Periodontal Microsurgery
Dennis A. Shanelec, Leonard S. Tibbetts, Adriana McGregor and J. David Cross*
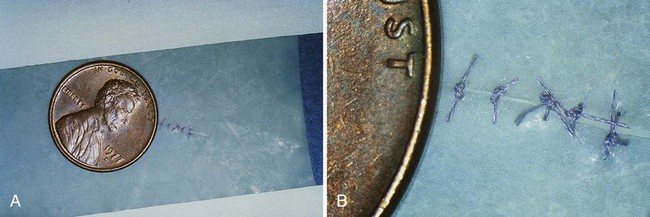
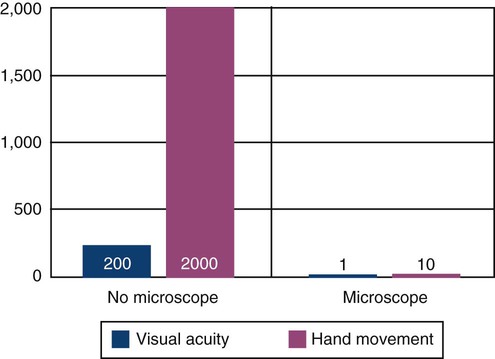
Microsurgery is defined as surgery performed under magnification of 10× or more which is only possible using a surgical microscope.5 The hallmarks of microsurgery are increased visual acuity and improved manual dexterity.17 When visibility is increased 10-fold, motor movement precision is increased from 1 mm to 10 µm.3 This is the approximate size of an epithelial cell.12 Large incisions for visibility are therefore not necessary. Small surgical instruments are used to advantage in the reduced surgical field (Figure 64-1). This minimally invasive philosophy results in less injury, diminished morbidity, and rapid healing.9,12 Central to this approach are sharp microsurgical blades to create incisions at a virtual cellular level (Figure 64-2). These incisions are closed with meticulous apposition to eliminate wound edge gaps and dislocations, allowing healing by primary intention to begin within hours of microsurgical closure. This circumvents the need for an extensive secondary mitotic stage of wound healing to bridge wound gaps and fill surgical voids.
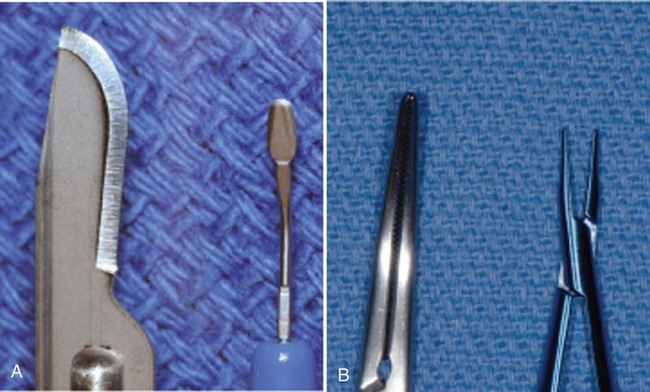
A, No. 15 blade versus ophthalmic blade. B, Working tip of conventional needleholder versus McGregor microsuturing forceps.

The red circle in the upper right image shows the area magnified in the lower right image. The green circle shows the disruption of only one epithelial cell. (SEM photographs courtesy Masana Susuki, DDS, Tokyo, Japan.)
Philosophy of Periodontal Microsurgery
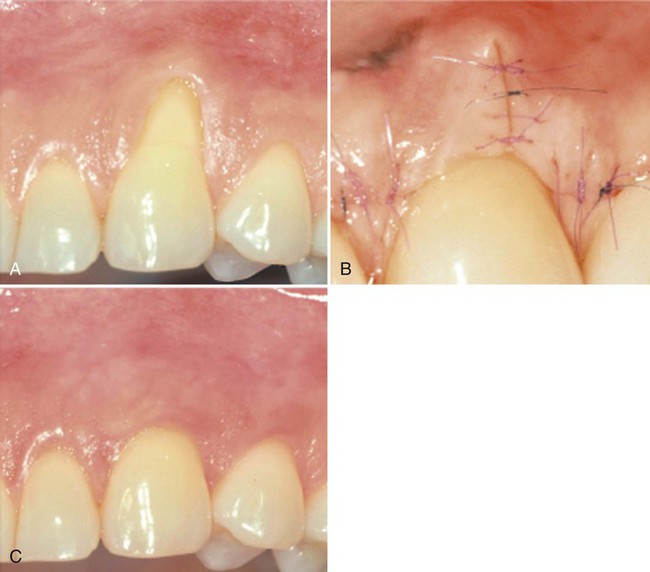
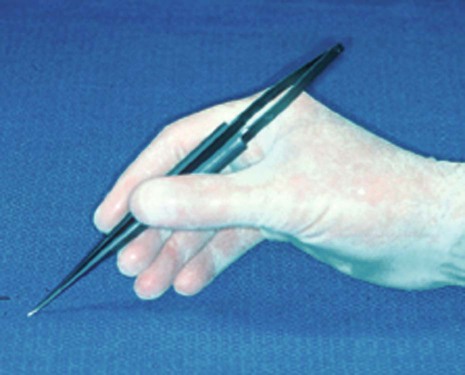
Microsurgery is a philosophy that embraces three core values. The first is enhanced motor skill for better surgical performance. This is accomplished through improved visual acuity and the use of a precise hand grip to increase accuracy and reduce tremor (Figure 64-3). The second is minimal tissue trauma, which is accomplished through smaller incisions and reduced surgical fields (Figure 64-4). The third value is primary passive wound closure.18 This is accomplished by microsuturing to eliminate gaps and dead spaces at the wound edge (Figure 64-5).

Minimal tissue trauma during incisions, surgical manipulation, and suturing is accomplished after microsurgical principles.
Advanced periodontics has an increasing need for clinical procedures that require intricate surgical skills. Regenerative procedures, periodontal plastic surgery, and dental implants are but a few of the surgical procedures that demand clinical performance that frequently challenge the skills of periodontal surgeons beyond the range of possibility with ordinary vision. Microsurgery establishes a minimal invasive surgical approach to periodontics exemplified by fewer vertical incisions and smaller surgical sites. Every field of microsurgery has noted the extent to which reduced incision size and less retraction directly relates to reduced postoperative morbidity and rapid healing2 (Figure 64-6).

In addition to the use of magnification and reliance on atraumatic technique, microsurgery requires specially constructed instruments designed specifically to minimize trauma. An important characteristic of microsurgical instruments is their ability to create clean incisions that prepare wounds for healing by primary intention. Microsurgical incisions are established at a 90-degree angle to the surface using ophthalmic microsurgical scalpels (Figure 64-7). Microscopy permits easy identification of ragged wound edges for trimming and freshening. For primary wound closure, microsutures in the range of 6-0 to 9-0 are needed to approximate the wound edges accurately (Figure 64-8). Microsurgical wound apposition minimizes gaps or voids at the wound edges and encourages rapid healing with less postoperative inflammation and less pain. Figures 64-9 and 64-10 illustrate periodontal surgery cases using microsurgical techniques.
Advantages of Microsurgery
Periodontal microsurgery raises the treatment bar in many ways. Surgical decision making is enhanced because the quality and quantity of visual data reaching the cerebral cortex is increased by a square of the magnification level. Ergonomic and body posture advantages also occur when using the surgical microscope1 (Figure 64-11). Issues, such as neuromuscular fatigue and occupational skeletal pathology, are reduced. Sitting comfort, good body posture, arm support, and controlled breathing are inherent to proper microscope use. Motor skills are enhanced through instruments designed for a precision grip of the hand. Titanium instruments are used for strength and lightness and are made with round handles to permit precise rotation (Figure 64-12). This reduces hand fatigue and tremor for precise surgical movement. Ergonomic benefit may be one of the most significant aspects of microscope use in periodontics.

An important aspect of periodontal microsurgery is technical improvement in surgical performance. Higher skill levels have been shown in many surgical disciplines and can be fully appreciated when a surgeon tries his or her hand under the microscope. Viewing surgery under the microscope impresses a surgeon with the coarseness of conventional surgical manipulation (Figure 64-13). What appears to the unaided eye as gentle surgery is revealed, under the microscope, as gross crushing and tearing of delicate tissues. Periodontics has long advocated atraumatic surgery, but the limits of normal vision have made this goal unattainable.

Proprioceptive guidance is of little value at the microsurgical level. Visual guidance is used for midcourse correction of scalpels and instruments to achieve the finest level of skill and dexterity.4,9 Incisions can be accurately mapped, flaps elevated with minimal damage, and wounds closed accurately without tension (Figure 64-14). Periodontal microsurgery is a natural progression from conventional surgical principles to a surgical ethic in which the surgical microscope is employed for the most accurate and atraumatic handling of tissue (Figure 64-15).

The end-point appearance of microsurgery is superior to that of conventional surgery. The difference is self-evident and often startling (Figures 64-16 to 64-18). As much as judgment and knowledge play a role in surgery, in the end, surgery is a craft. Surgeons appreciate this, especially when microsurgery raises their work to levels of artistic expression. Personal gratification in performing better surgery leads to acceptance of periodontal microsurgery by surgeons motivated to improve the quality of their work.


A, Improper placement caused unesthetic result. B, Microsurgical grafting procedure. C, Final surgical result after fabrication of new crowns.

A, Altered passive eruption covering teeth crowns. B, Immediate microsurgical postoperative result. C, Three weeks’ postoperative healing.
Another very important advantage of microsurgery is in the area of root preparation. The importance of root debridement is recognized universally as an essential component of periodontal therapy.10,17 Research in clinical dentistry has shown that microscope-enhanced vision more readily accomplishes the long-established clinical goals of endodontic and restorative dentistry. In periodontics, studies demonstrated that root debridement performed without magnification was incomplete. When debrided roots were examined with the aid of a mi/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses