Chapter 7
Problem-Solving Challenges in Dentin Hypersensitivity and Vital Pulp Therapy
Problem-solving challenges and concerns with dentin hypersensitivity and vital pulp therapy addressed in this chapter are:
“The task of keeping alive the exposed healthy pulp demands an undamaged pulp, capable of reacting to treatment. Damage to the enamel, be it of a chemical, mechanical, or bacterial nature and to a greater degree similar damage to the dentine of the tooth, may affect the pulp and the adjoining odontoblasts. Apart from caries prophylaxis and the early treatment of carious defects in the human dentition, dental treatment if carried out with the necessary understanding of the basic physiology of the dental tissue, can often keep alive the vital pulp of the tooth, which as an organ for nourishing and registering stimulation has to fulfill an important function.”< ?xml:namespace prefix = "mbp" />
Dentin Hypersensitivity: Patient Considerations, Etiologies, and Treatment Issues from an Endodontic Viewpoint
One of the more challenging problems to deal with in dentistry is to maintain teeth in symptom-free function over the life of the patient. Over time through normal wear, function, and maintenance, some teeth create a “sensitivity” problem for the patient to a point where the patient is alerted to teeth that give them a shooting sensation, a tingling sensation, sometimes a painful sensation, or at times just a different feeling during normal daily activities. The teeth may or may not be painful, depending on the patient’s perception, pain threshold, and emotional and physical factors.
In some cases, the patient can identify the problem tooth and go directly to the sensitive part of it; in other situations, the problem is not focused and rather vague but very real. Daily, these patients are referred for an endodontic evaluation or are sent to have root canal treatment. In most circumstances, root canal treatment is unwarranted, but the patient feels that their dentist does not know what to do about the sensitivity that is present and has been for a period of time. A root canal procedure will certainly solve the problem. This is the quick fix and unfortunately occurs in many private-practice settings. However, the real question is whether this degree of treatment is truly indicated and in the best interest of the patient. In the bigger picture, the patient needs a diagnosis and treatment plan to maintain the vitality of the dental pulp in a particular tooth or teeth and if possible to restore symptom-free function.
Tooth hypersensitivity, or more frequently identified as dentin hypersensitivity, is defined as a short pain arising from exposed dentin in response to stimuli. Typically, thermal, evaporative, tactile, osmotic, or chemical stimuli produce responses which cannot be ascribed to any other form of dental defect or disease
The two most common etiologies have been identified as gingival recession and attrition,
With the first etiology, a simple evaluation using a fiberoptics (transillumination),
Desensitization techniques and minimally invasive procedures to eliminate the patient’s hypersensitivity would seem to be the treatments of choice to manage the patient’s chief complaint in these situations. This approach goes hand in hand with the initial phases of vital pulp therapy. Many clinicians may not identify this approach to management as being within the scope of endodontics, because too often endodontics and the everyday use of the term are erroneously equated only with root canal treatment. Treatment modalities for vital pulp therapy do fall within the scope of endodontics and should be considered first before doing a root canal procedure.
Directives for Considering Vital Pulp Therapy
It is a reasonable goal of endodontic research to seek diagnostic and treatment methods that more predictably determine the status of the dental pulp and preserve the vitality of the pulp under all conditions, especially when the vital pulp has exposed. Preserving pulpal vitality would have several advantages. The current techniques of vital pulp capping or pulpotomy are much less complicated and time consuming than root canal procedures. From a public health perspective, reduction of the number of teeth requiring root canal treatment would lessen the economic burden of dental care and increase tooth retention.
Are Vital Treatment Procedures Viable Options in Contemporary Dentistry?
Yes, pulp capping can play a major role in pulp and tooth retention. Recent studies have provided a great insight into the pulpal responses to irritants (see
When challenged by irritants, the pulp has an amazing capacity to form a hard, reparative tissue, sometimes in the form of its original tissue, tubular dentin (
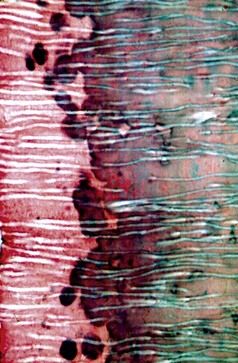
FIGURE 7-1 Normal tubular dentin showing mineralized, unmineralized, and partially mineralized dentin.
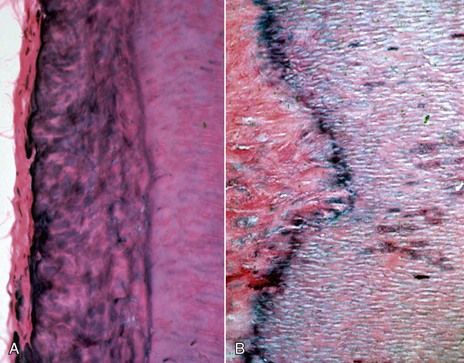
FIGURE 7-2 A, Gnarled dentin in apposition to normal dentin. B, Gnarled, irregular, irritational dentin (left) with evidence of the calciotraumatic line. Note normal dentin (right) and bacteria that have penetrated the tubules.
Ideally, the clinician should strive to prevent a pulpal exposure, especially under optimal conditions when there are no signs or symptoms of pulpal pathosis. A step-wise approach to caries excavation known as an indirect pulp cap is one possible treatment option that may prevent an exposure and allow for remineralization of the affected dentin or stimulate the formation of dentinal sclerosis and irritational dentin.
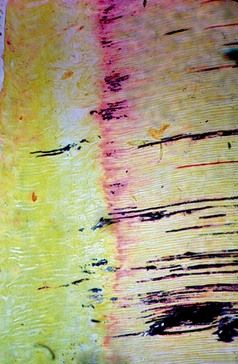
FIGURE 7-3 Irregular, irritational dentin (left), presence of the calciotraumatic line, and bacteria in the tubules. Note how some of the bacteria have passed through the calciotraumatic line into tubules that formed with the irritational dentin.
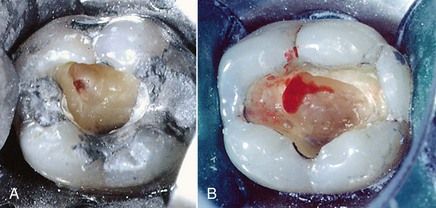
When signs or symptoms are not of consideration and an exposure occurs, the visual appearance of the exposure (
When Is Treatment of the Vital Pulp Preferable to Root Canal Treatment?
Possibly the most important indication for vital treatment procedures is in the case of pulpal exposures on teeth with incomplete root formation. In these cases, preservation of pulpal vitality is an essential objective for all exposures—whether traumatic, mechanical, or carious—to permit normal apexogenesis. Removal of the pulp immediately eliminates the possibility of further root development, leaving the root canal with an open apex and the root itself with thin dentinal walls that cannot undergo thickening, owing to loss of the radicular pulp. Root canal procedures in teeth with open, immature apices are more complicated, more time consuming, and less predictable in terms of outcome. Teeth with large-diameter canals and thin-walled roots are more prone to fractures of all types.
Fortunately, the pulps of teeth with immature root formation have a more generous blood supply than teeth with fully formed roots and apical closure. As a consequence, they are more tolerant of injury and exposure to microorganisms. Vital treatment procedures are far more likely to succeed in teeth with open, immature apical development than in teeth with mature root formation. With these factors in mind, vital techniques should be considered even when symptoms of pulpitis are present.

PROBLEM SOLVING
Problem
A 9-year-old male was brought to the dentist with a fractured maxillary right central incisor. The tooth had symptoms of irreversible pulpitis. There were prolonged pain reactions to cold, and the patient had experienced episodes of moderate spontaneous pain relieved by over-the-counter analgesics. The parent related that the tooth was fractured in a playground accident at school a month earlier. There had been little pain initially, and because of the Christmas holidays, no treatment was sought. Clinical examination indicated a complete midcoronal horizontal fracture with exposure of the coronal pulp. The periapical film indicated that the tooth had an open, immature apex and the apical periodontal ligament space was widened 2 to 3 mm more coronally than what would be typical of a normal physiologic apical formation (
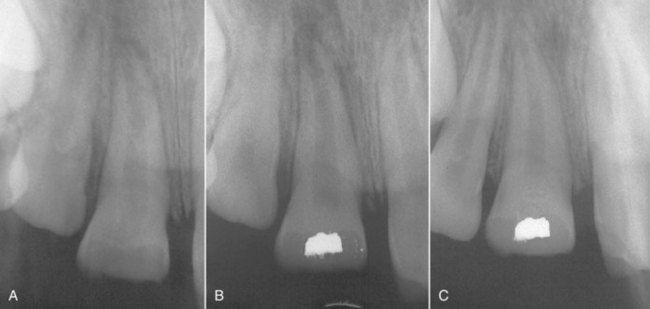
FIGURE 7-5 A, Traumatic fracture of a maxillary right central incisor in a 9-year-old boy. The tooth was examined approximately 1 month after the accident and was symptomatic of irreversible pulpitis. B, Postoperative radiograph of Cvek pulpotomy with calcium hydroxide. C, One-year reevaluation radiograph. The tooth responded normally to pulp testing, and the apex was closed.
Solution
Although the symptoms and radiographic appearance of the periapical tissues suggested an irreversible pulpitis, the potential problems associated with root canal treatment of the open apex highlighted the need to consider a form of vital therapy. A direct pulp cap (partial pulpotomy, also known as the Cvek technique), was performed with calcium hydroxide,
Discussion
This case was treated more than 30 years ago with materials available at the time, which were limited. Fortunately, the choice of materials has improved, and the prognosis for pulpal healing has improved as well. Nevertheless, the preoperative conditions were no different than many cases today, so this case illustrates the reparative potential of pulp tissue in teeth that exhibit immature root development. Had this treatment approach failed, apexification (techniques for nonvital pulps) would have been indicated (see

There is growing evidence that vital pulp treatment is effective for carious exposures on permanent teeth. Clinicians must remember that a carious exposure does not necessarily imply that bacteria actually reached the dental pulp. Often the demineralized front of dentin that contains bacterial byproducts has reached the pulp, but not the bacteria themselves. Studies have found that with techniques to be described, both direct pulp caps and coronal pulpotomies can preserve pulpal vitality with a very high degree of predictability.
When Is Root Canal Treatment Preferable to Vital Pulp Treatment Procedures?
Preoperative pulp sensibility testing would be appropriate for teeth with large carious lesions, but some teeth may respond positively to tests and still have localized intrapulpal inflammation and tissue degeneration. Factors that have been cited as indications for pulpectomy are uncontrollable hemorrhage from the exposure site,
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses