7 Local Anesthesia
In modern endodontic treatment, dental local anesthesia has a central role in treatment planning. Additional measures such as intravenous premedication, intravenous sedation, or general anesthesia are necessary only in exceptional cases.
However, the various risk factors that may be present (e.g., the increasing number of older patients and those with pre-existing medical conditions or taking long-term medications for systemic conditions) demand an individualized approach that takes the risks into account. Available local anesthetics, vasoconstrictors, and application techniques should be optimally used for each individual patient. At approximately 4.5%, the rate of complication associated with the use of local anesthesia is low, and life-threatening complications are extremely rare (Daubländer, 1997).
Local anesthesia in dentistry involves reversible blockade of stimulus propagation either from the peripheral nerve endings (e.g., infiltration anesthesia, periodontal ligament injection) or at the level of the peripheral nerves (block anesthesia). In addition to their effect on vegetative and sensory functions, increasing concentrations of local anesthetics can cause inhibition or reduction of motor neuron functions and paralysis can occur. At the molecular level this happens through a specific, receptor-mediated blockade of voltage-gated sodium channels of the neuronal axon. This leads to inhibition of formation and further transmission of action potentials. The sodium channels are present throughout the body and represent an important signal conduction system. Therefore, at a sufficiently high systemic concentration, local anesthetics can elicit systemic nerve blockage. Possible consequences are disturbances of the central nervous system and the cardiovascular system.
All local anesthetic solutions have the same basic chemical structure, consisting of three components (Niesel, 2003):
• an aromatic residue that is responsible for the lipophilic characteristics;
• a substituted amino-nitrogen compound, which is hydrophilic;
• an intermediate chain, whose length is responsible for the intensity of the anesthetic effect, and differentiation in esters and amides.
Ester-type solutions are metabolized and rendered nontoxic by cholinesterases in tissues and blood. The amides are primarily metabolized in the liver. For injectable solutions only amides should be used, whereas esters are still appropriate for superficial anesthesia (tetracaine or benzocaine) (Malamed, 2004).
Local anesthetic solutions must change their charge potential twice in order to reach the receptors on the inner surface of the nerve membrane. The local anesthetic molecules can only diffuse in their basic state. Local anesthetic solutions exist as hydrochloride compounds. Therefore they have to be neutralized by local tissue buffers to achieve a basic and diffusion-capable state. Following penetration of the multilayered neuronal membrane, the molecule releases the accumulated hydrogen ions, and then remains nonprotonated and can interact with the receptors.
Depending upon the diameter of the nerve and the presence of a myelin layer, a sequence of nerve blockade occurs. Clinically, pain and temperature sensitivity (C- and Aδ fibers) is blocked.
Local Anesthetic Solutions (Amides)
Lidocaine is a common local anesthetic and antiarrhythmic drug that is used worldwide; it is also the oldest amide preparation. Lidocaine is typically used as a 2% solution with epinephrine as vasoconstrictor (usually 1:100 000). It should be available as an alternative local anesthetic.
Articaine has potency similar to lidocaine, but is less toxic because it is metabolized primarily in the tissues and blood. For dental use, it is available as a 4% solution with and/or without epinephrine. Because of its high protein-binding capacity, it is also indicated for use in pregnant women. An epinephrine concentration of 1:200 000 or 1:400 000 is sufficient for routine dental procedures.
Mepivacaine can be used without a vasoconstrictor because it possesses certain vasoconstrictor effects. It should be used as a 3% solution, but has a relatively short period of efficacy.
Bupivacaine, the most potent but most toxic local anesthetic drug, is effective up to 6 hours even without epinephrine. Therefore it is indicated for long-term anesthesia and pain control.
Maxillary anesthesia
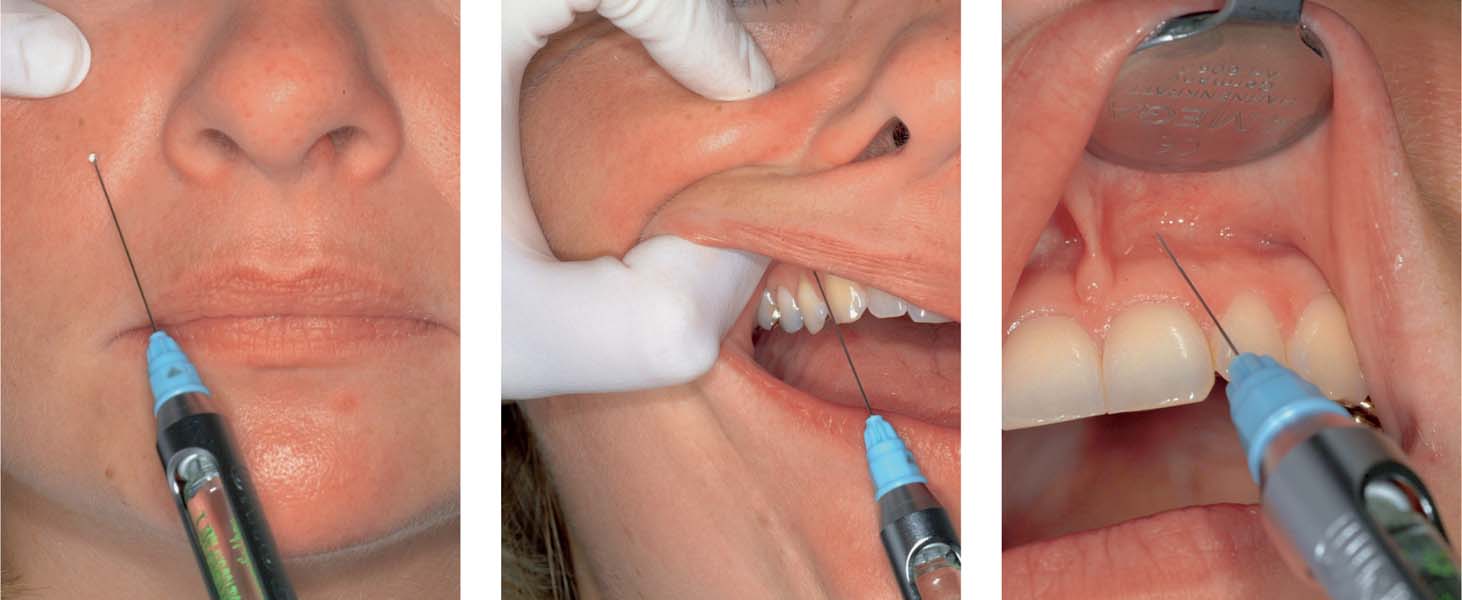
7.1 Block anesthesia of the infraorbital nerve
Left: Extraoral injection site.
Middle: Intraoral technique (injection). It is important to palpate the infraorbital foramen as the needle is inserted. With this intraoral approach the canine is the primary landmark for both the choice of injection site and the direction of insertion of the needle.
Right: Infiltration anesthesia in the labial region.
7.2 Nerve block anesthesia
Left: Block anesthesia of the nasopalatine nerve. The direction of entry of the needle is from the corner of the mouth on the opposite side and it is inserted until contact is made with the bone.
Right: Block anesthesia of the nasopalatine nerve. Approaching from the opposite side of the mouth, the needle is inserted adjacent to the papilla only a few millimeters deep.
Vasoconstrictors
Since virtually all local anesthetics lead to vasodilation, a vasoconstrictor should be used along with them, as long as there are no contraindications. This improves the depth of anesthesia and lengthens the therapeutic period of efficacy, while reducing reabsorption and therefore limiting the systemic plasma levels. The agent of first choice is the catecholamine epinephrine. Octapressin has a delayed and weaker effect; epinephrine no longer/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses