Tooth Development and Eruption
Learning Objectives
New Key Terms
Accessory roots (ah-mel-oh-blasts)
Alveolar bone (ah-mel-oh-blasts)
Ameloblasts (ah-mel-oh-blasts)
Amelogenesis (ah-mel-oh-jen-i-sis), imperfecta (im-per-fek-tah)
Anodontia (an-ah-don-she-ah)
Apposition (ap-oh-zish-in)
Cells of the dental papilla (pah-pil-ah): central, inner, outer
Cementoblasts (see-men-tah-blasts)
Cementocytes (see-men-toe-sites)
Cementogenesis (see-men-toe-jen-i-sis)
Cementoid (see-men-toyd)
Cervical loop (ser-vi-kal)
Concrescence (kahn-kres-ens)
Dens in dente (denz in den-tay)
Dental lamina (lam-i-nah), papilla (pah-pil-ah), sac
Dentigerous cyst (den-ti-jer-os)
Dentin dysplasia (den-tin dis-play-ze-ah)
Dentinal tubule (den-tin-oh-jen-i-sis), imperfecta (im-per-fek-tah)
Dentinogenesis (den-tin-oh-jen-i-sis), imperfecta (im-per-fek-tah)
Dentition (den-tish-in): permanent, period, primary, mixed
Ectomesenchyme (ek-toe-mes-eng-kime)
Enamel epithelium (ep-ee-thee-lee-um): inner, outer
Enamel knot, organ, dysplasia (dis-play-ze-ah), pearl
Epithelial rests of Malassez (ep-ee-thee-lee-al mal-ah-say)
Eruption: active, passive (fu-zhin)
Fusion (fu-zhin)
Gemination (jem-i-nay-shin)
Hertwig’s epithelial root sheath (hirt-wigz)
Junction: dentinocemental, dentinoenamel (mak-roe-don-she-ah)
Macrodontia (mak-roe-don-she-ah)
Matrix (may-triks): enamel (ih-nam-l)
Microdontia (mi-kro-don-she-ah)
Nasmyth’s membrane (nas-miths)
Nonsuccedaneous (non-suk-seh-dane-ee-us)
Odontoblasts (oh-don-toe-blasts)
Odontoclasts (oh-don-toe-klasts)
Odontogenesis (oh-don-to-jen-eh-sis)
Oral epithelium (ep-ee-thee-lee-um)
Periodontal ligament (pre-ah-mel-oh-blasts)
Preameloblasts (pre-ah-mel-oh-blasts)
Predentin (oh-don-toe-blast-ik), Tomes’ (tomes)
Process: odontoblastic (oh-don-toe-blast-ik), Tomes’ (tomes)
Proliferation (pro-lif-er-ay-shin)
Reduced enamel epithelium (ih-nam-l ep-ee-thee-lee-um)
Repolarization (re-po-ler-i-za-shun)
Stage: bell, bud, cap, initiation (stel-ate reh-tik-u-lum)
Stellate reticulum (stel-ate reh-tik-u-lum)
Stratum intermedium (stra-tum in-ter-mede-ee-um)
Succedaneous (suk-seh-dane-ee-us)
Successional dental lamina (suk-sesh-shun-al)
Supernumerary teeth (soo-per-nu-mer-air-ee)
Tooth fairy, germ (tu-ber-kls)
Tubercles (tu-ber-kls)
Tooth Development
Dental professionals must have a clear understanding of the stages of odontogenesis or tooth development and their physiological basis. Developmental disturbances can occur within each stage of odontogenesis, affecting the physiological processes taking place. These developmental disturbances can have ramifications that may affect the clinical treatment of a patient.
Development of the Dentitions
The term dentition is used to describe the natural teeth in the jaws (see Chapter 15). There are two dentitions: primary dentition and permanent dentition. A child’s primary dentition develops during the prenatal period and consists of 20 teeth, which erupt and are later shed or exfoliated (see Chapter 18). As the primary teeth are shed and the jaws grow and mature, the permanent dentition, consisting of as many as 32 teeth, gradually erupts and replaces the primary dentition (see Chapters 16 and 17). An overlapping period between the primary and permanent dentition during the preteen years is referred to as the mixed dentition period, when an individual has some teeth from both dentitions (see Figures 15-4 and 18-17).
This chapter initially focuses on the development of the primary dentition, and then its eruption and shedding. The final discussion centers on the eruption of the permanent dentition. The process of development for both dentitions is similar; only the associated time frame for each is different. The overall general dental anatomy associated with both these dentitions is discussed further in Chapter 15.
Odontogenesis takes place in stages, which occur in a stepwise fashion for both dentitions (Table 6-1). Odontogenesis is a continuous process until completed, and there is no clear-cut beginning or end point between stages. However, these stages are used to help focus on the different events in odontogenesis and are based on the appearance of the developing structures. After initiation of odontogenesis, identifiable stages in tooth development include the bud stage, the cap stage, and the bell stage. Odontogenesis then progresses to the stage of apposition with the formation of the hard dental tissue types, such as enamel, dentin, and cementum, and then finally to the stage of maturation for these structures (Table 6-2).
TABLE 6-1
| STAGE/TIME SPAN∗ | MICROSCOPIC APPEARANCE | MAIN PROCESSES INVOLVED | DESCRIPTION |
| Initiation stage/sixth to seventh week | 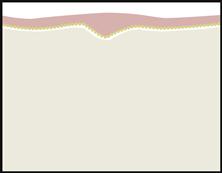 |
Induction | Ectoderm lining stomodeum gives rise to oral epithelium and then to dental lamina; adjacent to deeper ectomesenchyme, which is influenced by the neural crest cells. Both tissue types are separated by a basement membrane |
| Bud stage/eighth week | 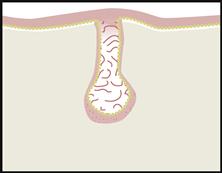 |
Proliferation | Growth of dental lamina into bud shape that penetrates growing ectomesenchyme |
| Cap stage/ninth to tenth week | 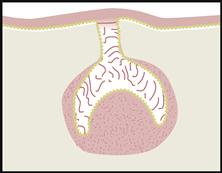 |
Proliferation, differentiation, morphogenesis | Formation of tooth germ as enamel organ forms into cap shape that surrounds inside mass of dental papilla, with an outside mass of dental sac, both from the ectomesenchyme. |
| Bell stage/eleventh to twelfth week | 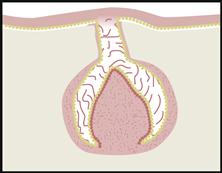 |
Proliferation, differentiation, morphogenesis | Differentiation of enamel organ into bell shape with four cell types and dental papilla into two cell types |
| Apposition stage/varies per tooth | 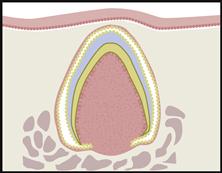 |
Induction, proliferation | Dental tissue types secreted in successive layers as matrix |
| Maturation stage/varies per tooth | 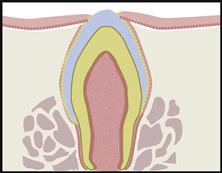 |
Maturation | Dental tissue types fully mineralize to mature form |
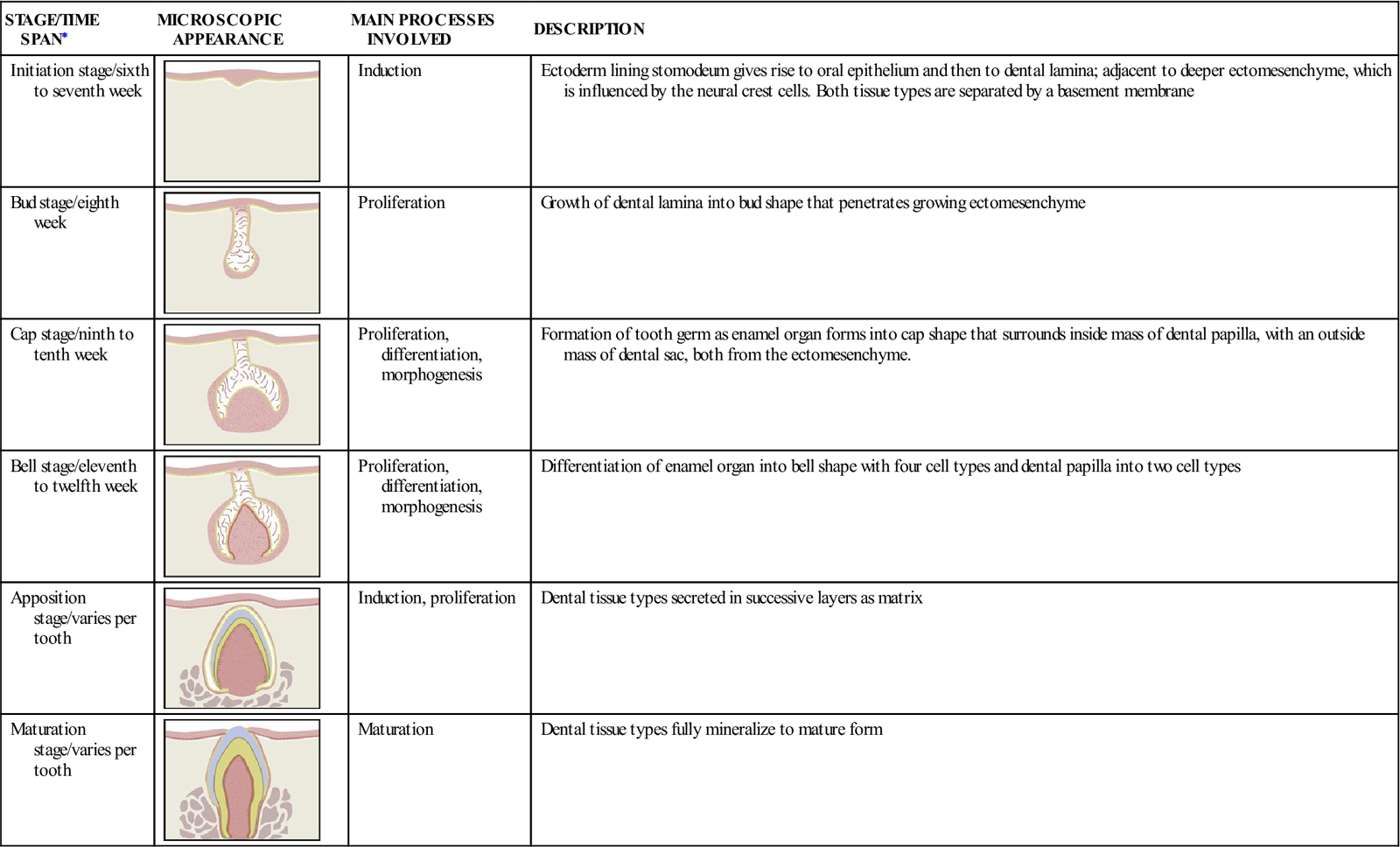
∗Note that these are approximate prenatal time spans for the development of the primary dentition.
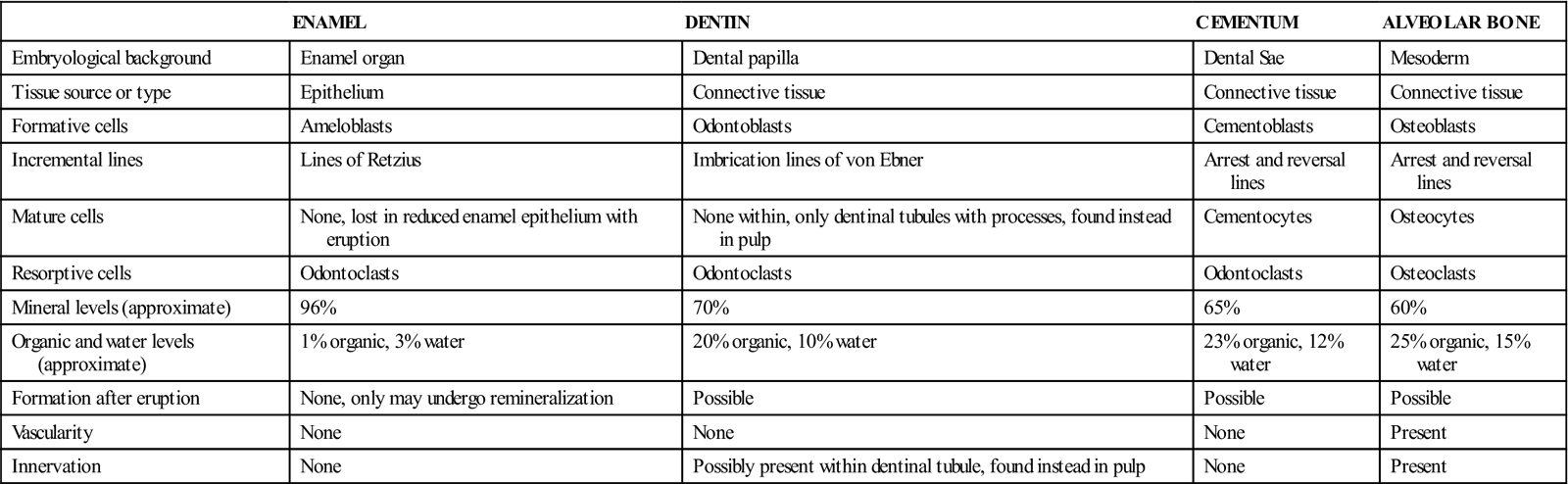
TABLE 6-2
Comparison of Dental Hard Tissue Types
| ENAMEL | DENTIN | CEMENTUM | ALVEOLAR BONE | |
| Embryological background | Enamel organ | Dental papilla | Dental Sae | Mesoderm |
| Tissue source or type | Epithelium | Connective tissue | Connective tissue | Connective tissue |
| Formative cells | Ameloblasts | Odontoblasts | Cementoblasts | Osteoblasts |
| Incremental lines | Lines of Retzius | Imbrication lines of von Ebner | Arrest and reversal lines | Arrest and reversal lines |
| Mature cells | None, lost in reduced enamel epithelium with eruption | None within, only dentinal tubules with processes, found instead in pulp | Cementocytes | Osteocytes |
| Resorptive cells | Odontoclasts | Odontoclasts | Odontoclasts | Osteoclasts |
| Mineral levels (approximate) | 96% | 70% | 65% | 60% |
| Organic and water levels (approximate) | 1% organic, 3% water | 20% organic, 10% water | 23% organic, 12% water | 25% organic, 15% water |
| Formation after eruption | None, only may undergo remineralization | Possible | Possible | Possible |
| Vascularity | None | None | None | Present |
| Innervation | None | Possibly present within dentinal tubule, found instead in pulp | None | Present |
During these stages of odontogenesis, many physiological processes occur. In many ways, these parallel the processes that occur in the formation of other embryonic structures, such as the face. These physiological processes include induction, proliferation, differentiation, morphogenesis, and maturation (see Table 3-3). Except for the induction process, many of these processes overlap and are somewhat continuous during odontogenesis. However, one individual process does tend to be predominant and mark each stage of odontogenesis.
TABLE 6-3
Common Dental Developmental Disturbances and Involved Stage
| DISTURBANCE | STAGE | DESCRIPTION | ETIOLOGICAL FACTORS | CLINICAL RAMIFICATIONS |
| Initiation stage | Absence of single or multiple teeth | Hereditary, endocrine dysfunction, systemic disease, excess radiation exposure | May cause disruption of occlusion and esthetic problems. May need partial or full dentures, bridges, and/or implants to replace teeth | |
| Initiation stage | Development of one or more extra teeth | Hereditary | Commonly found between the maxillary centrals, distal to third molars and premolar region. May cause crowding, failure of normal eruption, and disruption of occlusion | |
| Bud stage | Abnormally large or small teeth | Hereditary with partial; endocrine dysfunction with complete | Commonly affects permanent maxillary lateral incisor and third molars with partial microdontia | |
| Cap stage | Enamel organ invaginates into the dental papilla | Hereditary | Commonly affects the permanent maxillary lateral incisor. May have deep lingual pit and need endodontic therapy | |
| Cap stage | Tooth germ tries to divide | Hereditary | Large single-rooted tooth with one pulp cavity, with “twinning” in crown area. Normal number of teeth in dentition. May cause problems in appearance and spacing | |
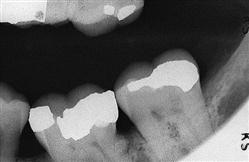
| Cap stage | Union of two adjacent tooth germs | Pressure on area | Large tooth with two pulp cavities. One fewer tooth in dentition. May cause problems in appearance and spacing | |
| Cap stage | Extra cusp from affect on enamel organ | Trauma, pressure or metabolic disease | Commonly found on permanent molars or cingulum of anterior teeth | |
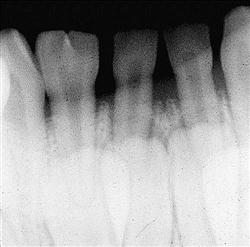
| Apposition and maturation stages | Faulty development of enamel from interference involving ameloblasts | Local or systemic; hereditary | Pitting and intrinsic color changes in enamel, with changes in thickness of enamel possible. Problems in function and esthetics | |
| Apposition and maturation stages | Union of root structure of two or more teeth by cementum | Traumatic injury or crowding of teeth | Commonly affects permanent maxillary molars. Problems with extraction | |
|
J. Enamel pearl |
Apposition and maturation stages | Sphere of enamel on root | Displacement of ameloblasts to root | May be confused as calculus deposit on root |
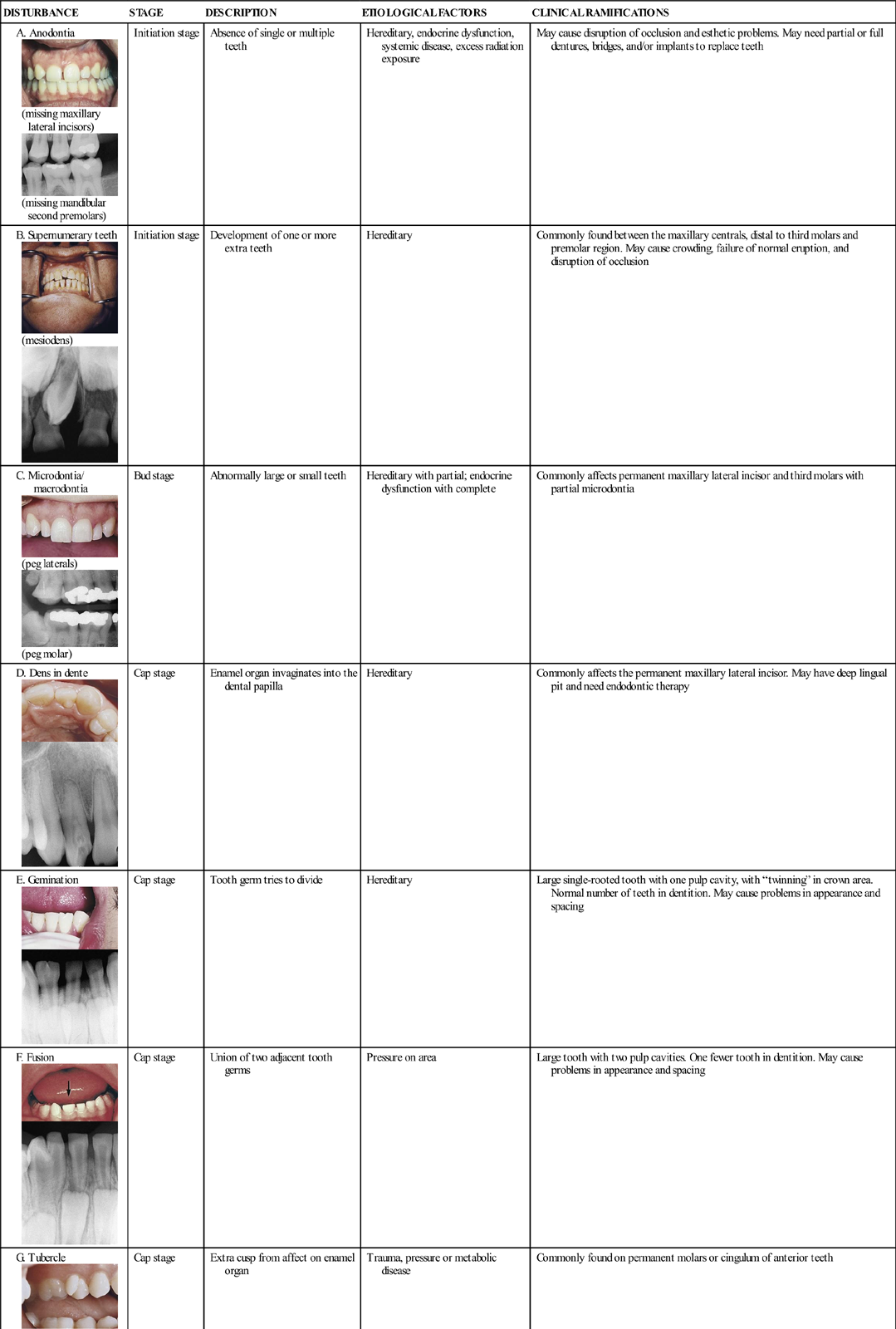
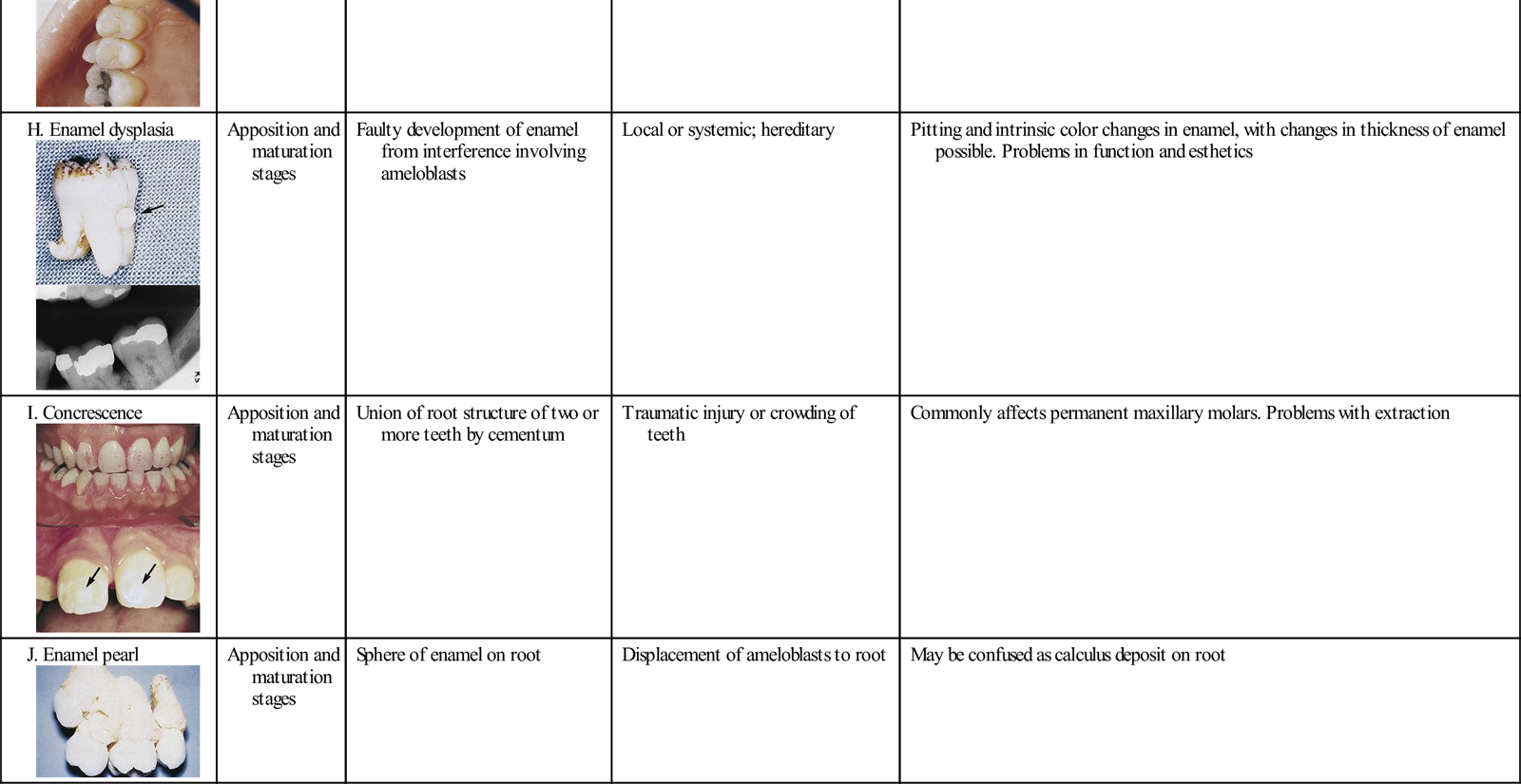
All courtesy of MJ Fehrenbach, 2011, Seattle, WA.
In the past, the study of odontogenesis included a discussion of developmental lobes that were thought to be growth centers during tooth development. These parts of the crown of the tooth are both microscopically and clinically visible by the presence of associated depressions. Whether there may be any justification for including them in a discussion of tooth formation remains controversial; developmental lobes may simply be evidence of the tooth form only, but information concerning lobes are included in this textbook for completeness.
Not all the teeth in each dentition begin to develop at the same time across each arch of the jaws. The initial teeth for both dentitions develop in the anterior mandibular region, followed later by the anterior maxillary region, and then development progresses posteriorly in both jaws. This posterior progression of odontogenesis allows time for the jaws to grow to accommodate the increased number of primary teeth, the larger primary molars, and then finally the overall larger permanent teeth.
The primary dentition develops during both the embryonic period and fetal period of prenatal development. Most of the permanent dentition is formed during the fetal period. Tooth development continues for years after birth, however, especially considering the formation of the permanent second and third molars; see Unit IV and Appendix D for tooth development timelines. Thus, teeth have the longest developmental period of any set of organs in the body.
Initiation Stage
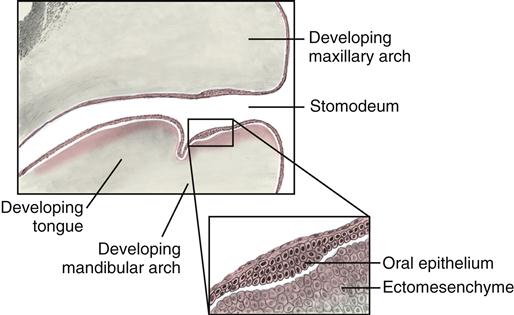
Odontogenesis of the primary dentition begins between the sixth and seventh week of prenatal development, during the embryonic period (Figure 6-1). This first stage of tooth development, known as the initiation stage, involves the physiological process of induction, which is an active interaction between the embryological tissue types. Studies show that mesenchymal tissue must influence the ectodermal tissue in order to initiate odontogenesis, but the exact mechanisms are unknown at this time.
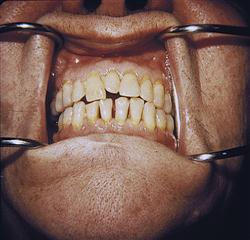
At the beginning of the sixth week, the embryo’s stomodeum, or primitive mouth, is lined by ectoderm (see Chapter 4). The outer part of the ectoderm gives rise to oral epithelium. The oral epithelium initially consists of two horseshoe-shaped bands of tissue at the surface of the stomodeum, one for each future arch or jaw. At the same time, deep to the forming oral epithelium, there is a type of mesenchyme originally from the ectoderm, ectomesenchyme, which is influenced by neural crest cells that have migrated to the area (see Figure 6-1).
An important acellular structure that separates the oral epithelium and the ectomesenchyme within the stomodeum is the basement membrane. This basement membrane is similar to the one separating all epithelium and connective tissue (see Figure 8-4).
During the later part of the seventh week, the oral epithelium grows deeper into the ectomesenchyme and is induced to produce a layer, the dental lamina (Figure 6-2). This growth occurs in the developing jaw areas where the two future curved dental arches of the primary dentition will form. The dental lamina then begins to form initially in the midline for both arches and progresses posteriorly.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses