Treatment of periodontally compromised patients
Orthodontic tooth movement in periodontally involved patients constitutes a problem distinct from routine orthodontics. Orthodontic treatment is based on understanding the relationship between the orthodontic tooth movement and the different biologic processes that will take place. This chapter deals with the understanding of the health and status of the supporting structures of the teeth, the need for altered orthodontic mechanics, defining treatment goals, treatment planning and sequencing, treatment outcome and retention and stability considerations. It will also describe the role of periodontist and prosthodontist as a part of an interdisciplinary approach in the management of periodontally compromised patients.
Patients with advanced periodontal disease may experience tooth migration involving single or multiple teeth. The most common symptoms may include tipping and extrusion of one or several incisors and development of single or multiple diastemas of the anterior teeth.1 Correction of these problems demands advanced techniques and an understanding of the biologic situation present in those patients.2
Periodontal disease is not a continuous and steadily progressive degenerative process.3 Instead, it is characterized by episodes of acute attack on some but usually not all areas of the mouth, followed by quiescent periods. It is obviously important to identify high-risk patients and high-risk sites. At present, persistent bleeding on probing is the best indicator of active and presumably progressive disease. New diagnostic procedures to evaluate subgingival plaque and crevicular fluids for the presence of indicator bacteria, enzymes or other chemical mediators show promise and are likely to be clinically useful in the near future. There appear to be at least three risk groups in the population: those with rapid progression (approximately 10%), those with moderate progression (the great majority, approximately 80%) and those with no progression despite the presence of gingival inflammation (approximately 10%).4
There is no contraindication to treating adults who have had periodontal disease and bone loss, as long as the disease has been brought under control. Progression of untreated periodontal breakdown must be anticipated; however, the periodontal situation must receive major attention in planning and executing orthodontic treatment for all adults.5
The aims of this chapter are to illustrate and discuss, by means of case reports, the interrelationship of orthodontics, periodontics and prosthetic dentistry to fulfil the needs of periodontally involved patients and to highlight the benefits of the team approach.
Minimal Periodontal Involvement
Any patient undergoing orthodontic treatment must take extra care to clean the teeth, but this is even more important in adult orthodontics. Bacterial plaque is the main aetiologic factor in periodontal breakdown, and plaque-induced gingivitis is the first step in the disease process.5 Orthodontic appliances simultaneously make maintenance of oral hygiene more difficult and more important. In children and adolescents, even if gingivitis develops in response to the presence of orthodontic appliances, it almost never extends into periodontitis. This cannot be taken for granted in adults, no matter how good their initial periodontal condition is.6
A periodontal evaluation in an adult orthodontic patient must include an assessment of the level and the condition of the attached gingiva – the part of the gingiva that is tightly bound to the underlying bone. Earlier animal experiments suggested that the thickness of the gingiva, rather than its surface qualities, could be the key factor that influences the occurrence of recession.7 Proclination of incisors in some patients may be followed by thinning of the alveolar bone, leading to thinning of the attached gingiva. These patients are at higher risk for gingival recession and loss of attachment. The risk is greatest when irregular teeth are aligned by expanding the dental arch. Lower incisors in patients with a prominent chin and compensation in the form of lingual tipping of these teeth are at particular risk of recession, and thin gingival tissue probably is the reason. For adult orthodontic patients, it is much better to prevent gingival recession than to try to correct it later. Once recession begins, it can progress rapidly, especially if there is little or no keratinized attached gingiva and the attachment is only alveolar mucosa.5 Therefore, the gingival condition must receive major attention when planning the orthodontic treatment.
For the cases with abnormal gingival margins and gingival height, innovative orthodontic concepts should be used to enhance biologic structure, as well as the aesthetics of the supporting tissues. In many situations, orthodontic treatment can achieve results that could not be attained by restorations and other mean of cosmetic dentistry, especially when dealing with gingival margins and gingival height.8 In the following case report, orthodontic intervention was used to move the gingival margin of a maxillary canine incisally by almost 9 mm to mimic a lateral incisor. Increasing the thickness of the labial plate of bone of the canine and subsequently increasing the thickness of the attached gingiva before extrusion prevented gingival recession at a later stage. A step-by-step approach to achieving these treatment objectives is described.
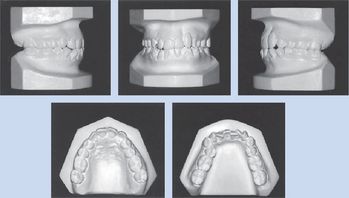
In Case 1, the attached gingiva was very thin because of the canine prominence, and the gingival margin was 9 mm higher than that of the adjacent teeth (Fig 10.1). The width of the attached gingiva was 2 mm, considerably less than that of the adjacent teeth. The width of the attached gingiva is measured as the amount of keratinized gingiva between the depth of periodontal probing and the beginning of the alveolar mucosa.9 Therefore, in planning the treatment for this patient, protective measures were taken to increase the thickness of the labial plate of bone and subsequently the thickness of the attached gingiva before extruding the canine.

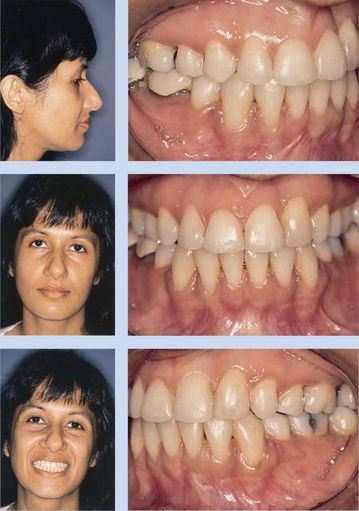
Figure 10.1 Pretreatment photos of a 34-year-old Indian woman with maxillary left canine replacing missing lateral incisor. Profile photo shows straight lateral facial profile. Intraoral photos show high gingival margin of maxillary left canine with composite buildup to mimic lateral incisor and bony depression on mesial of tooth. Figs 10.1–10.8, Reproduced with permission from Chay SH, Rabie AB. Am J Orthod Dentofacial Orthop 2002; 122:95–102.
Determining the sequence of this patient’s orthodontic treatment was based on understanding the relationship between the orthodontic tooth movement and the different biologic processes that would take place. The first step in the orthodontic treatment was palatal root torque of the maxillary left canine. As the root moved palatally, the periodontal ligament (PDL) was stretched on the labial surface, leading to bone deposition at the crest of the alveolus.9 The increase in the thickness of the labial plate of bone produced an increase in the thickness of the attached gingiva.10,11 It is believed that for some adult patients, gingival grafting before orthodontic treatment prevents gingival recession. Increasing the thickness rather than the width of the attached gingiva probably produces this protective effect. Increasing the thickness of the labial plate of bone through palatal root torque could also increase the thickness of the attached gingiva and therefore could also prevent gingival recession. Increasing the thickness of the labial plate of bone may render a healthier attachment around the tooth and ensure that both the bone and the gingiva follow the tooth during extrusion.
The application of palatal torque was made possible on the second visit, before levelling and alignment were completed. The rectangular wire was placed in the auxiliary tubes of the first molars, bypassing all teeth until it was tied to the bracket of the maxillary left canine (Fig 10.4B). Four months later, the attached gingiva looked healthier (Fig 10.4C), and the prominence of the root was less apparent. The width of the attached gingiva increased as the palatal root torque was improved. This was the indication to begin gradual extrusion of the maxillary canine. As the canine was extruded, the gingiva followed (Fig 10.4D). The composite restoration on the incisal edge was removed gradually to provide enough space for the extrusion. After the extrusion was completed, a lateral incisor bracket was placed on the maxillary left canine in an ideal position, and the root was moved mesially to reduce the bony depression. Because the root of the maxillary left canine was moved palatally, it was safe to move the root mesially. This movement was accomplished with a gable bend in the wire, and the mesial of the tooth was extruded and the distal intruded (Fig 10.4E). The patient was then referred to a dentist to restore the maxillary left canine with composite to simulate the appearance of a lateral incisor (Fig 10.4F). Again, the sequence of treatment ensured a successful result because the root of the canine was tipped mesially only after the root was moved palatally.
Therefore, if the attached gingiva appears thin and vulnerable and there is a chance of gingival recession with orthodontic tooth movement, increasing the thickness of bone through orthodontic intervention may be a way to create healthier attached gingiva before tooth movement.
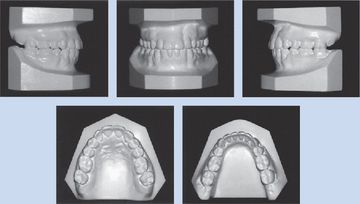
Moderate Periodontal Involvement
Before orthodontic treatment is attempted for patients who have preexisting periodontal problems, dental and periodontal disease must be brought under control. In situations where tooth movement is indicated as an adjunct to periodontal therapy, vigorous preparation of root surfaces and gingival tissues should precede placement of the orthodontic appliance.12 Deep pockets must be eliminated before orthodontic treatment is initiated so as to prevent apical displacement of plaque that could establish progressive periodontal lesions.13 Results of a longitudinal study of adults with reduced gingival height and a healthy periodontium showed that orthodontic treatment did not result in significant further loss of attachment.14 This finding depended on the prerequisite that periodontal treatment was provided to arrest active disease before orthodontic treatment was begun. Furthermore, these patients received monthly reinforcement of plaque removal and also received subgingival debridement at 3-month intervals during orthodontic treatment to maintain healthy gingival tissues.14
Disease control also requires endodontic treatment of any pulpally involved teeth. There is no contraindication to the orthodontic movement of an endodontically treated tooth, so root canal therapy before orthodontics will cause no problems. Attempting to move a pulpally involved tooth, however, is likely to cause a flare-up of the periapical condition.5
The relationship between periodontal disease and malocclusion has been a controversial subject. Tooth malpositioning has been recognized as both an aetiologic factor contributing to periodontal destruction and a result of chronic destructive periodontal disease.15 Malposed or rotated teeth may be predisposed to more rapid breakdown of the periodontium when the roots are too close to one another, resulting in a thin interproximal septum.16 Klassman and Zuckeri 17 reported that correction of these malposed teeth may be therapeutic or prophylactic. At the present time, there have been no significant studies that confirm a definite relationship between malocclusion and periodontal disease.18,19 On the contrary, the consensus of the majority of studies is that there is no relation between various types of malocclusion and periodontal diseases.15,19 In a study of 188 persons with periodontal disease, no relationship was found between periodontal disease and Angle’s classification, overbite, overjet, open bite, rotation or inclination of the mandibular incisor. Grewe et al20 reported that plaque retention based on oral hygiene habits may be the major factor in periodontal disease, while irregularities of tooth position may play another minor complicating role. The only exceptions to this appear to be extremely severe overbite, in which there is direct impingement of the teeth on the soft tissues, and localized crossbite with traumatic occlusion, which results in destructive effects on the periodontal supporting structure. Gingival recession and mobility affecting isolated mandibular incisors are not uncommon in association with lingually positioned incisors.21 In such cases, the risk of accelerated loss of attachment appears likely.21 Because traumatic occlusion may have been a predisposing factor for the gingival recession and tooth mobility, elimination of traumatic occlusion becomes a major objective of the treatment planning.
On the one hand, traumatic occlusion may contribute to destructive periodontal disease, but on the other hand, advanced periodontal disease with the loss of periodontal supporting structure can cause migration, extrusion, flaring and loss of teeth.12,22 This is because a secondary occlusal trauma may further complicate an already difficult problem. The most common symptoms may include tipping and extrusion of one or several incisors and development of single or multiple diastemas of the anterior teeth.1 Correction of these problems demands advanced techniques and an understanding of the biologic situation present in those patients.2 Melsen et al12,13 concluded that intrusion of incisors in adult patients with marginal bone loss offers a beneficial effect on the />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses