Periodontium
Cementum, Alveolar Bone, and Periodontal Ligament
Learning Objectives
• Define and pronounce the key terms in this chapter.
• Discuss the periodontium, and describe the properties of each of its components.
• Describe the development of the periodontium.
• Outline the types of cementum and alveolar bone.
• Label the fiber groups of the periodontal ligament and discuss their functions.
• Indicate and discuss the microscopic features of the periodontium.
New Key Terms
Alveolar crest (al-vee-o-lar), group
Alveolar bone proper (al-vee-o-lar)
Alveolodental ligament (al-vee-o-lo-dent-al)
Bone: basal (bay-sal), cortical (kor-ti-kal), supporting alveolar, trabecular (trah-bek-u-lar)
Canaliculi (kan-ah-lik-u-lie)
Cemental caries (see-men-tal), spurs
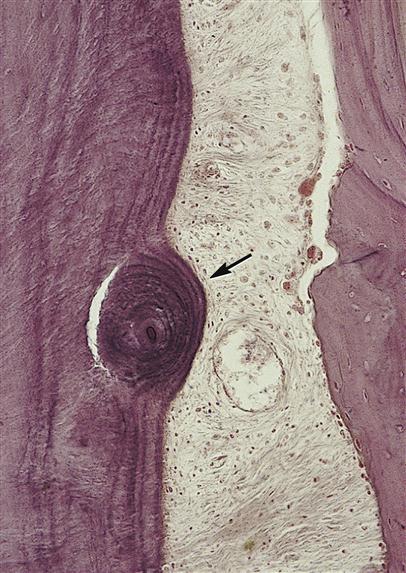
Cementicles (see-men-ti-kuls)
Cementoenamel junction (see-men-tum): acellular, cellular
Cementum (see-men-tum): acellular, cellular
Edentulous (e-den-tu-lus)
Fibers: principal, Sharpey’s (shar-peez)
Group: apical, gingival fiber (jin-ji-val), horizontal, interradicular (in-ter-rah-dik-u-lar), oblique (o-bleek)
Hypercementosis (hi-per-see-men-toe-sis)
Interdental septum, ligament (in-ter-den-tal)
Interradicular septum (in-ter-rah-dik-u-lar)
Lamina dura (lam-i-nah dur-ah)
Mesial drift (me-ze-il)
Periodontal ligament space (pare-ee-o-don-tal)
Periodontium (per-e-o-don-she-um)
Fibers: principal, Sharpey’s (shar-peez)
Periodontium
To understand the pathological changes that occur during the disease states involving the periodontium, dental professionals must first appreciate the histology of the healthy, normal periodontium. Thus, the underlying histological states of these components provide a clue to the clinical features noted visibly with the periodontium, whether in a healthy or diseased state.
Components of the Periodontium
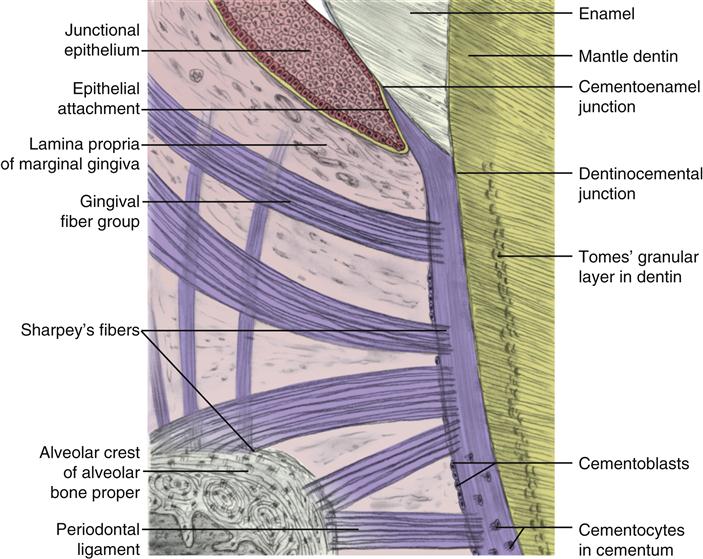
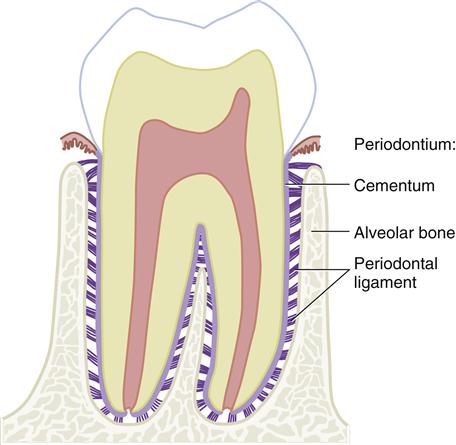
The periodontium consists of both the supporting soft and hard dental tissue between the tooth and the alveolar bone, as well as parts of the tooth and alveolar bone (Figure 14-1). The periodontium serves to support the tooth in its on-going relationship to the alveolar bone. Thus, the periodontium includes the cementum, alveolar bone, and periodontal ligament, each one’s individual components. Some clinicians may include various types of gingival tissue in the category of the periodontium, but it has only a minor role in the support of the tooth (see Chapter 10).
Cementum
The cementum is the part of the periodontium that attaches the teeth to the alveolar bone by anchoring the periodontal ligament (Figure 14-2). However, in a healthy patient, the cementum is not clinically visible because it usually covers the entire root, overlying Tomes’ granular layer in dentin, which is not usually exposed in a healthy oral cavity.
Cementum is a hard tissue that is thickest at the tooth’s apex or apices and in the interradicular areas of multirooted teeth (50 to 200 μm) and thinnest at the cementoenamel junction (CEJ) at the cervix of the tooth (10 to 50 μm). Cementum has no nerve supply and is also avascular, receiving its nutrition through its own imbedded cells from the surrounding vascular periodontal ligament. Like other the dental hard tissue of both dentin and alveolar bone, cementum can form throughout the life of the tooth (see Table 6-2), including after eruption.
Mature cementum is by weight 65% mineralized or inorganic material, 23% organic material, and 12% water. This crystalline formation of mature cementum consists of mainly calcium hydroxyapatite, with the chemical formula of Ca10(PO4)6(OH)2. The calcium hydroxyapatite found in cementum is similar to that found in higher percentages in both enamel and dentin, but more closely resembles the percentage found in bone tissue such as alveolar bone. Other forms of calcium are also present.
In certain situations, when cementum is initially exposed from gingival recession, such as occurs during periodontal disease, it is
a dull pale yellow, lighter than dentin but darker than enamel’s whitish shade (discussed later). When instruments are used, cementum feels grainy compared with the harder dentin and the even harder, smoother enamel surfaces. Because of its mineral level, cementum appears more radiolucent (or darker) than either enamel or dentin, but more radiopaque (or lighter) than pulp tissue when viewed radiographically; however, any cemental layer(s) near the CEJ may not be viewable on radiographs due to its thinness.
Development of Cementum
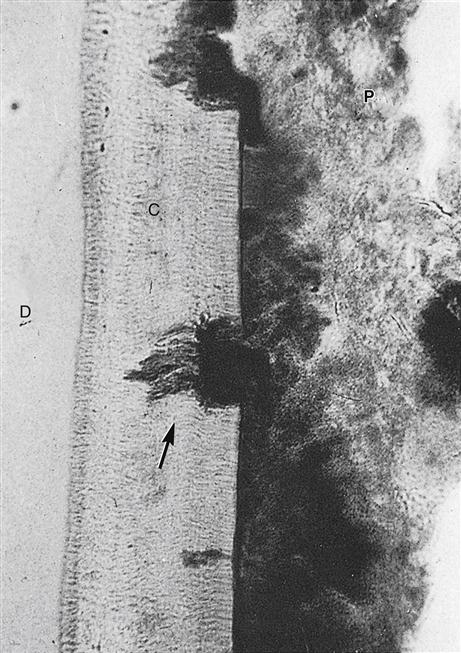
Cementum, which develops from the dental sac, forms on the root after the disintegration of Hertwig’s epithelial root sheath (see Figure 6-20). This disintegration allows the undifferentiated cells of the dental sac to come into contact with the newly formed surface of root dentin, inducing these cells to become cementoblasts. The cementoblasts then disperse to cover the root dentin area and undergo cementogenesis, laying down cementoid. Unlike ameloblasts and odontoblasts, which leave no cellular bodies in their secreted products, during the later steps within the stage of apposition, many of the cementoblasts become entrapped by the cementum they produce, becoming cementocytes (Figure 14-7). Thus again, cementum is more similar to alveolar bone, with its osteoblasts becoming entrapped osteocytes.
When the cementoid reaches the full thickness needed, the cementoid surrounding the cementocytes becomes mineralized, or matured, and is then considered cementum. Because of the apposition of cementum over the dentin, the dentinocemental junction (DCJ) is formed. This interface is not as defined, either clinically or histologically, as that of the dentinoenamel junction, given that cementum and dentin are of common embryological background, unlike that of enamel and dentin.
Microscopic Appearance of Cementum
Cementum is composed of a mineralized fibrous matrix and cells (see Figures 14-2 and 14-11). The fibrous matrix consists of both Sharpey’s fibers and intrinsic nonperiodontal fibers. Sharpey’s fibers are a part of the collagen fibers from the periodontal ligament that are each partially inserted into the outer part of the cementum at 90 degrees, or at a right angle, to the cemental surface (as well as the alveolar bone on their other end) as they are inserted on the other end, the alveolar bone. These fibers are organized to function as a ligament between the tooth and alveolar bone. The intrinsic nonperiodontal ligament fibers of the cementum are collagen fibers made by the cementoblasts and laid down in a nonorganized pattern, yet all these fibers still run parallel to the DCJ.
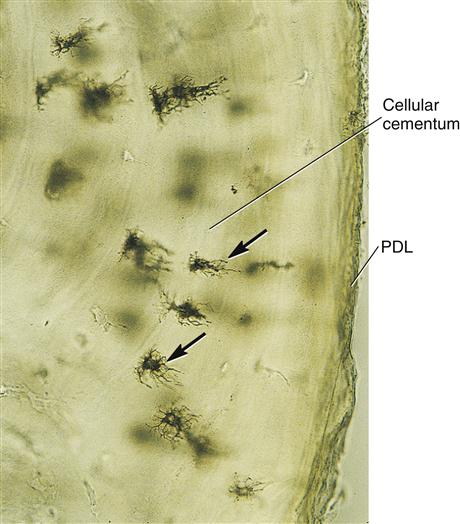
The cells of cementum are the entrapped cementoblasts, the cementocytes (see Figure 14-7). Each cementocyte lies in its lacuna (plural, lacunae), similar to the pattern noted in bone. These lacunae also have canaliculi or canals. Unlike those in bone, however, these canals in cementum do not contain nerves, nor do they radiate outward. Instead, the canals are oriented toward the periodontal ligament and contain cementocytic processes that exist to diffuse nutrients from the ligament because it is vascularized.
After the apposition of cementum in layers, the cementoblasts that do not become entrapped in cementum line up along the cemental surface along the length of the outer covering of the periodontal ligament. These cementoblasts can form subsequent layers of cementum if the tooth is injured (discussed later).
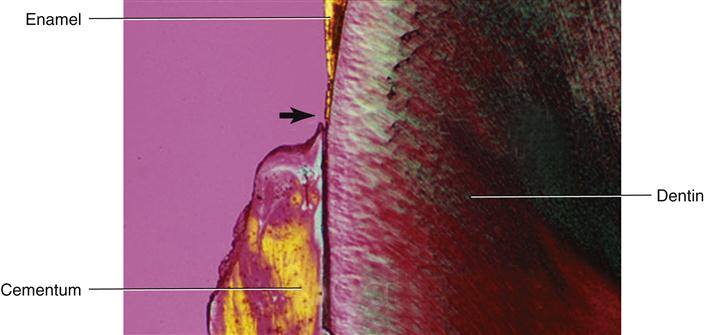
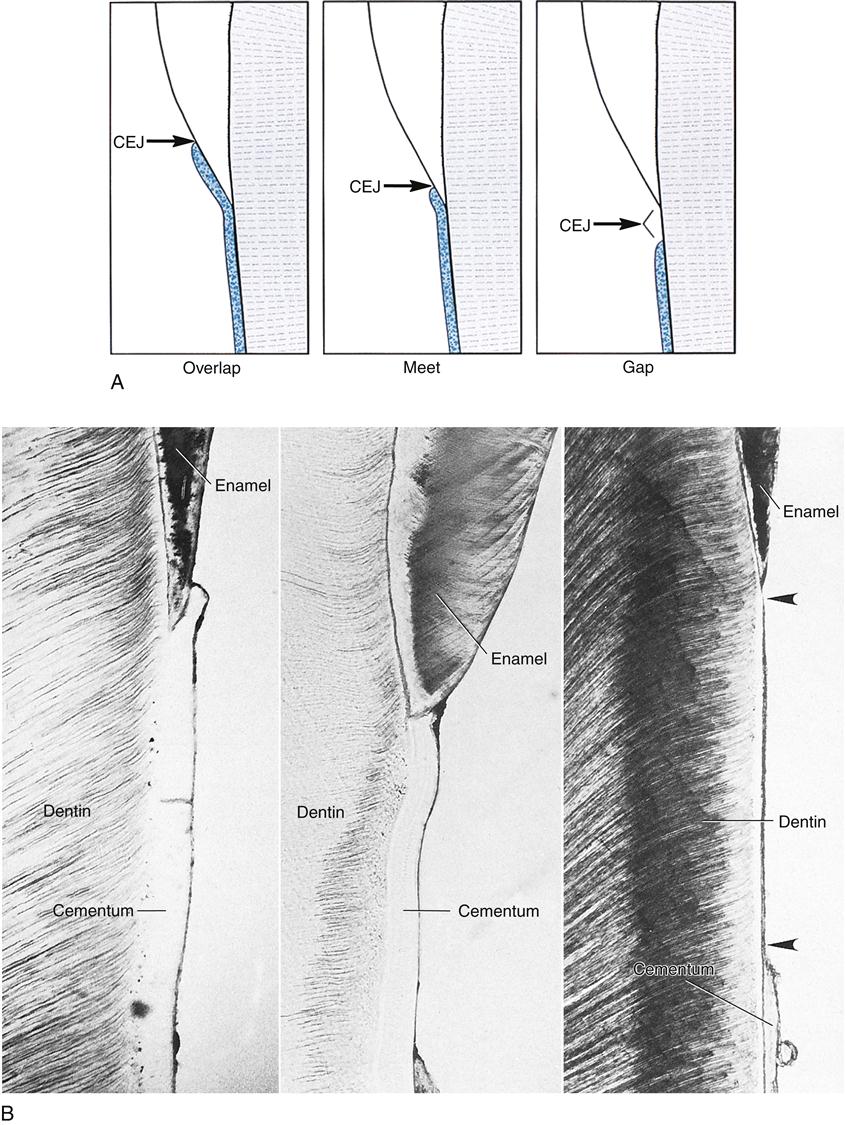
Three possible types of transitional interfaces may be present at the CEJ. The traditional view was that certain interfaces dominated in certain oral cavities. Studies with the scanning electron microscope indicate that the CEJ may exhibit all of these interfaces in an individual’s oral cavity, and there is even considerable variation when one tooth is traced circumferentially (Figure 14-8; see Figure 14-3). In some cases, the cementum may overlap the enamel at the CEJ (but thankfully fewer times than previously thought) at less than 15%. Novice clinicians may have difficulty discerning the CEJ from calculus deposits around the cervix with this situation. However, compared with the usually spotty placement and roughness of calculus, cementum exhibits a more uniform placement and roughness when using an explorer.
Another possible interface that can occur the CEJ is that the cementum and enamel may meet end to end, presenting no problems for either the clinician or patient, and it is the most common finding at about 52% of cases. Finally, another possible interface at the CEJ is that a gap may exist between the cementum and enamel, exposing dentin in about 33% of cases (see Figure 14-8). Thus, patients may experience dentinal hypersensitivity (see Figure 13-9).
Similar to bone tissue such as alveolar bone, cementum can undergo removal within the tissue as a result of trauma (Figure 14-9). This removal involves resorption of cementum by the odontoclast, resulting in reversal lines. When viewed in a stained section of cementum, these reversal lines appear as scalloped lines, just as in bone. However, cementum is less readily resorbed than bone, an important consideration during orthodontic tooth movement (discussed later).
At the same time, there can be repair of traumatic resorption area by involving the apposition of cementum by cementoblasts in the adjacent periodontal ligament. Apposition of this recently formed protective cementum is noted by layers of growth, or arrest lines, which, when viewed in a stained section, look like smooth growth rings in a section of a tree similar to what occurs in bone tissue such as alveolar bone. Both reversal and arrest lines are prominent in cementum subjected to occlusal trauma or to orthodontic tooth movement, as well as during the shedding of primary teeth and eruption of the permanent tooth. However, unlike bone, cementum does not continually undergo remodeling or repair as part of its makeup, but only when severely traumatized.
Types of Cementum
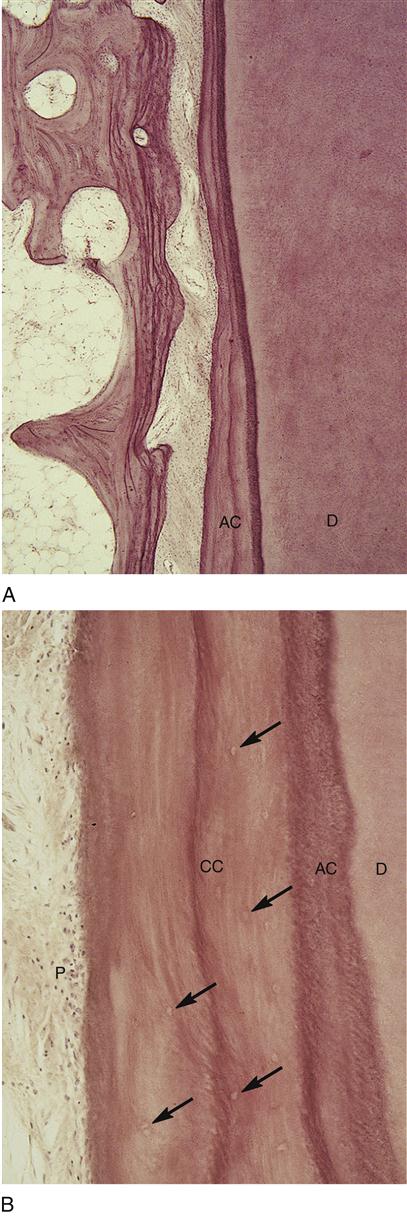
Two basic types of cementum are formed by cementoblasts: acellular and cellular (Figure 14-10 and Table 14-1). Acellular cementum consists of the first layers of cementum deposited at the DCJ, and thus is also considered primary cementum. It is formed at a slower rate than other types and contains no embedded cementocytes. At least one layer of acellular cementum covers the entire outer surface of each root with many more layers covering the cervical one third near
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses