8 Emergency Endodontics
The dentist in general practice is most often confronted with pain of endodontic origin. Carious lesions (also secondary caries) are the primary culprit in 88% of cases, followed by cusp fracture, hypersensitive cervical areas, and traumatic occlusion. If the patient can identify the responsible tooth, or a radiograph reveals apical pathology, or there are additional clinical symptoms (e.g., sensitivity to percussion or a fistula) that provide clues about the affected tooth and the overall pathophysiologic situation, a treatment decision should be made quickly. If the patient reports radiating pain not directly related to a specific tooth, symptomatic treatment should be initiated.
Clinical studies have reported varying rates of success following direct pulp capping as an emergency treatment measure, ranging from 97.8% after 1.5 years to 61.4% 5 years later. In one clinical study, the success rate of 37% after 5 years dropped to only 13% after 10 years. Similar clinical studies following immediate extirpation of the exposed vital pulp found significantly higher success rates. For example, Rocke reported a 5-year success rate of 93% for all endodontically treated teeth, and a 10-year success rate of 81%. An exception to these excellent results were immature teeth with exposed pulps whose root growth was not yet complete.
8.1 Step one
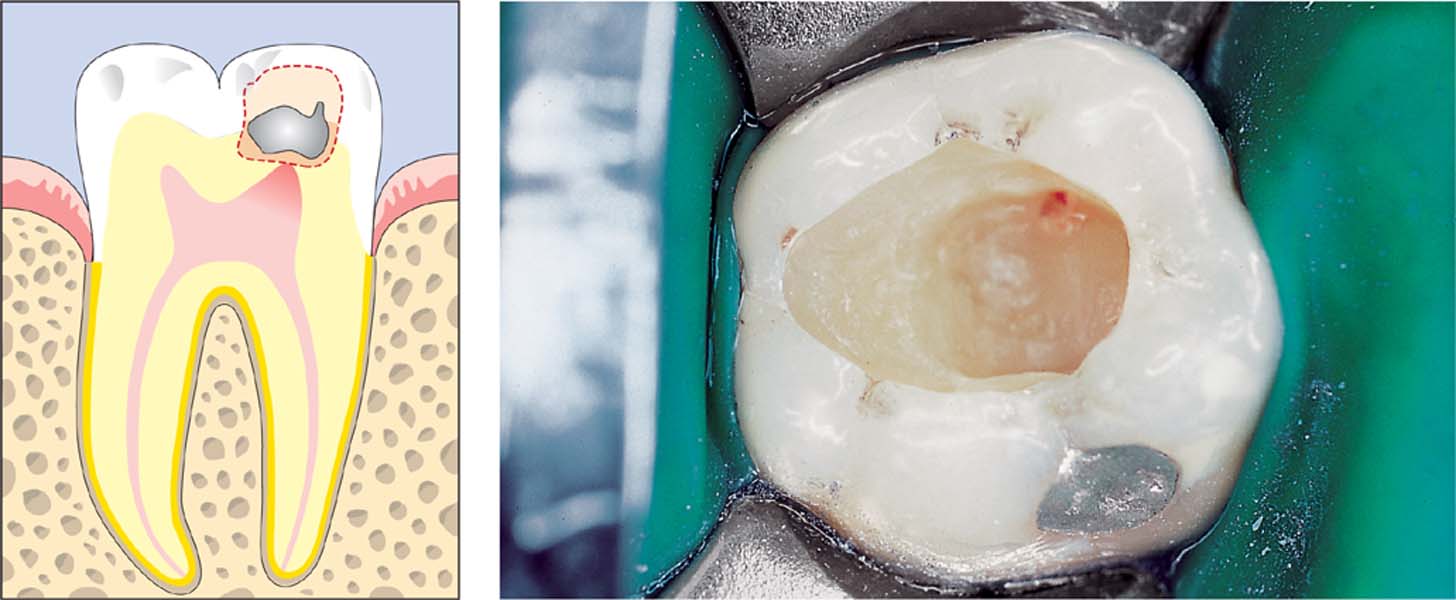
Hemostasis should be attempted immediately following a pulp chamber exposure.
Left: The caries lesion has not yet involved the pulp horn.
8.2 Step two
Apply a water-based calcium hydroxide paste as a thin layer and press it lightly with a sterile cotton pellet. Wait a few minutes to determine whether any blood seepage occurs; if this is the case, the pulp capping material should be washed out and reapplied after bleeding has been completely stopped. An excavator is used to remove any excess material so that only the root canal orifice is covered.
Left: Such pulp capping procedures may only be performed if the dentin is caries-free.
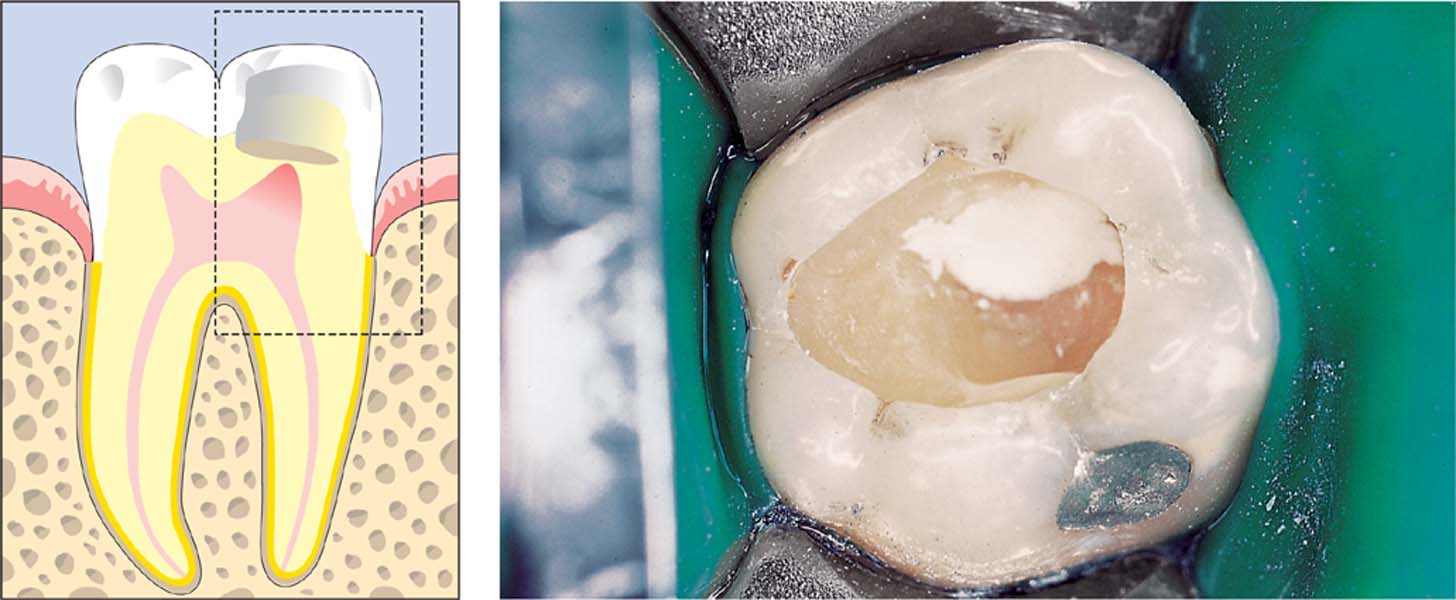
8.3 Step three
The calcium hydroxide capping material is covered with zinc oxide eugenol cement, followed by glass ionomer cement, and a definitive restoration using composite resin.
Left: Against the regenerating, inflamed pulpal tissue with temporary damage is a zone of reparative dentin (2), diffuse mineralization (3) and osteoidlike dentin (4) and the zone of necrosis (5). The calcium hydroxide paste (1) is covered with zinc oxide eugenol, and the cavity is then filled with glass ionomer cement and a composite restoration.
Pulpal Diagnosis
Before attempting any management of pain of dental origin, the clinician must establish whether the patient has irreversible or reversible pulpitis or necrosis with or without apical involvement.
The transition into irreversible pulpitis is gradual, making precise diagnosis very difficult. In the first instance, the pulp chamber is not directly violated, but there may be a fractured restoration, exposed dentin, or an inadequate restoration. Pain can be elicited by stimuli such as cold, sweet, and sour and is of short duration.
The standard sensitivity test is positive, but there is no pain on percussion. A radiograph usually reveals deep caries or an old restoration with secondary caries; there are generally no radiographic signs of periapical involvement. Pulpal diagnosis has as its goal the maintenance of tooth vitality while simultaneously eliminating pain. This will usually involve complete removal of all old restorations and caries; in no case should residual caries be left untreated. Only by these measures is it possible to eliminate the possibility of additional pulpal irritation. When the patient has been pain-free for 48 hours, the tooth can be restored. If pain persists or increases in intensity, it indicates that irreversible pulpitis is present. In such cases, the root canal must be appropriately instrumented endodontically and later definitively restored.
8.4 Diagnosis
Approximately 4 months after placement of a composite restoration, this patient presented with pain in the maxillary anterior region. The restorations were removed using a dental explorer; carious dentin that had not been completely removed is clearly visible. The caries was fully excavated, and the cavities were lined with zinc oxide eugenol cement with a low proportion of eugenol.
Right: The teeth were not sensitive to percussion, but in the radiograph the lateral incisor shows a slight widening of the periodontal ligament space.
8.5 Treatment
The primary and secondary caries beneath the inadequate restorations were removed as far as possible without exposing the pulp. Subsequently the cavities were temporarily restored for 24–48 hours, using a temporary filling material.
Right: On the next day, a definitive swelling in the right infraorbital area was evidence of the failure to make the expected pulpal diagnosis. Maintenance of tooth vitality was no longer possible and a soft-tissue incision was made. The following day the patient was free of symptoms.
8.6 Conclusion of treatment
After another 2 days, the root canals were instrumented in all three teeth and a calcium hydroxide dressing was applied loosely into the canals.
Right: Three weeks later, the patient was symptom-free and definitive root canal fillings were placed.
Devitalization of the Pulpal Tissues
An important component of all devitalization pastes is paraformaldehyde. It leads to coagulation and denaturation of cell wall proteins, which, finally, results in the arrest of all vital cell functions. The tissue becomes “fixed,” and this state of fixation is irreversible.
Animal experiments have demonstrated cellular toxicity, mutagenesis, carcinogenesis, and genotoxic changes. Using radioactively labeled paraformaldehyde, 14 days following pulpectomy, accumulation of metabolites in the liver has been observed. Systemic dissemination has also been observed in blood plasma, as well as in the lungs and kidneys.
With root canal fillings that are inadequately sealed, the result may be sequestrum formation in the adjacent bone, ultimately leading to tooth loss. Even with optimally sealed proximal restorations it is not always possible to inhibit the penetration of formaldehyde into adjacent bone, where damage can occur.
At the time of writing, there are no indications for devitalization of the pulpal tissues as “emergency” therapy. The numerous adverse effects far outweigh the potential beneficial effects.
8.7 Diagnosis
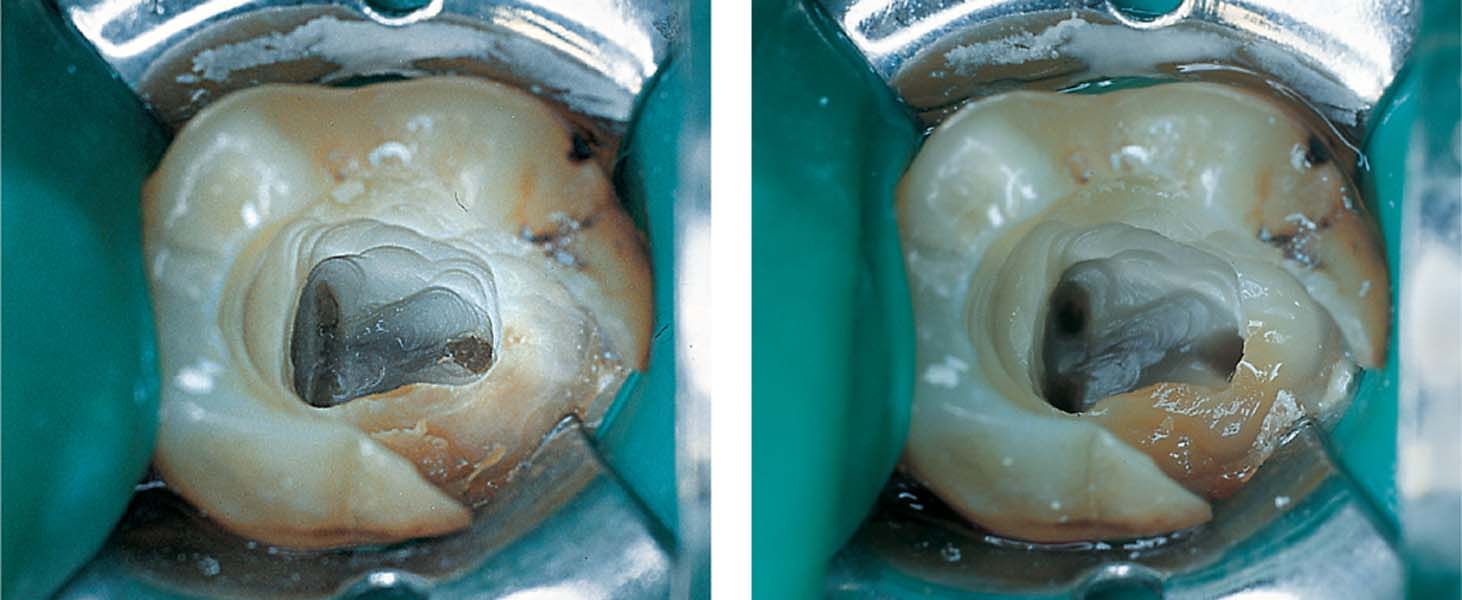
Left: Ten days after an emergency visit, this patient presented to her dentist’s office with continuing mild discomfort. Tooth 37 was isolated using a rubber dam. Following removal of the temporary restoration, a dark-gray devitalization paste was visible near the incompletely exposed root canals.
Right: The devitalization paste and residual carious dentin have been completely removed.
8.8 Treatment
Left: Following preparation of the access cavity and the removal of the fixed and non-bleeding coronal pulp tissue, the canal orifices became visible.
Right: The root canals were instrumented using the crown-down technique and thoroughly irrigated with sodium hypochlorite solution and EDTA.
8.9 Conclusion of treatment
Left: Following precise determination of root canal length, all the root canals were completely instrumented and a temporary dressing applied to each canal.
Middle: Following a symptom-free period, definitive root canal fillings were placed and the coronal aspect was definitively restored.
Right: A bony sequestrum, approximately 5 mm in size, was removed from the interdental area.
Emergency Involving a Vital Pulp: Amputation of the Coronal Pulp
Among emergency treatments of irreversible pulpitis, immediate endodontic treatment with extirpation and temporary filling provides the highest rate/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses