outcome for many types of perforation defects has been greatly improved with the proper use of MTA.
TYPES OF PERFORATION DEFECTS
Access preparation-related perforations
Exploration for calcified canals can result in perforation. Perforation coronal to the crestal bone should be repaired with an appropriate restorative material, such as amalgam or composite (Fig. 7.4). Perforation below the crestal bone should be repaired with MTA. Every attempt should be made to avoid access-related perforations. Even with successful repair, the tooth is weakened and more susceptible to fracture. Preventive measures include:
- Careful evaluation of the preoperative radiograph. Calcification of the coronal chamber, angulation of the long axis of the root(s), and anatomy of the tooth should be considered. Horizontal radiographic angulation (mesial, distal) provides additional information to guide access preparation.
- Proper outline form for each type of access preparation. An improper design will result in inadequate vision and orientation during the access opening (Fig. 7.5).
- Magnification and lighting. Adequate vision allows the operator to see the subtle changes in the color and consistency of dentin that can offer clues to orifice location. If the coronal restoration is defective and will be replaced, vision is greatly enhanced if the restoration is removed before starting the access preparation. A microscope should be used for challenging cases, such as calcified canals or endodontic therapy through crowns.
- Radiographs taken during preparation. Metal clamps may prevent visualization of the access opening. Placement of the clamp on a distal or proximal tooth and placement of a “split dam” may prevent this problem. In some cases, location of the canal or chamber prior to placement of the rubber dam is recommended. The preoperative radiograph should be measured to determine the depth of preparation required to locate the chamber or canal. If this depth is approached and the chamber or canal is not located, a radiograph should be taken to evaluate orientation of the preparation (Fig. 7.6).


Fig. 7.4 (A) An accidental procedure has resulted in coronal perforation and development of a lesion on the distal of second mandibular premolar. (B) After finding the canal and its cleaning, as well as its obturation, the defect was repaired with amalgam.

Fig. 7.5 An improper design has resulted in inadequate vision and orientation and lateral crown perforation during access preparation.

Fig. 7.6 Placement of a small bur at the bottom of the access preparation and taking a radiograph is extremely helpful to locate calcified canals.
Cleaning and shaping related (“strip”) perforations
Most perforations of this type can be avoided by utilization of proper endodontic technique. Knowledge of root anatomy for each type of tooth and study of the preoperative and working length radiographs for canal curvatures are essential in the prevention of perforation (Fig. 7.7). Perforation repair with MTA is more difficult in the coronal area of the root compared to the apical portion of the canal. Using cleaning and shaping instruments too large for a given canal and failure to recognize the proximity of canals to the furcation in multi-rooted teeth are the most frequent causes of this type of perforation (Fig. 7.8).


Fig. 7.7 Lack of attention to the anatomy of mesial roots (A) has resulted in severe strip perforation (B) in the mandibular molar.
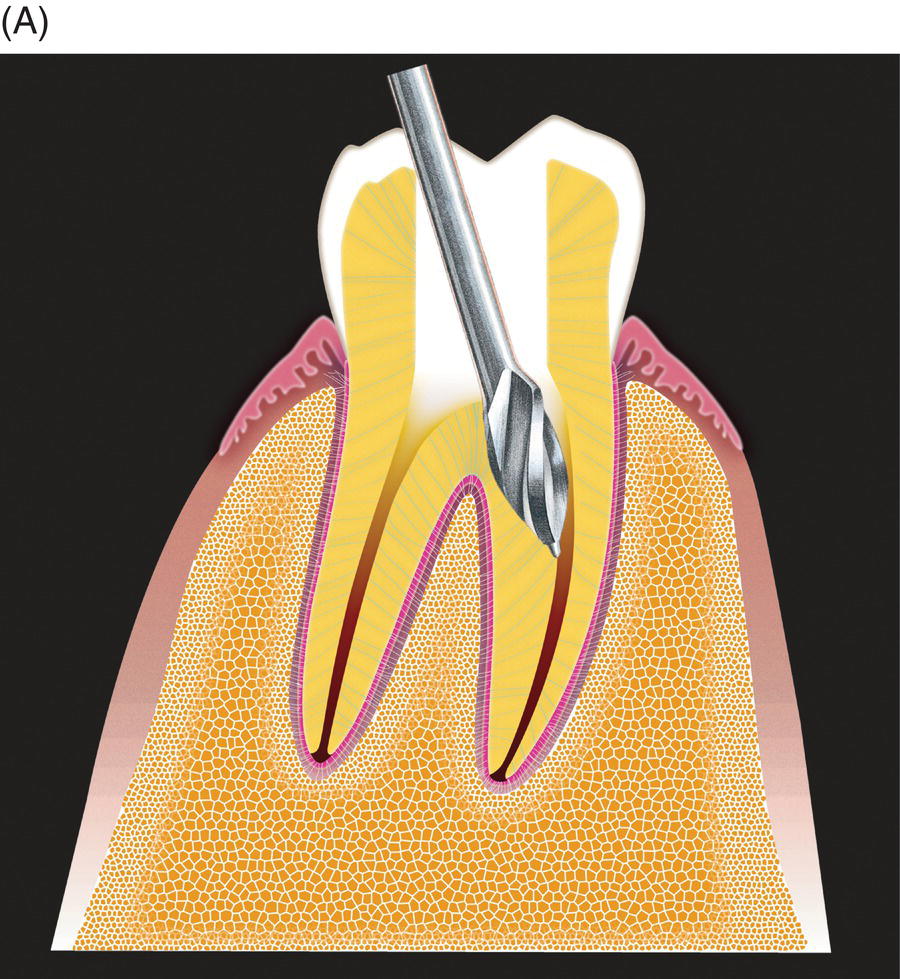
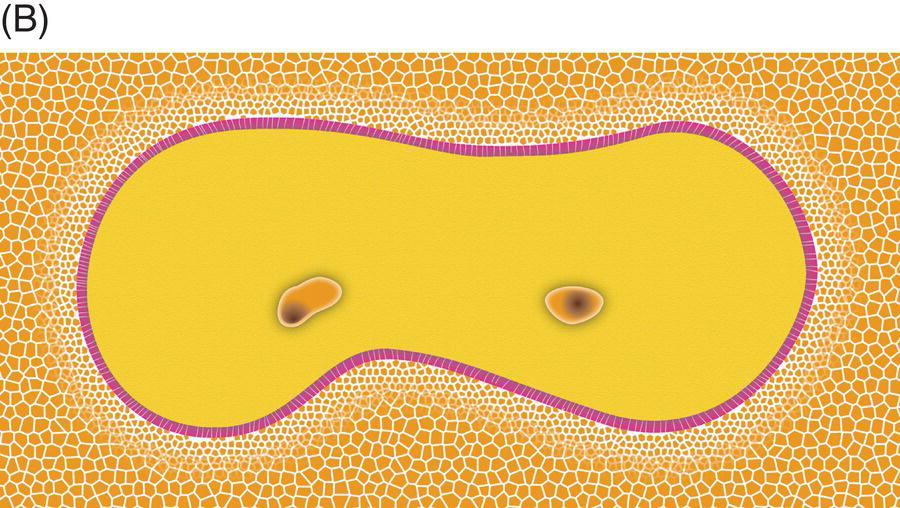
Fig. 7.8 (A) Using large rotary instruments for thin roots and (B) failure to recognize the proximity of canals to the furcation in multi-rooted teeth are the most frequent causes of strip perforation.
Resorption-related perforations (internal/external)
Internal resorption has a pulpal etiology. Routine endodontic therapy will prevent progression of the resorption, and the prognosis is excellent if the treatment is performed prior to perforation into the periradicular tissues. MTA repair is not necessary if the resorption is intercepted prior to perforation. However, MTA may be the obturation material of choice if perforation is detected (Fig. 7.9).



Fig. 7.9 (A) Internal resorption of pulpal origin. (B) Routine endodontic therapy was performed in the apical portion of the root using gutta-percha and sealer. MTA was used to fill the defect as obturation material. (C) A radiograph taken 1 year later shows excellent results.
Inflammatory external resorption may perforate into the pulp canal space (Fig. 7.10). The prognosis depends on the etiology of the resorption and the amount of dentin loss. Replacement resorption (ankylosis) is caused by loss of the cementum barrier. Most commonly, this phenomenon is associated with the replantation of avulsed teeth. MTA is of questionable value for stopping this process. Inflammatory resorption may be arrested with MTA obturation if the etiology is associated with a necrotic pulp. However, the prognosis is guarded.


Fig. 7.10 (A) An extracanal invasive root resorption is present in the mandibular second premolar. After root canal cleaning and identifying the portal of entry into the root canal, the entire root canal was filled. (B) A radiograph taken 2 years later shows this procedure has stopped the root resorption.
FACTORS INFLUENCING PROGNOSIS FOR REPAIR (TABLE 7.1)
Table 7.1 Perforation location: single-rooted teeth.
| Location | Repair material | Considerations |
| Coronal to crestal bone | Geristore, amalgam, composite, glass ionomer cement | Difficult to control placement of repair material May require surgery May compromise esthetic result |
| Cervical third of root apical to crestal bone | MTA ± collagen matrix | Decreased prognosis if periodontal pocket communicates with perforation Canal patency difficult to maintain MTA must set (1 week) prior to obturation |
| Middle/apical third of root | MTA ± collagen mat/> |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


