7
Preventive and management strategies against toothwear
Following diagnosis and assessment, prevention and management efforts for toothwear must follow sound strategic principles to allow for, if required and desired, successful restoration and rehabilitation. Counselling patients and offering advice form an important part of the prevention and management of toothwear, and must be directed towards controlling risk factors as well as addressing any imbalances within the oral environment. The range of preventive adjuncts to supplement preventive advice is discussed later in the chapter. Toothwear and dental caries prevention principles differ significantly and cannot be utilised interchangeably (Table 7.1).
Table 7.1 Preventive considerations for toothwear and dental caries.
| Preventive considerations | Toothwear | Dental caries |
| Preventive advice | Reduce dietary acids Improve salivary protection Remineralisation products WATCH strategy |
Reduce dietary sugars Improve oral hygiene Remineralisation products |
| Dietary emphasis | Reduce dietary acids Promote water rehydration Increase dairy |
Decrease frequency of sugars Increase dairy |
| Lifestyle factors | Crucial Detailed clinical history important Advise based on clinical history |
Important Sugar consumption habits |
| Oral hygiene advice | Limited Often have a good oral hygiene Soft toothbrush and gentle technique No brushing after acid exposure |
Important Flossing Toothbrushing technique Interdental brushes |
| Salivary protection | Important Sugar-free chewing gum Coincide acid exposure with times of high salivary protection |
Beneficial Coincide sugar consumption with times of high saliva protection at meal times |
| Adjunct therapies | Beneficial Sugar-free chewing gum Fluoride formulations CPP-ACP |
Important Chlorhexidine products Fluoride gels, pastes, rinses CPP-ACP |
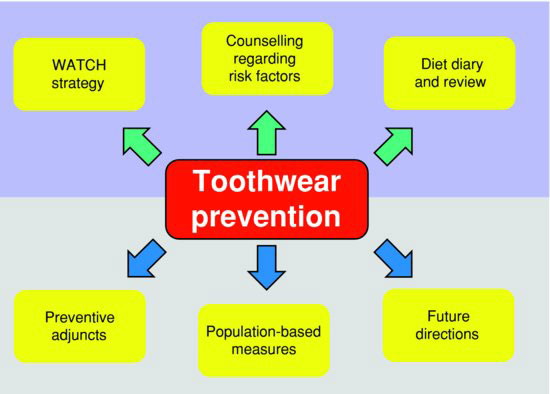
In offering preventive advice (Fig. 7.1) to patients with toothwear or at risk of its development, the approach taken must include the following:
- Discussion of risk factors in the patient’s lifestyle, work and sports environment, and diet
- Consideration of the patient’s health and any medications they may be taking
- The WATCH strategy introduced in this chapter
- Patient’s education and dietary diary review (see Chapter 3)
- Provision of information sheets or brochures to reinforce recommendations
Figure 7.1 Toothwear prevention strategies.
Advertising and dental health campaigns have increased awareness of the public in many parts of the world to the risks associated with frequent sugar consumption and the development of dental caries. Less awareness exists regarding dental erosion (Lussi et al. 2006) and the risks associated with high or frequent acidic food and beverage consumption. The focus of this chapter is patient-based prevention and management, and population-based measures will not be covered.
AIMING PREVENTION AT ALL AGES
Toothwear is a continuous process and a limited amount of wear continues physiologically as part of the aging process. Across the patient’s lifetime, alternating stages of active progression of toothwear and periods of stability occur (Fig. 7.2a). A patient may, under parental supervision, have had a good diet during childhood, whilst during teenage years and early adulthood changed lifestyle and dietary patterns with increasing consumption of acidic beverages. The same patient may in middle age have improved their diet and in later life, as health declined commenced taking medications that affected salivary protection of the dentition. This simple example details subtle variation over time that would fluctuate the rate of toothwear progression due to changes in diet. As considered in Chapter 6, the clinical history often identifies many risk variables.
Figure 7.2 Toothwear across a lifetime involves alternating stages of toothwear progression (red) and stability (green). The arbitrary total amount of tooth structure lost over a lifetime increases with age and progresses more rapidly at certain times (a). Three different patients will, over their lifetime, experience differing amounts of toothwear (b). Individual A experienced a high rate of wear (red) in the deciduous and mixed dentition phases. The high rate of wear continued in adolescence and slowed during middle age when toothwear processes were minimal (green), increasing again at a later stage in life. Individual B experienced a slow rate of wear up until the teenage years, rapidly progressed during young adulthood and then stabilised during middle age, again accelerating in older age as health declined. Individual C went through life with relative stability and only minimal physiologic toothwear considered normal for age.
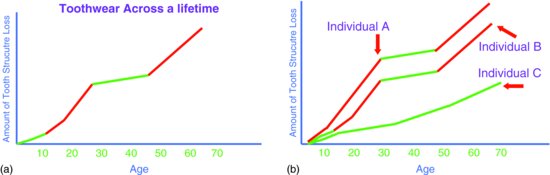
Variation of toothwear progression also exists from one patient to the next. Some may experience minimal wear throughout their lifetime, whilst others more severe toothwear (Fig. 7.2b). Previously considered cases highlight such variation. The 11-year-old male patient in Fig. 1.14 had severe toothwear from a very young age. The 24–year-old male athlete shown in Fig. 1.8 developed severe toothwear during young adulthood. When considering the appropriate preventive and management strategy for a patient, these arbitrary considerations are relevant as they identify that a patient presenting clinically may attend whilst in a period of:
- relative stability with past toothwear experiences;
- slow or rapid active progression;
- relative stability but at significant risk of developing considerable toothwear.
Preventive efforts must target all age groups, but the advice offered differs. Advice offered must be age appropriate, and variation in the preventive approaches applied for a patient must consider potential risks in the patient’s lifestyle, medical history and environment, as determined by the clinical history interview. Young children and their parents must be advised of erosive potentials of foods and beverages and consumption habits to avoid. Young adults in the under-30-year age bracket, who frequently consume acidic beverages particularly during and after physical activity and as a means to rehydrate, need to be counselled accordingly. This group of patients is often of good health, and instead work- and sports-related dehydration and outgoing lifestyles need further evaluation. A third broad group are elderly patients who have developed health-related issues and are on short- and long-term medications that affect salivary protection or themselves may be acidic. The key in all three groups is to provide advice based on the imbalance identified in the oral environment.
Imbalance in the oral environment
The ultimate aim of preventively based management is to avoid all further imbalances in the oral environment in order to conserve remaining tooth structure, whilst restoration and rehabilitation aim to improve or correct problems created through past imbalances. Management must include a component reinforcing prevention. Prevention must include consideration of all external influences on the oral environment that may alter this equilibrium.
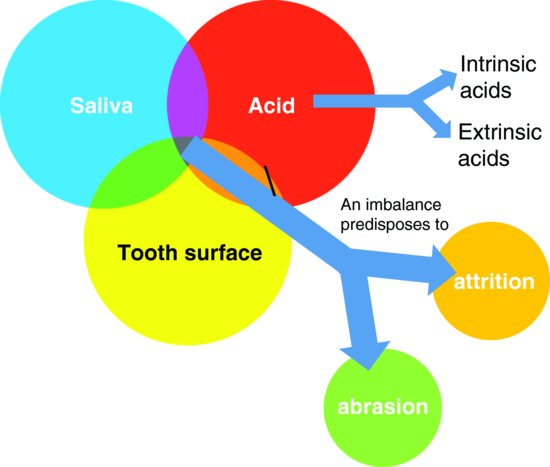
Tooth surfaces are demineralised by intrinsic and extrinsic acids and are protected by saliva. Excessive acidic influxes with or without reduced saliva protection promote dental erosion processes, which in turn potentiates further attrition and abrasion. The provision of targeted prevention and management modalities requires the complexity of underlying aetiological processes to be addressed (Fig. 7.3).
Figure 7.3 A tooth surface is protected by saliva from intrinsic and extrinsic acids. An imbalance to these components results in dental erosion that may further predispose to accelerated tooth structure loss from abrasion and attrition processes.
LIFESTYLE, HEALTH AND ENVIRONMENTAL RISK FACTORS
A central component for prevention of toothwear involves patient counselling regarding any potential or identified risk factors. This process should involve all members of the dental team – including dental assistants, therapists and hygienists – and not just the dentist. Preventive strategies foremost must address and reduce any risks the patient’s lifestyle, health and environment may place detrimental pressures on their health and dentition. Appreciating these potential risks and identifying those that may apply to a patient allows counselling and discussion to commence to eliminate, minimise or control them. Preceding chapters have identified various health- and medication-related toothwear risks factors (Table 7.2). Patients identified with these factors should be considered at a high risk for further toothwear and managed with a strong preventive emphasis.
Table 7.2 Health and medications affecting toothwear.
| Health-related considerations | Risk factors potentiating toothwear processes |
| Gastric reflux and conditions involving intrinsic acids |
|
| Medications |
|
| Chronic alcoholics |
|
| Rare genetic conditions |
|
| Conditions of dietary alteration |
|
Whilst health ailments may create moderate and even severe toothwear in the subset of patients affected by ill health or on medications with side effects, such as salivary reduction, the predominant group of patients affected by moderate and severe toothwear are commonly healthy.
Table 7.3 Lifestyle-related acceleration of toothwear processes.
| Lifestyle-related factors | Risk factors potentiating toothwear processes |
| High-frequency acidic beverage consumption |
|
| Sports enthusiasts |
|
| Diet- and health-conscious individuals |
|
| Partygoers with episodes of binging |
|
| Stress |
|
| Patients with habits |
|
Table 7.4 Work-related risk factors potentially accelerating toothwear processes.
| Work environment | Risk factors potentiating toothwear processes |
| Shift workers |
|
| Outdoor workers |
|
| Office workers |
|
| Wine tasters |
|
| Work with abrasive elements |
|
| Work with industrial acids |
|
Lifestyle risk factors are most important in the majority of patients, and preventive focus must consider these risks (Table 7.3) Lifestyle changes throughout life and is never constant. Parental guidance dictates lifestyle in childhood, whilst from young adulthood onwards, the individuals choose their own leisure, sports and day-to-day activities and dietary consumption. Consumption of acidic beverages contributes significantly to the dental erosion component and toothwear in many individuals (Jarvinen et al. 1991; Lussi et al. 2004; Nunn 1996).
A great proportion of adult life is spent within the work environment. Often a regular daily routine evolves, including dietary consumption patterns. The work environment itself is important in certain circumstances and may present an environmental risk factor (Table 7.4). Whilst often not as severe a risk as health, lifestyle or dietary factors, work-related risks tend to develop slowly over many years and affect a subset of the population.
When discussing lifestyle, health and work parameters with a patient, the dental team aims to ascertain the following:
- Frequent consumption of acidic foods and beverages
- Sports- or work-related dehydration reducing salivary protection
- Acidic beverage rehydration at times of dehydration
- Health-related changes
- Medications affecting salivary protection
- Work-related exposure to acids or abrasive
- Or any combination of the above
- Any detrimental habits or dietary preferences ‘Before the last line’ or any combination of the above
Having identified and discussed these risks, a strategy to convey preventive advice is required.
THE WATCH STRATEGY
Any strategy proposed for toothwear prevention, if it is to be effective, must be straightforward, easily understood and agreed to by the patient. It needs to be in line with the best advice of dietitians, nutritionists and the medical profession.
The authors have formulated the WATCH strategy (Fig. 7.4), which is central to preventive counselling advice offered to any patient presenting with toothwear to allowing a tailor-made preventive approach to be communicated (Young 2005). The WATCH strategy is a preventive approach encouraging a lifestyle that is both healthy and dentally healthy, irrespective of whether patients present with significant toothwear or not.
Figure 7.4 The WATCH strategy (Young 2005) for preventing toothwear.
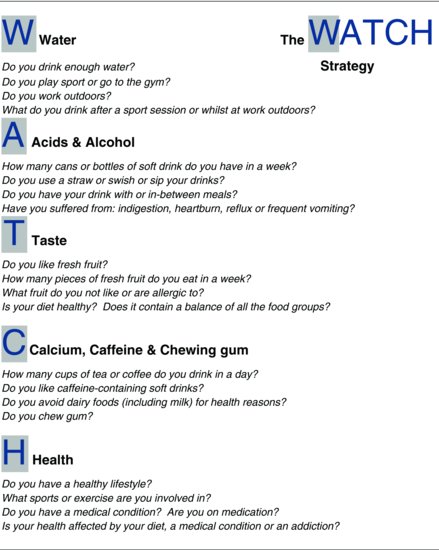
For toothwear patients, this strategy can be applied either subsequent to in-depth clinical history-taking or at the review appointment at which time the diet diary is also reviewed. For all other patients presenting for routine dental examinations and treatments, the strategy can provide a succinct line of questioning and dentally relevant lifestyle advice therefrom to help reduce the risk of developing toothwear. Patients should be provided with an information sheet or brochure to reinforce key recommendations made during counselling in the clinical setting (Fig. 7.5). In training dental team members to follow the line of questioning for patients, the dentist can advise staff members to discuss the key abbreviated summary points of the WATCH strategy with the patient (Tables 7.5 & 7.6).
Figure 7.5 The WATCH strategy information sheet for patients detailing 20 key recommendations for preventing toothwear. (From Khan et al., 2010, with permission of Copyright Publishing Pty Ltd.)
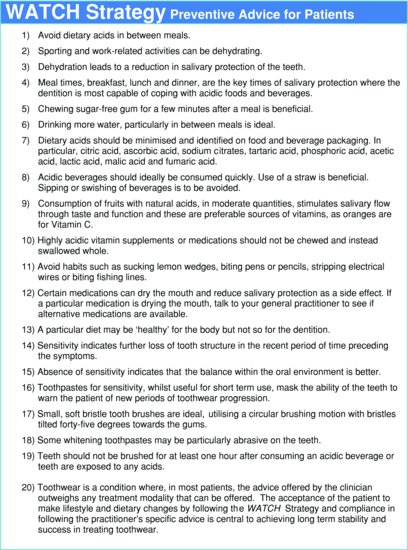
Table 7.5 Key discussion points for the WATCH strategy – water, acids and alcohol, taste.
| Key discussion points for water |
|
| Key discussion points for acids and alcohol |
|
| Key discussion points for taste |
|
Table 7.6 Key discussion points for the WATCH strategy – calcium, caffeine and chewing gum and health.
| Key discussion points for calcium, caffeine and chewing gum |
|
| Key discussion points for health |
|
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


