Chapter 7
Complications and Maintenance
Aim
The aim of this chapter is to discuss common complications in treatments involving the use of implants and to consider arrangements for the monitoring and maintenance of completed implant cases.
Outcome
After reading this chapter the reader should be familiar with the nature and management of common complications in treatments involving the use of implants. In addition, the reader should be familiar with arrangements for the monitoring and maintenance of completed implant cases.
Introduction
Complications may occur in both the surgical and prosthodontic phases of implant therapy. It is essential to warn patients of the possibility of surgical and postoperative problems. Failure of osseointegration is relatively rare in well-planned cases, with most failures occurring soon after surgical placement or before loading.
Complications in most cases are avoidable by careful attention to diagnosis, treatment planning and good surgical and prosthodontic planning, and by following established protocols of individual implant systems.
Surgical Complications
The more common, relatively minor complications following surgery include swelling, bruising and discomfort. All patients should be warned of these complications and the anticipated extent of them before surgery is undertaken.
As with all minor surgical procedures, surgical complications can be minimised by adequate anaesthesia, gentle surgical manipulation of both hard and soft tissues, pre- and postoperative analgesia, and careful postoperative wound management, including the use of pressure and ice packs to reduce swelling.
Haemorrhage may occur at the time of surgery if there is excessive trauma to soft tissue or damage to aberrant vessels within the bony cortex. Failure to establish good primary stability at the time of implant placement may result in early failure.
Incorrect positioning of implants at the time of surgery, as a consequence of poor planning or lack of necessary skills, knowledge and understanding may result in considerable difficulties during the restorative phase of treatment. It is essential to use surgical guides and templates if positioning problems are to be minimised (Fig 7-1).

Fig 7-1 Clinical view of an upper partial case displaying poor positioning of the implants in relation to the final tooth position.
Postoperative Pain
Mild postoperative pain is to be expected. It should, however, be readily controlled by means of non-prescription analgesics.
Severe pain following implant surgery is extremely rare. Patients with pain after 24 hours should be monitored for signs of infection, bleeding and other complications. In such situations there may well be an increased risk of implant failure.
The routine use of antibiotics pre- and postoperatively will decrease the possibility of infection. The practitioner must, however, be satisfied as to the indications to prescribe prophylactic antibiotics.
Wound Dehiscence
In the two-stage surgical technique, breakdown of the soft tissue following implant placement may lead to the exposure of the implant and cover screw (Fig 7-2). This may be the result of poor soft-tissue coverage of the implant or trauma from the prosthesis covering the surgical site. The diagnosis of the cause of soft-tissue breakdown needs to be established when planning further management of the case. In all cases the surgical sites must be kept clean with antiseptic mouthrinses, such as chlorhexidine, used as indicated clinically.
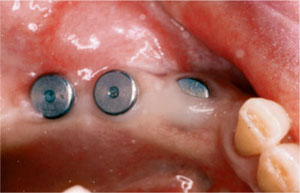
Fig 7-2 Wound dehiscence and exposure of cover screws.
Paraesthesia
Paraesthesia may arise following trauma to nerves in the region of the implant site. The trauma may be direct from drilling through, or at least into a structure, or indirect as a result of excess heat generation. Whatever the cause, trauma to sensory nerves may lead to loss of sensation to the lower lip (Fig 7-3).

Fig 7-3 A dental panoramic radiograph showing implant on lower right quadrant, which has been placed through the inferior dental nerve, resulting in paraesthesia.
Transient loss of sensation in the lower lip may occur from bruising and swelling of soft tissue around the mental foramina.
Permanent loss of sensation may be the result of damage to the inferior dental nerve. This should be avoided through careful radiographic assessment and including a safer margin for possible error in the planning of implant placement.
Damage to the incisive branch of the inferior dental nerve may result in patients complaining of parasthesia or anaesthesia to any remaining lower incisors.
Mandibular Fractures
In severely resorbed mandibles multiple implants may weaken the jaw with a resultant fracture. This is, however, very rare in suitably planned cases.
Complications Following Second-Stage Surgery
Second-stage surgery involves uncovering of the implant, removal of the cover screw, replacing i/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


