Surgical orthodontics
People today usually recognize irregular teeth or obvious jaw deformities and seek treatment from an orthodontist, who can improve teeth alignment, function and facial aesthetics. More severe deformities that cannot be addressed with orthodontics alone will require a combination of surgical and orthodontic corrections and are called dentofacial deformities. These deformities can affect facial aesthetics and function in several ways and would require combined orthodontic and orthognathic surgical treatment.
Several factors presenting either collectively or individually may indicate the need for combined orthodontic and surgical treatment. They include impaired mastication, temporomandibular pain and dysfunction, oral respiration due to lack of lip competency, impaired speech and susceptibility to caries and periodontal disease. Although the functional impediment is important, the most common reason for patients seeking surgical correction and the most important indication of the need for orthognathic surgery are usually the psychosocial effects resulting from the unaesthetic appearance from the dentofacial deformity.
Because of rapid advances in both orthodontics and maxillofacial surgery, it is now possible to treat patients with dentofacial deformities to produce outstanding results that are aesthetically and functionally efficient. This, with the advent of modern computing skills and with the availability of more reliable video and computer imaging softwares, makes it not only possible for the surgeon and the orthodontist to interact better but also facilitates the patient to perceive the outcome of the treatment procedure, making the patient a partner in the treatment planning processes.
Ackerman and Proffit1 have further recommended that the clinician might ignore the limitations of the soft tissue in guiding the treatment planning processes.
These constraints include the pressure exerted on the teeth by the surrounding soft tissue envelope and the tongue, the temporomandibular joint including the muscles that play a major role in function and the periodontal apparatus. Superimposed on all these is the dynamic soft tissue integrity of the entire face.1
There are only three alternatives for treating patients with severe skeletal or dentofacial deformity.2
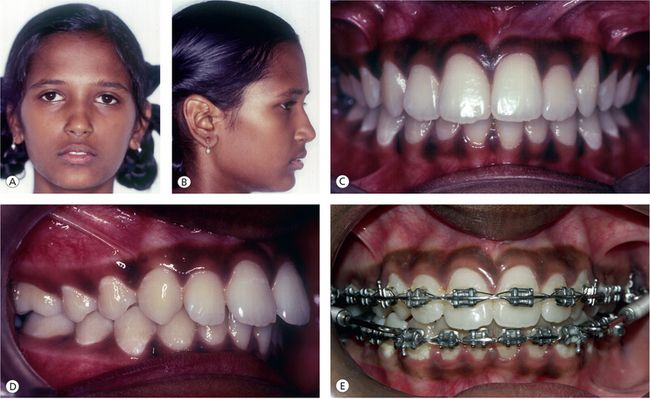

Figure 6.1 Case VP. Growth modifications in a growing child with a retrusive mandible (A and B) Pretreatment facial photograph. (C and D) Pretreatment intraoral photograph. (E and F) Fixed functional device to modify mandibular growth. (G and H) Posttreatment intraoral photograph. (I and J) Posttreatment facial photograph.

Figure 6.2 Case AR. Orthodontic camouflage treatment nongrowing patient (A) Pretreatment frontal view. (B) Profile view. (C and D) Occlusion. (E and F) The dentition was compensated to camouflage the skeletal malocclusion. (G and H) Posttreatment occlusion reveals good reduction in overjet with molars in Angle Class II and canines in Class I relationship. (I and J) Posttreatment facial view revealing good soft tissue balance despite a convex profile.
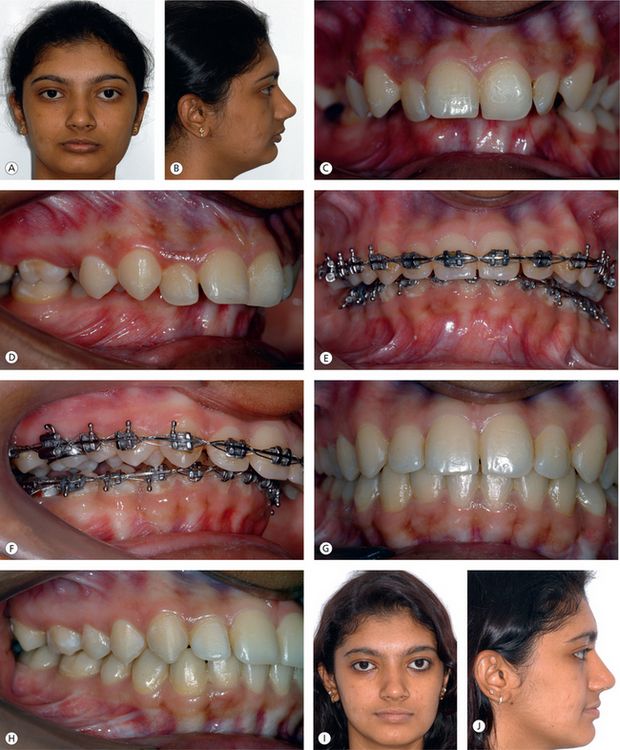
Figure 6.3 Case EN (21 years 4 months). (A and B) Facial view prior to treatment showing short vertical facial height and anteroposterior deficiency of the mandible. (C and D) Pretreatment occlusion revealing 100% deep overbite and increased overjet. (E and F) Presurgical orthodontic preparation to decompensate the dentition. (G and H) Occlusion at the completion of treatment. (I and J) Facial view at the completion of mandibular advancement surgery; note the increase in facial height, reduction in facial convexity and improvement in soft tissue balance.
While the choice between growth modification and orthognathic surgery depends upon the growth status of the individual, the choice between camouflage and combined orthodontics and orthognathic surgery depends not only on the severity of the jaw discrepancy but also on other aesthetic parameters. Ackerman and Proffit4 have enumerated some common denominators of relative dentofacial attractiveness or unattractiveness, which can be used as a guideline to decide between surgery and camouflage. These parameters include the following:
In general, patients in whom growth is completed, with a reverse overjet of greater than 3 mm, or Class II patients with an overjet of greater than 10 mm, a mandibular body length of less than 70 mm or a facial height of greater than 125 mm can be treated only by orthognathic surgery.
Diagnosis and Treatment Planning
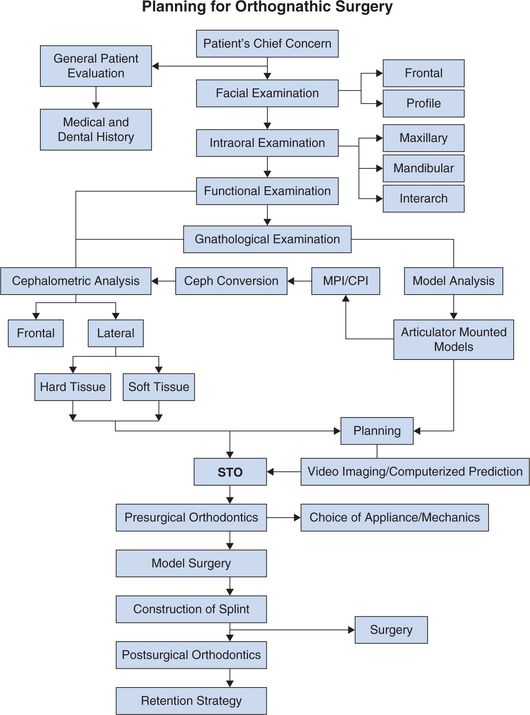
Orthognathic surgery is the art and science of diagnosis, treatment planning and execution of treatment by combining orthodontics and oral and maxillofacial surgery to correct skeletal, dental and soft tissue deformities of the jaws and associated structures. Problem-oriented diagnosis and treatment planning approach is a well-established approach in orthodontics and maxillofacial surgery and can be used in patients who are candidates for orthognathic surgery. The method involves collecting adequate information about the patient and distilling from it. The information can then be used to generate a problem list and outline the treatment strategy. The sequence of database collection and treatment planning is outlined in Table 6.1.
Patient’s chief concern
A patient’s ultimate satisfaction with treatment outcome depends on attention to the patient’s chief concern. Understanding the patient’s concern, motivations and expectations will help define treatment parameters. It will also help in identifying patients with unrealistic expectations. It is important that patients thoroughly understand all treatment options, expected outcomes and potential risks and complications. Situations in which a patient is uninformed or has unrealistic expectations often result in dissatisfaction.
General patient evaluation
Orthognathic surgery is usually performed on healthy patients. This does not, however, diminish the importance of presurgical evaluation, including medical and dental histories, physical examination and appropriate investigations.
Patient examination should rule out or identify patients with airway problems, autoimmune diseases, bleeding disorders or other pathological conditions that may complicate the surgery.
Psychological evaluation
A major reason that patients seek treatment for dentofacial problems is to overcome social handicaps resulting from an abnormal facial appearance. Most often, the motive for patients seeking treatment is due to their feeling of inadequacy and discontent that their facial appearance creates for them.
It is well recognized that physical attractiveness is associated with socially desirable characteristics. In general symmetric faces, straight profile and facial proportions that are close to the population average are considered to be attractive. Women are judged less attractive if their faces are skeletal Class III, and men are judged more negative if their faces are skeletal Class II. An individual’s response to facial appearance depends on a complex interplay of behaviours, attitudes and beliefs. Because of these strong psychosocial issues, it is imperative that the clinician makes an attempt to evaluate the psychology of the patient during the initial examination.
Facial evaluation
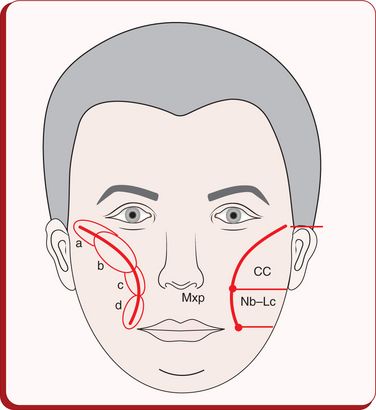
The clinical assessment of the face is probably the most valuable of all diagnostic procedures.5 Primary emphasis should be placed on frontal aesthetics, since this is how people see themselves. Balance and proportions between the various facial structures in the individual are more important than numeric values. The patient should be examined in natural head posture,6 with the teeth in centric occlusion and lips relaxed (Fig 6.4).
Frontal analysis
From the frontal view, it is particularly important to assess facial form, transverse dimensions, facial symmetry and the vertical relationship in the upper, middle and lower third of the face and the lips. Normative values for selected facial dimensions are provided in Table 6.2.
Table 6.2
Normal values for selected facial dimensions
| Parameters | Male | Female |
| Zygomatic width (zy–zy; mm) | 137 (4.3) | 130 (5.3) |
| Gonial width (go–go) | 97 (5.8) | 91 (5.9) |
| Intercanthal distance | 33 (2.7) | 32 (2.4) |
| Pupil–midfacial distance | 33 (2.0) | 32 (1.8) |
| Nasal base width | 35 (2.6) | 31 (1.9) |
| Mouth width | 53 (3.3) | 50 (3.2) |
| Face height (N–gn) | 121 (6.8) | 112 (5.2) |
| Lower face height (subnasal–gn) | 72 (6.0) | 66 (4.5) |
| Upper lip vermilion | 8.9 (1.5) | 8.4(1.3) |
| Lower lip vermilion | 10.4 (1.9) | 9.7 (1.6) |
| Nasolabial angle (degrees) | 99 (8.0) | 99 (8.7) |
| Nasofrontal angle (degrees) | 131 (8.1) | 134 (1.8) |
Facial form
The relationship between the facial width and the facial height has a strong influence on facial harmony. The height to width proportion is 1.31 for females and 1.351 for males. The bigonial width should be approximately 30% less than the bizygomatic dimension (Fig 6.5).
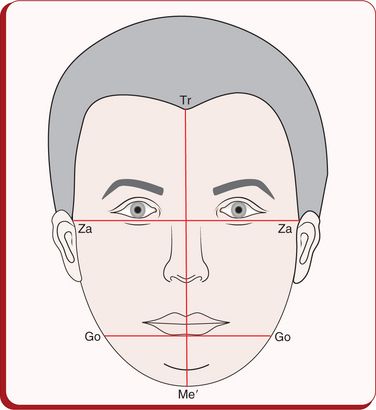
Figure 6.5 Facial form. The facial height (trichion to soft tissue menton and bizygomatic width [Za-Za]) should be 1.3:1 in females and 1.35:1 in males. Bigonial width (Go-Go) should be approximately 30% less than the bizygomatic width.
Short square facial types are often associated with a Class II deep bite malocclusion, vertical maxillary deficiency, massetric hyperplasia and macrogenia, while long narrow facial types are often associated with vertical maxillary excess, narrow nose, mandibular anteroposterior deficiency, microgenia and anterior open bite malocclusion.
Vertical dimension
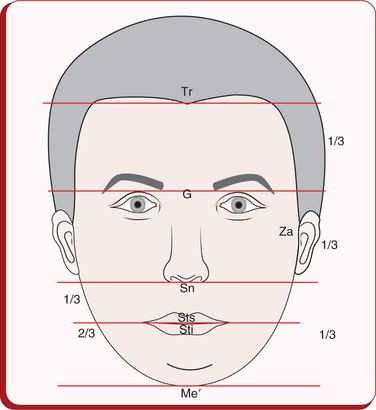
Figure 6.6 Facial third. The distance from trichion (Tr) to glabella (G), G to subnasale (Sn) and Sn to soft tissue menton (Me’) should be even. The lower third can be divided in to upper one third, from Sn to stomion superioris (Sts), and lower two thirds, from stomion inferioris (Sti) to Me’.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses